Translate this page into:
Restenosis following percutaneous transluminal coronary angioplasty among aircrew during intermediate and long term follow up
Abstract
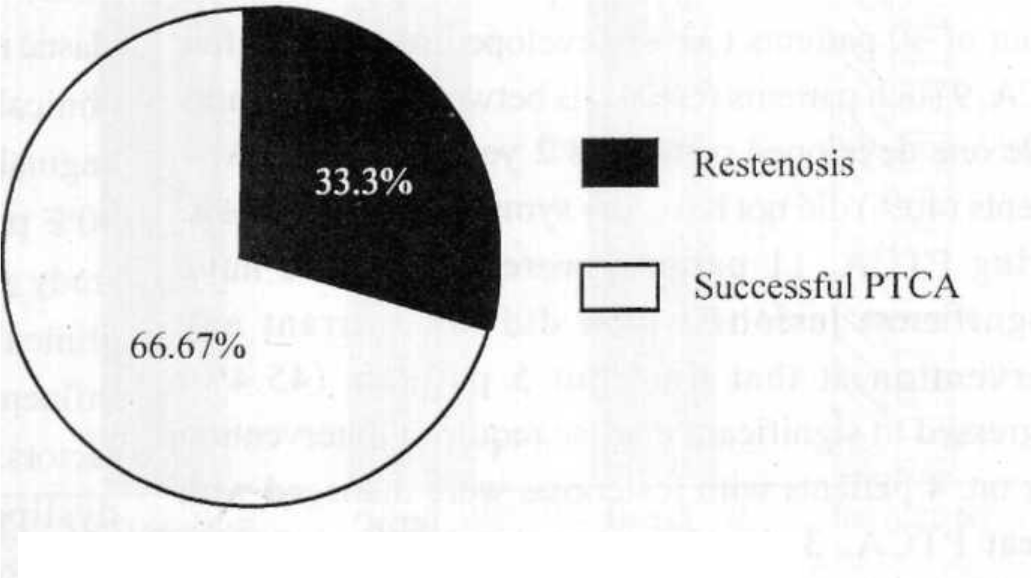
To study the incidence of restenosis following PTC A among Aircrew and analyse contributing factors for restenosis and to evaluate various methods to detect coronary restenosis. 61 Aircrew with CUD underwent cardiac evaluation before being reflighted between June 99 to October 2001,30 Aircrew who underwent PTCA, formed the basis of this study. During cardiac evaluation, all aircrew underwent clinical examination, resting ECG, echocardiography, TMT, 24 hours ambulatory ECG, SPECT stress thallium myocardial perfusion and MUGA studies after they were taken off all cardioactive drugs. A repeat coronary angiography was done between 6 to 12 months after PTCA. All were males, their age ranged from 31 to 59 years, mean age was 50.2 + 6.5 years. The follow up period after PTCA ranged from 12 months to 150 months, mean being 54.2 + 30.4 months. 22 patients (73%) had single vessel disease, 8 (27%) had multiple vessel disease (6 DVD and 2 TVD), there was no left main disease. 25 patients (83%) had normal LV function and 5 patients (17 %) had LV dysfunction, Among 30 Aircrew who underwent PTCA, a total of 38 lesions were dilated (16 in LAD, 12 in RCA and 10 in Circumflex). PTCA with stent implantation was carried out in 26 lesions, while POBA (plain old balloon angioplasty) was done in 12 lesions. 10 out of 30 patients (33.3 %), developed restenosis after PTCA. Analysis of these patients with restenosis revealed; 5 patients had Type “C” lesions, 1 had NIDDM, 3 underwent PTCA following acute coronary syndromes (2 had thrombi in the vessels to be dilated) and one had degenerated venous graft after CABGS. All these variables are associated with higher rates of restenosis. Among various methods evaluated to detect restenosis, TMT had 75 % sensitivity, and 50 % specificity and test accuracy was 57.5% SPECT Stress thallium had 75% sensitivity, 95.2% specificity and 89.4% test accuracy. Restenosis occurred in 33.3% patients after PTCA despite recent advances in hardware, technique and drugs. Appropriate patients should be chosen for PTCA in order to minimize the rate of restenosis. Out of various non-invasive methods studied, SPECT stress thallium myocardial perfusion study has the maximum predictability to detect restenosis after PTCA.
Keywords
Percutaneous Transluminal Coronary Angioplasty (PTCA)
Coronary restenosis
Coronary Heart Disease (CHD) has already assumed epidemic proportions in South Asian countries. CHD rates among Indians are two to four folds higher at all ages and five to ten folds higher under the age of forty [1-3]. A large number of these patients of CHD require revascularisation procedures (PTCA / CABGS) as definitive treatment. There has been a phenomenal growth in Interventional Cardiology procedures such as PTCA during last two decades world over including India. More than 800,000 PTCA are performed worldwide per year.
The present study has been undertaken with following objectives :
To study incidence of restenosis following PTCA among Aircrew with CHD on intermediate and long term follow up and to analyse various contributing factors for restenosis.
To compare various non-invasive methods (TMT, SPECT Stress thallium myocardial perfusion study, MUGA study, Ambulatory ECG monitoring and Echocardiography), to detect coronary restenosis.
Material and Methods
61 aircrew with CHD (confirmed by coronary angiography) underwent cardiac evaluation before being reflighted between June 1999 to Oct. 2001 (fig. 1) 30 Aircrew underwent PTCA, 12 were managed by CABGS and 19 were on medical management. 30 aircrew, who underwent PTCA, form the basis of this study. This evaluation was carried out between 6 to 12 months after PTCA.

- Management of CHD by Revascularisation Procedures
- Restenosis after PTCA
Other variables examined: Subject demographics, traditional medical risk factors and various other clinical variables were evaluated. These included age, sex, diabetes mellitus, hypertension, smoking and family history of premature CHD, presenting diagnosis, clinical interventions and left ventricle ejection fraction. Diabetes mellitus was defined as a fasting and post prandial blood sugar > 120 mg/dl and 180 mg/dl respectively, use of antidiabetic medication or a glycocelated hemoglobin > 8.0%. Hypertension was defined as a systolic blood pressure > 160 mm Hg or a diastolic blood pressure > 90 mm Hg or use of antihypertensive medication. Family history of premature CHD was considered positive if a first order relative had suffered cardiovascular death, myocardial infarction or coronary revascularisation before the age of 45 years. Tobacco use was considered present in subjects who were active smokers or had a smoking history of > 10 pack-years. Baseline fasting lipid profile was performed at index hospitalization. Only conventional risk factors parameters were assessed in this study. The clinical presentation at index hospitalization was categorized as stable angina (stable exertional symptoms only), unstable angina (progressive symptoms, or symptoms at rest), or myocardial infarction (diagnosed by WHO criteria, when at least two of the three conditions were present viz. classical history, raised enzyme levels or classical ECG changes). Clinical treatments at index hospitalization were categorized as medical therapy (only) or percutaneous transluminal angioplasty (including plain old balloon angioplasty, atherectomy and/or stenting).
During cardiac evaluation all aircrew underwent detailed physical examination for assessment of atherosclerotic occlusive disease in other vascular beds. Following investigations were carried out, after cardioactive drugs were taken off:
Resting 12 lead ECG and a 24-hour ambulatory ECG monitoring for assessment of any cardiac arrhythmia, conduction defect and silent ischaemia.
A detailed Echocardiography with Doppler study for assessment of any new regional wall motion abnormalities. Left Ventricular (LV) ejection fraction was calculated and assessment of all the valves was carried out.
Maximal symptom limited Treadmill test by Bruce protocol (usually stage 3 or more) was analysed for ST segment changes during exercise and recovery, along with other parameters like Heart rate, BP, Double product and any symptoms were noted.
SPECT Stress thallium myocardial perfusion study was performed by injecting Thallium-201 radioisotope intravenously at peak exercise. Tomographic images were reconstructed in the short axis, vertical long axis and horizontal long axis. Images were taken after four hours of test. Many perfusion defects were noted in all the vascular territories supplied by coronary arteries.
Gated SPECT MUGA test: Stress and Multigated acquisition was done with isotope 99mTc. Rest images acquired were analysed for contraction of all regions of left ventricle. Patient was made to exercise on bicycle ergo meter to achieve target heart rate and adequate double product. The stress images so acquired were analysed for contraction of all regions of left ventricle and ejection fraction was calculated. A rise of LVEF 5% from rest to exercise was considered as positive for significant CHD.
Coronary Angiographic Evaluation: Coronary angiography was evaluated by severity and extension of CHD. All patients were classified to be having significant CHD if any of the coronary artery or its major branch showed > 50% luminal diameter stenosis, while less than 50% stenosis was termed as insignificant CHD. The number of such occluded vessels (1 to 3 vessel disease) was also recorded. The Left Ventricular Ejection Fraction (LVEF) on LV angiography if 50% or more, was considered normal, and less than 50% was termed LV dysfunction. Coronary angiography was done at the time of first cardiac evaluation, it was repeated again during follow up, if their clinical condition warranted so. During repeat angiography, assessment of revascularisation treatment and any progression of the disease in native vessels was recorded.
Follow up: Those who were reflighted after initial cardiac evaluation were subjected to follow up every six months, which consisted of detailed history, physical examination and repetition of all non-invasive investigations as enumerated above. Repeat coronary angiography was done if the clinical conditions warranted so.
Comparison of Various Non Invasive Methods: A comparison was made among TMT, Echocardiography, Ambulatory ECG monitoring for 24 hrs. SPECT Stress Thallium Myocardial Perfusion study and MUGA study against Coronary Angiography results (which were taken as Gold standard), for assessment of Coronary Restenosis. Coronary Restenosis was considered to be present if luminal diameter of dilated segment of Coronary artery was < 50%. A progression of any other lesion in other coronary segments was also noted.
Results
All were males (n = 61), their age ranged from 31 to 59 years; mean age being 50.2 + 6.5 years. The follow up period after PTCA ranged from 12 months to 150 months mean being 54.06 ± 0.4 months. Average number of coronary angiography performed per Aircrew was 2.6. Four patients (13.3%) had hypertension, 6 (20%) had MI, 18 (60%) had dyslipidemia. The commonest dyslipidemia being high triglyceride levels, high LDL levels and low HDL levels. 16 (53.3%) were active smokers, 2 (6.6%) had NIDDM, while 4 (13.3%) had family history of premature CHD. 22 (73%) had single vessel disease, 8 (27%) had multiple vessel disease (6 DVD and 2 TVD). There was no left main disease. 25 patients (83%) had normal LV function and 5 patients (17%) had LV dysfunction.
Among 30 Aircrew who underwent PTCA, a total of 38 lesions were dilated (16 in LAD, 12 in RCA and 10 in Circumflex). PTCA with stent implantation was carried out in 26 lesions while POBA was performed in 12 lesions. 10 out of 30 patients (33%) developed restenosis after PTCA. 9 such patients restenosis between 5 to 7 months while one developed restenosis 2 years after PTCA. 4 patients (40%) did not have any symptoms of restenosis. During PTCA, 11 patients were detected to have insignificant lesions which did not warrant any intervention at that time but 5 patients (45.4%) progressed to significant disease requiring intervention later on. 4 patients with restenosis were managed with repeat PTCA, 3 developed restenosis and finally underwent CABGS. One was managed by rotablation followed by PTCA successfully. Ambulatory ECG monitoring for 24 hours did not reveal any ischaemic changes or any significant arrhythmia. Echocardiography revealed new regional wall motion abnormalities in only one patient of coronary restenosis. TMT and SPECT Stress thallium myocardial perfusion studies were compared against the coronary angiography findings being taken as Gold standard. TMT had 75% sensitivity, 50% specificity and test accuracy was 57.5%. SPECT Stress thallium has 75% sensitivity, 95.2% specificity and 89.4% test accuracy.
Discussion
It is well established that the long-term benefit of PTCA is compromised by the occurrence of restenosis in 21-58% of patients, with an average of 38% [5,6]. This restenosis leads to significant additional morbidity and costs related to relapses. Restenosis is the process of late arterial renarrowing at the site of an initially successful intervention. A variety of definitions have been used based on the presence and the degree of recurrent narrowing on follow up angiography (angiographic restenosis) or the occurrence of clinical events, death, non-fatal infarction or the need for repeat revascularisation during follow up (clinical restenosis). The presence of more than 50% stenosis at angiographic follow up is the most frequently used criteria for restenosis [7]. Going by this criterion our study has 33.3% restenosis rates, which are similar to published data. Earlier thought to be a simple cellular response to injury at the site of dilatation, restenosis is now recognized to be the result of multifactorial processes at both cellular and vascular level [4]. Restenosis is not an all or none phenomena but rather a process. Late loss, defined as the difference in lumen diameter after intervention and at follow up, reflects the net effect of intimal hyperplasia, elastic recoil and vascular remodeling. The most common clinical manifestation of restenosis is recurrences of anginal chest pain, MI as the first symptom is rare and 30% patients are asymptomatic as brought out by our study also. Several retrospective studies have identified clinical, anatomical and procedural factors that may influence the risk of restenosis [5, 6, 9]. Among clinical factors, presence of unstable angina, Diabetes, smoking, dyslipedemia have predicted higher incidence of restenosis. Anatomical factors, such as long lesions, saphenous vein graft disease, chronic total occlusions. Calcified ostial, bifurcation stenosis may predict higher risk of restenosis due to excessive plaque burden or excessive dilatation force required to achieve an acceptable angiographic result [8, 9]. Analysis of our patients with restenosis has revealed, NIDDM, long lesion (> 20mm). TYPE “C” lesions, acute coronary syndromes, POBA, ostial lesion and degenerated venous graft as probable causes for restenosis. Various technical improvements, pharmacological interventions, genetic manipulation and radiation therapy have been tried to prevent restenosis but only with varying success [13].
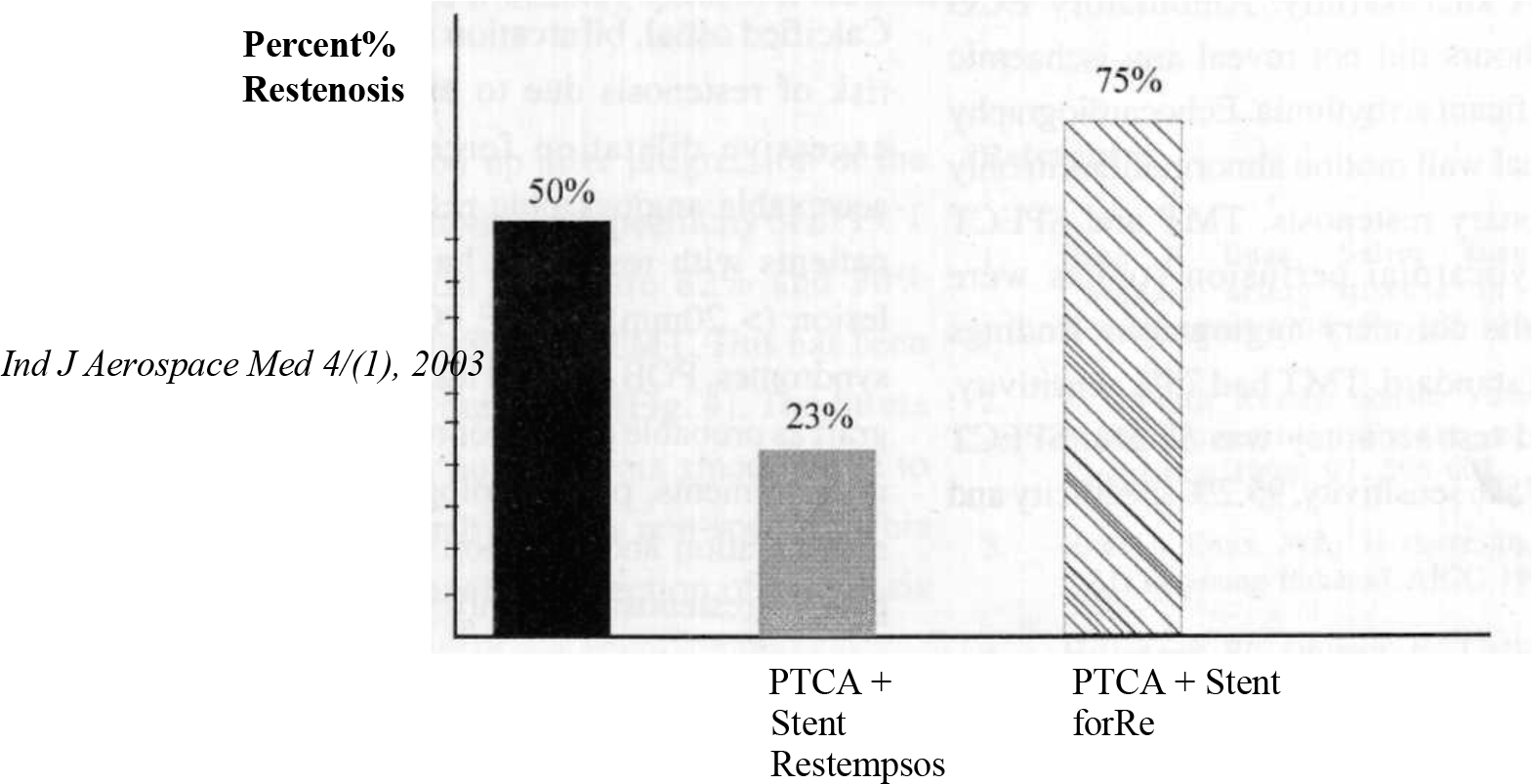
Intracoronary stents have had a dramatic impact on reduction of acute complications after PTCA and have shown reduction in clinical and angiographic restenosis.
In the Belgium and Netherlands STENT Study (BENESTENT) and in the Stent Restenosis Study, restenosis rates are significantly lower in stent groups than angioplasty groups [11, 12]. In our study restenosis rates are 50% for POBA and 23% for PTCA with stents [fig. 3]. Those undergoing repeat PTCA for restenosis have much higher rates of recurrence around 60% [10]; in our study it was 50% [fig 3]. Stress myocardial perfusion imaging is particularly useful after PTCA since its vascular territory can be evaluated for restenosis and new lesions can be picked up after progression of the disease [14-17]. The sensitivity and specificity of SPECT stress thallium perfusion study are 82% and 90% respectively while it is 50-80% for TMT. This has been very well brought out in our study. [fig.4]. The Stress MUGA study has fallen out of favors since failure to increase ejection function by >5% is non-specific. This test did not contribute much in detection of restenosis in our study.
- Restenosis after PTCA
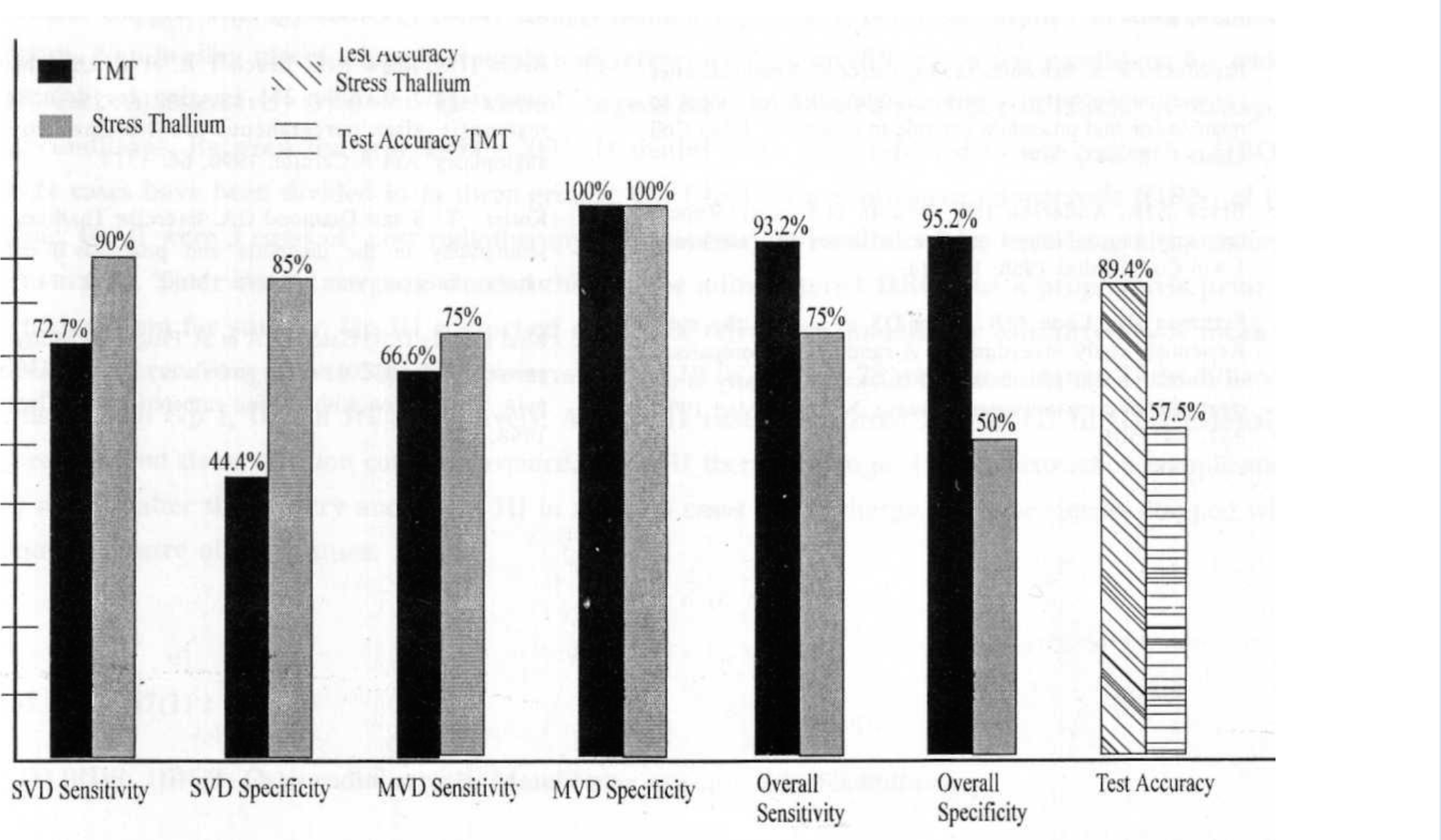
- Comparison of Sensitivity, Specifity & Test Accuracy of TMT and Stress Thallium Test for detection of Restenosis
Therefore, despite recent advances in hardware, drugs, techniques and better understanding of pathophysiology of restenosis, PTCA still gets complicated by it in almost 33.3% cases. Among various non-invasive methods available to detect coronary restenosis, SPECT stress thallium myocardial perfusion study gives the highest sensitivity and specificity to detect coronary restenosis as well as provides useful information about significant coronary artery disease in other coronary segments.
References
- Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596-601.
- [Google Scholar]
- Restenosis : the clinical issues In: Topol EJ, ed. Text book of Interventional Cardiology. Vol 2. Philadelphia, Pa: WB Saunders Co; 1994. p. :415-435.
- [Google Scholar]
- Mechanisms and prevention of restenosis : from experimental models to Clinical practice. Cardiovas Res. 1996;31:835-846.
- [Google Scholar]
- Restenosis after percutaneous transluminal coronary angioplasty (PTCA) : A report from the PTCA registry of the national heart, lung and blood institute. Am J Cardiol. 1984;53(Suppl 2):77c-81c.
- [Google Scholar]
- Resenosis after percutaneous coronary angioplasty : the Emory university hospital experience. Am J Cardiol. 1987;60:39B-43B.
- [Google Scholar]
- Resenosis after coronary angioplasty: A multivariable statistical model to relate lesion and procedure variable to restenosis. J Am Coll Cardiol. 1991;18:647.
- [Google Scholar]
- Repeat coronary angioplasty: Correlates of a second restenosis. J Am Coll Cardiol. 1988;11:714.
- [Google Scholar]
- For the stent Restenosis study investigators. A randomised comparison of coronary stent placement and balloon angioplasty in the treatment of coronary artery disease. N Engl J Med. 1994;331:491-501.
- [Google Scholar]
- for the BENESTENT study group. A comparison of balloon expandable stent implantation with balloon angioplasty in patients with coronary artery disease. N Eng L Med. 1994;331:489-495.
- [Google Scholar]
- Use of a monoclonal antibody directed against the platelet glycoprotein 116/IIIa receptor in high risk coronary angioplasty. N Eng J Med. 1994;330:956-961.
- [Google Scholar]
- Sequential thallium-201 Myocardial perfusion studies after successful percutaneous transluminal Coronary artery angioplasty : Delayed resolution of exercise induced Scintigraphic abnormalities. Circulation. 1988;77:86.
- [Google Scholar]
- Usefulness of tomographic thallium-201 imaging for detection of restenosis after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1990;66:1314.
- [Google Scholar]
- Exercise Thallium-201 scintigraphy in the diagnosis and prognosis of coronary artery disease. Ann. Intern. Med. 1990;113:684.
- [Google Scholar]
- Prognostic utility of the exercise thallium-201 test in ambulatory patients with chest pain: Comparison with cardiac catheterization. Circulation. 1998;77:745.
- [Google Scholar]






