Translate this page into:
Physical activity levels and sleep quality among military aircrew during COVID-19: A questionnaire-based pilot study

-
Received: ,
Accepted: ,
How to cite this article: Guru CS, Murtaza M, Mahajan U. Physical activity levels and sleep quality among military aircrew during COVID-19: A questionnaire-based pilot study. Indian J Aerosp Med 2023;67:8-16. doi: 10.25259/IJASM_18_2022
Abstract
Objective:
Adequate physical activities (PAs) and sleep quality are also crucial factors for maintaining optimal performance in military aircrew given the physiological demands of alien flying conditions and the occupational stress of the military lifestyle. During the COVID-19 pandemic, PA levels and sleep quality are compromised globally. Due to a lack of adequate research studies, this pilot study was aimed at assessing the PA levels and sleep quality among military aircrew during the COVID-19 pandemic.
Material and Methods:
Fifty-nine aircrew (Weight: 68.7 ± 6.45 kg and body mass index: 22.6 ± 1.76 kg/m2) of a training establishment voluntarily participated in this anonymous pen-paper pilot survey. The participants included instructors/trainee aircrew and one female aircrew. Responses for the validated International Physical Activity Questionnaire, Pittsburgh Sleep Quality Index (PSQI) questionnaire, and self-rating before the pandemic along with demographic details were collected. Data were expressed as a median and interquartile range with statistical significance set at 0.05.
Results:
About 80% of participants reported participating in games and PA regularly. Before the pandemic, 68% of aircrew did moderate-vigorous PA and >93% had average-good sleep quality. Total PA during the pandemic was 1059 (594, 1074) MET-min/week with an energy expenditure of 1226.48 (623.7, 2036.7) Kcal/week. Time spent sitting was 6 (5, 10) h/day and more than 86% of aircrew reported good global PSQI score. The effect of the pandemic was observed as significantly reduced energy expenditure, that is, 1001.25 (673.2, 1794) Kcal/week among aircrew who self-rated high levels of PA before the pandemic (P = 0.042). Aircrew who regularly played games significantly engaged in more total PA of 1547 (827, 1911) MET-min/weeks (P < 0.0001) with a significantly higher energy expenditure of 1752.7 Kcal/week (P < 0.0001).
Conclusion:
Despite pandemic restrictions, aircrew who were regularly involved in PA/games were able to maintain a better PA level. Moreover, aircrew with better sleep quality significantly engaged in higher PA levels and lesser sitting time. Sedentary behavior was assessed as sitting time increased in trainee aircrew, aircrew who were not involved in active flying, and aircrew with bad sleep quality.
Keywords
Aircrew physical activity
Sleep quality
Energy expenditure
COVID-19
Military aircrew
INTRODUCTION
Engaging in regular physical activity (PA) promotes positive health outcomes, namely, a decrease in all-cause mortality, cardiovascular disease mortality, hypertension, type-II diabetes, mental health illnesses, and an increase in cognitive health and sleep.[1,2] The World Health Organization (WHO) recommends an average adult to involve over a week in at least 150–300 min of moderate levels of PA/75– 150 min of vigorous PA.[2] Good sleep quality is essential for the recovery of body function, relieve work fatigue, and maintain sufficient energy, physical strength, and a healthy mental state as well as an important factor in the assessment of overall health and risk of cardiovascular diseases.[3] PA level and sleep quality are associated negatively in various studies.[4,5]
COVID-19 was declared, a pandemic by the WHO on March 11, 2021, and various governments across the globe announced several restrictions to curb the spread of this disease.[6] These unprecedented restrictions were found to prohibit outdoor activities as well as public gatherings including sports and fitness clubs and group PAs, thereby discouraging individuals to involve in both routine outdoor-based leisure time PA, games/sports, and fitness activities.[7] Widespread fear, anxiety, and other psychological problems affected the sleep quality of various frontline workers.[3] During COVID-19 pandemic, PA levels and sleep quality are compromised globally.[4,8] However, these two factors must be adequately maintained for a good immune function, especially against viral infections.[9,10] In addition, inadequate PA and disturbed sleep quality are both found to independently make an individual prone to develop obesity, which is suggested to be a key risk factor for poor outcomes in COVID-19 infection.[11,12]
Adequate PA and sleep quality are also crucial factors for maintaining optimal performance in military aircrew given the physiological demands of alien flying conditions and the occupational stress of the military lifestyle.[13,14] Aircrew who maintained a high level of PA reported lesser disabilities despite flying in a high-G environment and helped them maintain operational readiness.[15] The effect of COVID-19 restrictions on PA levels and sleep quality among military aircrew has not been studied. Hence, there was a felt need to study the PA levels and sleep quality among the military aircrew during the COVID-19 pandemic. This pilot study aimed at assessing the PA and sleep quality among military aircrew during COVID-19 pandemic using questionnaire based survey.
MATERIAL AND METHODS
A cross-sectional pilot survey was conducted among the aircrew of a training establishment in July 2021 after obtaining permission from the head of the institute. The aerospace medicine specialist of the center explained the participants about the study as well as instructions on filling out the questionnaire and only volunteering subjects participated in the questionnaire based survey. Participants’ identity was not included in the questionnaire to maintain the anonymity of the data and each response was given a unique ID by the investigator. The coded responses were then analyzed by the co-investigators to ensure complete anonymity and blinding. Fifty-nine aircrew (Weight: 68.7 ± 6.45 kg and body mass index [BMI]: 22.6 ± 1.76 kg/m2) participated in this pilot survey. All the volunteered participants returned the filled questionnaire with responses. The participants included instructors/trainee aircrew and one female aircrew. All aircrew who were medically fit and who were not suffering from any sleep disorders or any other ailments in the previous 7 days of the conduct of survey were included in the study.
The questionnaire included three parts namely demographic characteristics, PA level assessment, and sleep quality assessment. Demographic characteristics included were age categories, gender, weight, height, and instructor/trainee detail, flying experience in months, whether an individual was currently involved in flying, whether individual participated in sports events/games regularly in the past 2 years and whether the participant was involved in regular PA before pandemic as per the WHO guidelines.[2] The second part consisted of an assessment of PA level using validated International Physical Activity Questionnaire – Short Form (IPAQ-SF) in English with a final question of self-rating of the PA level before the pandemic in comparison to the answered questions. The final part of the questionnaire included the validated Pittsburgh Sleep Quality Index (PSQI) comprising 07 components namely subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Similar to the second part, this section also included a final question of self-rating of the PA level before the pandemic in comparison to the answered questions.
PA levels, namely, vigorous, moderate, and walking were converted into minutes per week. Total PA MET minutes as minutes/week were calculated using IPAQ short form scoring protocol.[16] One MET is the metabolic equivalent of oxygen consumption at rest. A MET-minute quantifies the oxygen consumption during the PA in METs for the given duration for doing that particular PA level.[17] The subjective sleep quality global index score, that is, the Global PSQI score comprising seven components was computed using the PSQI protocol.[18] PSQI score ≤5 was considered as good sleep and >5 was considered poor sleep.[3]
Summary statistics percentages, median, and inter-quartile range (IQR) were used to describe the PA scores, Kilocalories, and PSQI by characteristics of respondents. Shapiro–Wilk’s test was applied to test the normality of continuous variables. Mann–Whitney U test and Kruskal–Wallis test were used to study the differences in PSQI score, MET duration and Kilocalories of PA among study respondents. Chi-square and Fisher’s exact test were used to test the association factors associated with the PA and PSQI levels. Statistical significance was set at P ≤ 0.05. All the data analysis was done in Stata 12.1 (Stata Corp LP, Texas, USA).
RESULTS
A total of 59 respondents, including eight aircrew instructors and 51 aircrew trainees participated in the survey. About 78% of participants were <25 years of age. Only one female trainee aircrew participated in the study. About 90% of respondents were actively involved in flying activities currently. About 45.8% had a flying experience of <6 months and 42.4% between 6 and 18 months. About 80% of participants reported that they had been participating in games/sports events in the past 2 years. Games/sports events played included volleyball (28%), football (25%), basketball (15%), badminton (13%), cricket (9%), running (6%), tennis (2%), and hockey (2%). About 88.1% of respondents reported that they were involved in regular PAs before the COVID-19 pandemic and 57.6% of participants self-rated that they were doing a high level of PA before the pandemic as compared to during the study. About 44.2% of respondents reported good quality of sleep, while only 6.8% reported bad quality sleep before the pandemic. [Table 1] depicts the demographic characteristics and their distribution among respondents.
| Characteristics | No. of respondents, n(%) |
|---|---|
| Total respondents | 59 |
| Age (years) | |
| <25 | 46 (78.0) |
| 25–34 | 8 (13.6) |
| 35–44 | 5 (8.5) |
| Gender | |
| Male | 58 (98.3) |
| Female | 1 (1.7) |
| Body mass index (kg/m2) | |
| 18–25 | 53 (89.8) |
| 25–30 | 6 (10.2) |
| Mean±SD | 22.6±1.76 |
| Type of respondent | |
| Aircrew instructor | 8 (13.6) |
| Trainee | 51 (86.4) |
| Flying experience (months) | |
| ≤6 | 27 (45.8) |
| 7–18 | 25 (42.4) |
| >18 | 7 (11.9) |
| Mean±SD | 20.1±31.8 |
| Currently actively involved in flying activities | |
| Yes | 53 (89.8) |
| No | 6 (10.2) |
| Participated in any sports events/games last 2 years | |
| Yes | 47 (79.7) |
| No | 12 (20.3) |
| Involved in regular physical activity before pandemic | |
| Yes | 52 (88.1) |
| No | 7 (11.9) |
| Self-rated physical activities level before pandemic | |
| Low | 19 (32.2) |
| Moderate | 6 (10.2) |
| High | 34 (57.6) |
| Self-rated sleep quality before pandemic | |
| Bad | 4 (6.8) |
| Average | 30 (50.8) |
| Good | 25 (42.4) |
[Table 2] shows the comparison of PA levels, namely, vigorous, moderate, walking, or sitting in MET-duration, that is, MET minutes/week, the total PA in Kilocalories, and Global PSQI score with the demographic characteristics. Aircrew trainees were found to be engaging significantly less in moderate PA (P = 0.001) and walking (P = 0.037), thus spending 954 (480, 1674) MET minutes/week, which was significantly lower than the total PA of instructors (P = 0.013). The sitting time in instructor’s aircrew was significantly lower, that is, 3 (2, 5) h/day (P < 0.0001). Calories expenditure was also significantly higher in the instructor aircrew than in the trainee aircrew (P = 0.010).
| Variables | No. of respondents | MET (Min/week) | Sitting time (h/day) | Total PA (Kilocalories) |
Global PSQI score | |||
|---|---|---|---|---|---|---|---|---|
| Vigorous | Moderate | Walking | Total MET | |||||
| Total | 59 | 60 (0, 120) | 120 (30, 180) | 105 (70, 180) | 1059 (594, 1704) | 6 (5, 10) | 1226.48 (623.7, 2036.7) | 4 (3, 5) |
| Age (years) | ||||||||
| <25 | 46 | 53 (0, 90) | 90 (0, 135) | 105 (50, 180) | 938 (480, 1674) | 8 (6, 10) | 1000.8 (552, 1855.8) | 4 (3, 5) |
| 25–44 | 13 | 60 (0, 120) | 180 (180, 180) | 105 (90, 180) | 1547 (1017, 2274) | 4 (2, 6) | 1752.7 (1305.15, 2728.8) | 4 (3, 4) |
| P-value | 0.581 | 0.001 | 0.301 | 0.103 | 0.001 | 0.074 | 0.396 | |
| Body mass index (kg/m2) | ||||||||
| 18–25 | 53 | 60 (0, 90) | 120 (40, 180) | 105 (70, 180) | 1067 (720, 1674) | 6 (5, 10) | 1305.15 (828, 1855.8) | 4 (3, 5) |
| 25–30 | 6 | 0 (0, 180) | 60 (0, 180) | 85 (0, 180) | 521 (0, 2754) | 4 (3, 15) | 682.85 (0, 3488.4) | 4 (3, 5) |
| P-value | 0.633 | 0.516 | 0.369 | 0.383 | 0.331 | 0.531 | 0.959 | |
| Type of respondent | ||||||||
| Aircrew Instructor | 8 | 80 (15, 180) | 180 (180, 180) | 180 (135, 180) | 1954 (1166, 2754) | 3 (2, 5) | 2262.3 (1469.58, 3167.1) | 3 (2.5, 4) |
| Trainee | 51 | 60 (0, 90) | 90 (0, 180) | 105 (50, 180) | 954 (480, 1674) | 7 (6, 10) | 1000.8 (552, 1855.8) | 4 (3, 5) |
| P-value | 0.231 | 0.001 | 0.037 | 0.013 | <0.0001 | 0.010 | 0.133 | |
| Flying experience (months) | ||||||||
| ≤6 | 27 | 45 (0, 60) | 120 (60, 180) | 105 (80, 180) | 954 (827, 1547) | 6 (5, 8) | 1001.7 (922.2, 1813.5) | 4 (3, 5) |
| 7–18 | 25 | 60 (0, 180) | 60 (0, 180) | 100 (10, 180) | 923 (347, 2034) | 8 (6, 15) | 861 (358.05, 2373) | 4 (3, 5) |
| >18 | 7 | 40 (0, 180) | 180 (180, 180) | 180 (90, 180) | 1634 (1017, 2754) | 2 (2, 5) | 1795.8 (1305.15, 2845.8) | 3 (2, 4) |
| P-value | 0.297 | 0.009 | 0.163 | 0.133 | 0.002 | 0.124 | 0.188 | |
| Currently actively involved in flying activities | ||||||||
| Yes | 53 | 60 (0, 120) | 120 (60, 180) | 105 (70, 180) | 1547 (720, 1704) | 6 (4, 10) | 1667.8 (828, 2044.8) | 4 (3, 5) |
| No | 6 | 0 (0, 0) | 35 (0, 120) | 105 (50, 105) | 710 (347, 923) | 13 (8, 15) | 767.1 (358.05, 936.7) | 3 (2, 4) |
| P-value | 0.057 | 0.211 | 0.686 | 0.072 | 0.005 | 0.050 | 0.234 | |
| Participated in any sports events/games last 2 years | ||||||||
| Yes | 47 | 60 (0, 120) | 120 (60, 180) | 105 (80, 180) | 1547 (827, 1911) | 6 (5, 10) | 1752.7 (922.93, 2070.25) | 4 (3, 5) |
| No | 12 | 0 (0, 0) | 38 (0, 105) | 75 (0, 90) | 424 (47, 849) | 8 (4, 15) | 481.33 (51.15, 950.9) | 4 (3, 5) |
| P-value | <0.0001 | 0.017 | 0.006 | <0.0001 | 0.481 | <0.0001 | 0.408 | |
| Involved in regular Physical activity before pandemic | ||||||||
| Yes | 52 | 60 (0, 90) | 105 (30, 180) | 105 (55, 180) | 1038 (537, 1674) | 6 (6, 10) | 1195.69 (624.6, 1855.8) | 4 (3, 5) |
| No | 7 | 40 (10, 180) | 180 (0, 180) | 180 (90, 180) | 1634 (594, 2754) | 3 (2, 7) | 1634 (623.7, 3488.4) | 4 (3, 5) |
| P-value | 0.362 | 0.427 | 0.090 | 0.252 | 0.032 | 0.281 | 0.952 | |
| Self-rated physical activities level before pandemic | ||||||||
| Low | 19 | 60 (0, 90) | 90 (0, 180) | 100 (25, 180) | 1017 (443, 1911) | 7 (3, 10) | 1220.4 (464.63, 2070.25) | 5 (3, 5) |
| Moderate | 6 | 120 (0, 180) | 180 (180, 180) | 180 (105, 180) | 2150 (1314, 2754) | 6 (5, 6) | 2350.8 (1795.8, 2937.6) | 3 (2, 3) |
| High | 34 | 23 (0, 90) | 105 (40, 150) | 105 (60, 180) | 954 (594, 1554) | 6 (5, 10) | 1001.25 (673.2, 1794) | 4 (3, 5) |
| P-value | 0.259 | 0.010 | 0.163 | 0.069 | 0.865 | 0.042 | 0.025 | |
| Self-rated sleep quality level before pandemic | ||||||||
| Low | 4 | 53 (0, 120) | 90 (15, 180) | 143 (50, 180) | 1063 (480, 1794) | 6 (3, 10) | 1334.75 (727.05, 2150.9) | 6 (1.5, 10) |
| Moderate | 30 | 60 (0,75) | 120 (60, 180) | 105 (80, 105) | 1017 (720, 1650) | 7 (6, 10) | 1265.81 (576, 2036.7) | 4 (3, 5) |
| High | 25 | 60 (0, 120) | 120 (30, 180) | 105 (70, 180) | 1059 (594, 1704) | 6 (5, 10) | 1220.4 (828, 1855.8) | 4 (3, 5) |
| P-value | 0.849 | 0.931 | 0.215 | 0.829 | 0.085 | 0.970 | 0.785 | |
Values are expressed as Median (IQR: Inter Quartile Range). PA: Physical activity, PSQI: Pittsburgh sleep quality index, Significant P-values <0.05 are indicated in bold
Respondents with a flying experience of more than 18 months were found to significantly involve more in moderate PA (P = 0.009) and engage less in sitting activities (P = 0.002). The respondents who were actively involved in flying were found to expend much higher calories (P = 0.050) with less sitting time (P = 0.005) than those who were not currently flying. Aircrew who participated in sports events/games in the past 2 years were found significantly engaging in higher PA amounting to 1547 (827, 1911) MET minutes/week and energy expenditure of 1752.7 (922.93, 2070.25) Kcal/week (P < 0.0001).
The participants who responded that they engaged regularly in PA before the pandemic were found to be involved in longer sitting time, that is, 6 h/day (IQR = 6, 10) (P = 0.032) during the conduct of the study. Respondents who rated that they were engaged in a high level of PA before the pandemic were found to spend fewer calories, that is, 1001.25 (IQR = 673.2, 1794)/week during the study period (P = 0.042). The global PSQI score significantly differed among the respondents who rated low, moderate, or high PA before the pandemic (P = 0.025).
[Table 3] shows the comparison between PSQI components and PA levels. Respondents who reported bad subjective sleep quality were significantly spending less time in vigorous (P = 0.014) and moderate (P = 0.004) activities leading to a significantly lower total PA of 377 (93, 834) MET-minutes/week than other respondents (P = 0.010). These aircrews with bad sleep had significantly longer sitting time of 10 h/day (P = 0.026) and fewer calories expenditure of 452.4 (102.3, 1000.8) Kcal/week than the respondents with good sleep (P = 0.013). Bad sleep latency was also significantly associated with the lower duration of moderate level PA of 60 (8, 90) MET-minutes/week (P = 0.038). [Figures 1 and 2] show the global PSQI score wise total PA Kilocalories and total PA MET duration (min/week).
| Variables | No. of respondents | MET (Min/week) | Sitting time (h/day) | Total PA (Kilocalories) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vigorous | Moderate | Walking | Total MET | ||||||||||||
| Subjective sleep quality | |||||||||||||||
| Very good | 19 (32.2) | 60 (60, 180) | 180 (120, 180) | 105 (80, 180) | 1614 (1547, 2507) | 6 (4, 6) | 1760 (1634, 2634) | ||||||||
| Fairly good | 35 (59.3) | 30 (0, 90) | 90 (0, 180) | 105 (30, 180) | 954 (594, 1674) | 8 (5, 12) | 1001.7 (623.7, 1855.8) | ||||||||
| Fairly/very bad | 5 (8.5) | 0 (0, 0) | 15 (0, 60) | 90 (10, 180) | 377 (93, 834) | 10 (10, 10) | 452.4 (102.3, 1000.8) | ||||||||
| P-value | 0.014 | 0.004 | 0.832 | 0.010 | 0.026 | 0.013 | |||||||||
| Sleep latency | |||||||||||||||
| Very good | 16 (27.1) | 60 (0, 150) | 120 (30, 165) | 105 (38, 180) | 875 (537, 2394) | 8 (5, 10) | 929.8 (599.9, 2636.9) | ||||||||
| Fairly good | 31 (52.6) | 60 (0, 120) | 180 (60, 180) | 105 (70, 180) | 1547 (594, 1704) | 6 (5, 10) | 1752.7 (673.2, 1855.8) | ||||||||
| Fairly/very bad | 12 (20.3) | 5 (0, 90) | 60 (8, 90) | 180 (80, 180) | 954 (606, 1644) | 6 (4, 9) | 1001.3 (687.3, 1740.7) | ||||||||
| P-value | 0.549 | 0.038 | 0.482 | 0.801 | 0.606 | 0.715 | |||||||||
| Sleep duration | |||||||||||||||
| >7 h | 19 (32.2) | 0 (0, 120) | 120 (40, 180) | 105 (50, 180) | 954 (720, 1554) | 6 (6, 10) | 1001.7 (828, 1855.8) | ||||||||
| 6–7 h | 36 (61.0) | 60 (0, 120) | 90 (30, 180) | 105 (70, 180) | 1303 (594, 1704) | 6 (4, 10) | 1469.6 (648.5, 2044.8) | ||||||||
| 5–6 h | 4 (6.8) | 35 (5, 75) | 68 (8, 128) | 135 (50, 180) | 996 (235, 1704) | 8 (5, 12) | 1060.1 (277.4, 1730.9) | ||||||||
| P-value | 0.523 | 0.576 | 0.967 | 0.758 | 0.783 | 0.554 | |||||||||
| Habitual sleep efficiency | |||||||||||||||
| >85% | 53 (89.8) | 60 (0, 120) | 120 (30, 180) | 105 (60, 180) | 1067 (594, 1704) | 6 (5, 10) | 1305.2 (673.2, 2044.8) | ||||||||
| 75–84% | 6 (10.2) | 15 (0, 60) | 120 (0, 120) | 135 (90, 180) | 881 (594, 1614) | 6 (4, 12) | 1100 (623.7, 1667.8) | ||||||||
| P-value | 0.297 | 0.455 | 0.516 | 0.547 | 0.899 | 0.437 | |||||||||
| Sleep disturbances | |||||||||||||||
| Not during the past month | 5 (8.5) | 0 (0, 60) | 150 (90, 180) | 105 (0, 180) | 954 (720, 1067) | 6 (4, 15) | 1001.7 (828, 1226.5) | ||||||||
| Less than once a week | 49 (83) | 60 (0, 120) | 120 (30, 180) | 105 (70, 180) | 1547 (594, 1704) | 6 (5, 10) | 1752.7 (673.2, 2044.8) | ||||||||
| Once or twice a week | 5 (8.5) | 0 (0, 10) | 60 (0, 60) | 180 (105, 180) | 834 (377, 834) | 10 (5, 10) | 1000.8 (452.4, 1000.8) | ||||||||
| P-value | 0.229 | 0.243 | 0.409 | 0.431 | 0.796 | 0.389 | |||||||||
| Use of sleeping medication | |||||||||||||||
| Not during the past month | 53 (89.8) | 60 (0, 120) | 120 (40, 180) | 105 (70, 180) | 1067 (720, 1704) | 6 (4, 10) | 1305.2 (828, 2036.7) | ||||||||
| Less than once a week | 6 (10.2) | 15 (0, 60) | 75 (15, 135) | 105 (25, 180) | 635 (347, 1614) | 10 (8, 11) | 693.8 (358.1, 1667.8) | ||||||||
| P-value | 0.297 | 0.553 | 0.917 | 0.259 | 0.080 | 0.192 | |||||||||
| Daytime dysfunction | |||||||||||||||
| No problem at all | 36 (61.0) | 20 (0, 120) | 90 (0, 180) | 143 (28, 180) | 954 (480, 1854) | 7 (4, 12) | 969.1 (564, 2071.1) | ||||||||
| Only a very slight problem | 21 (35.6) | 60 (0, 90) | 120 (60, 180) | 105 (80, 105) | 1547 (827, 1650) | 6 (6, 10) | 1752.7 (979.6, 1855.8) | ||||||||
| Somewhat of a problem | 2 (3.4) | 60 (60, 60) | 158 (135, 180) | 143 (105, 180) | 1580 (1547, 1614) | 6 (5, 6) | 1761.8 (1667.8, 1855.8) | ||||||||
| P-value | 0.835 | 0.317 | 0.631 | 0.758 | 0.709 | 0.574 | |||||||||
| Global PSQI | |||||||||||||||
| Good (>5) | 51 (86.4) | 60 (0, 120) | 120 (30, 180) | 105 (60, 180) | 1066.5 (594, 1704) | 6 (5, 10) | 1305.15 (673.2, 2044.8) | ||||||||
| Poor (≤5) | 8 (13.6) | 5 (0, 75) | 60 (7.5, 90) | 142.5 (80, 180) | 834 (361.75, 1704) | 10 (4.5, 11.5) | 1000.8 (405.225, 1730.9) | ||||||||
| P-value | 0.434 | 0.065 | 0.520 | 0.425 | 0.371 | 0.308 | |||||||||
PA: Physical activity, PSQI: Pittsburgh sleep quality index, Significant P-values <0.05 are indicated in bold.

- Physical activity in Kilocalories and global PSQI score of military aircrew. PSQI: Pittsburgh sleep quality index.
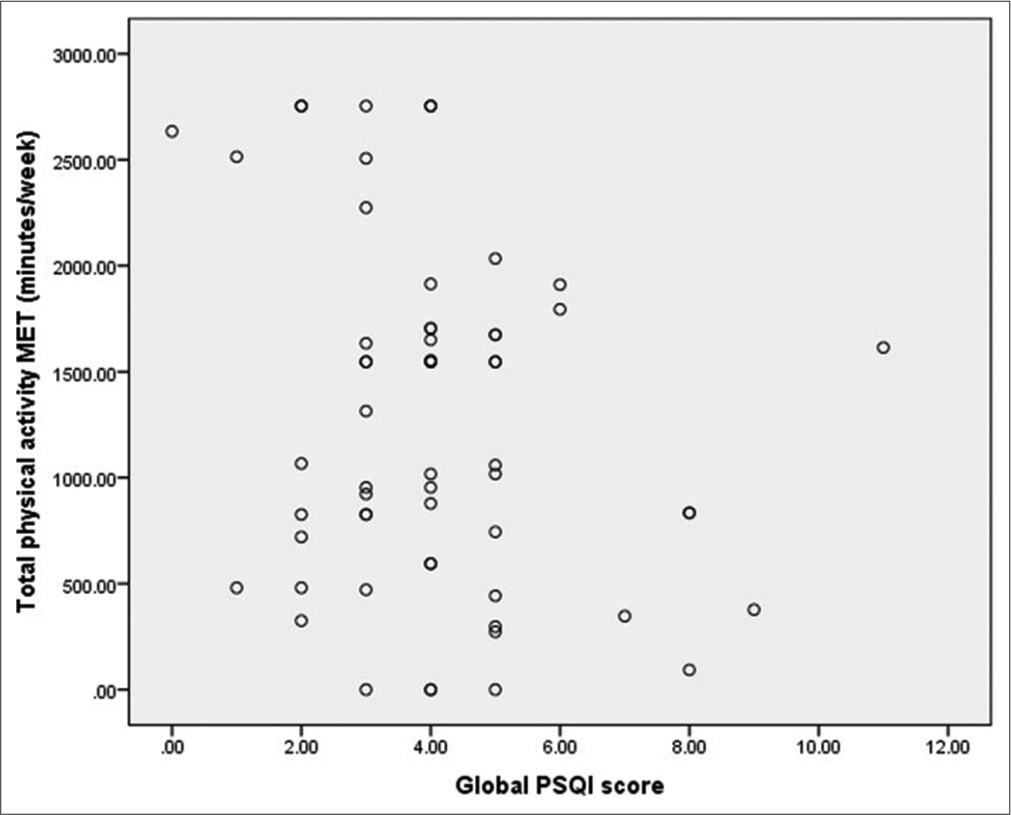
- Physical activities in MET (min/week) and global PSQI score of military aircrew. PSQI: Pittsburgh sleep quality index.
DISCUSSION
This pilot survey aimed to assess the level of PA and sleep quality among military aircrew during the COVID-19 pandemic in a fighter-training establishment. The research idea demonstrated is novel in this field, to the best of our knowledge, given the importance of both PA levels and sleep in flying performance, military operational readiness as well as in augmenting one’s immunity in the fight against COVID-19 and the lack of adequate studies in literature.
Respondents were predominantly young male trainee aircrew in the early years of their active flying career maintaining well within their accepted range for body composition, that is, BMI: 22.6 ± 1.76 kg/m2 [Table 1]. More than 80% of the aircrew were involved in either regular PA as per the WHO recommendation, that is, at least 150 min of PA in a week or engaged in sports or events before the pandemic. Self-rating of PA level as compared to the present response on PA levels and sleep quality showed that about 68% of aircrew did moderate to a high level of PA and more than 93% of aircrew had fairly good to good sleep quality before the pandemic. This indirectly depicts the knowledge, attitude, and practice of aircrew concerning the need to incorporate PA regularly for maintaining health, and fitness, and thereby enhance flying performance.
PA and sedentary behavior during COVID-19 pandemic
The total PA MET-minutes/week calculated based on the IPAQ-SF responses during the previous 07 days of the conduct of the study worked out to be 1059 (594, 1074) MET-min/week among these aircrew. This range is above the current recommended guidelines for an adult of 500–1000 MET-min/week of moderate to vigorous PA to lead a healthy and disease-free lifestyle.[19,20] Calories of energy expended by reported total PA worked out to be 1226.48 (623.7, 2036.7) Kcal/week which is again higher than the recommended weekly minimum target energy expenditure by any PA, that is, at least 1000 Kcal/week for an adult.[21-23] Total time reported to be spent sitting in a day was 6 (5, 10) h/day. Increased sedentary behavior or increased sitting time alone enhances the risk of mortality due to cardiovascular diseases manifold.[24] Although there is a lack of a cutoff to classify sitting time for adults that poses a health risk, most of the studies have found adults with sitting time in the upper quartile of 7–8 h/day as vulnerable.[25,26] However, for a healthy lifestyle, WHO has recommended that adults should limit their sitting time/sedentary behavior and replace with PA of any intensity.[2]
Analysis of the PA levels of aircrew according to their demographic characteristics showed few significant findings. Age-wise categorization as <25 years and 25–44 years showed that aircrew between 25 and 44 years significantly engaged in moderate PAs of 180 MET-minutes/week (P = 0.001), while aircrew <25 years of age significantly reported increased sitting time of 8 (6, 10) h/day than other respondents (P = 0.001). It is quite obvious that aircrew <25 years were trainee aircrew and this difference in age groups PA levels and sitting time might be due to the training syllabus which involves considerable ground training. Longer reported sitting time of 8 h/day, reduced total PA of 938 (480, 1674) MET-min/week and total energy expenditure of 1000.8 (552, 1855.8) kcal/week both below the total PA and energy expenditure of the aircrew <25 years of age indicates the need for further detailed study in a large sample of aircrew with appropriate study design. Aircrew with more than 18 months of flying experience and who are actively involved in flying reported significantly lesser sitting time as compared to the other groups.
Sleep quality during COVID-19 pandemic
We found that from the reported sleep quality analysis, the global PSQI score/sleep quality index of more than 86% of aircrew was ≤5, that is, good sleep quality during the previous 1 month of the study. It is well validated in the literature that a global PSQI score of more than five yields a diagnostic sensitivity of 89.6% and specificity of 86.5% in distinguishing between good and poor sleep quality.[18] More than 93% of aircrew reported that they slept at least 06 h in that month and out of them almost 34% slept for more than 07 h duration. About 90% of aircrew reported that they never took any sleep medication and had a habitual sleep efficiency of more than 85%. These preliminary findings demonstrate the need for further detailed objective based sleep studies in the future.
Effect of COVID-19 pandemic on PA levels and sleep quality
Aircrew who self-rated a high level of PA before the pandemic, during the conduct of study amidst pandemic had reported that they significantly engaged in walking to moderate level of PA resulting in significantly reduced energy expenditure, that is, 1001.25 (673.2, 1794) kcal/week compared to those who were engaged in low to moderate PA before pandemic (P = 0.042). Even though they were engaged in walking to moderate PAs, the reduction in vigorous PAs might be due to various restrictions during COVID-19 including workout in confined space (home), outdoor movement restrictions, prohibition of outdoor recreational/sporting activities, and closure of health and fitness centers. However, despite these restrictions, aircrew who regularly played sports events/games over the past 2 years significantly engaged in all levels of PAs with a total PA of 1547 (IQR: 827, 1911) MET-min/weeks and significantly higher energy expenditure of 1752.7 kcal/week. Thus evident that aircrew who regularly played sports/ games adapted to the constraints of the pandemic and were physically active than other groups.
In the self-rated response of sleep quality in comparison to the PSQI questionnaire before the pandemic, 6.8% of aircrew had reported that their sleep quality was bad even then. Although not significantly different from other aircrews who reported good/fairly-good sleep, the global PSQI score of this group of aircrew with bad sleep quality before pandemic was found to be 6 (1.5, 10) even during the pandemic (P = 0.785). This shows that sleep quality did not vary in these aircrew irrespective of the effects of pandemic.
PA levels and sleep interplay
Although the PA levels in comparison with PSQI global score did not vary significantly, it is evident from [Figures 1 and 2] that lower the PSQI global score higher are the expended Kcal/week and reported PA total METmin/week, respectively. However, some of the individual sleep components showed significant association when compared with PA levels [Table 3]. The subjective sleep quality component showed a significant difference with varying PA levels. Aircrew who reported fairly good to good subjective sleep quality was found to involve significantly more in a vigorous and moderate level of PA during the pandemic. Their total PA levels as well as energy expenditure were significantly higher as compared to the aircrew who reported very bad/fairly bad subjective sleep quality. These findings suggest that sleep and PA have a close relation wherein moderate to vigorous PA level promotes better sleep quality and reduced PA levels negatively affects sleep quality.[5,8,27]
In addition, it was found that a deteriorating subjective sleep quality from good quality to bad quality significantly affected the sitting/sedentary time, that is, aircrew with bad sleep spent more time sitting significantly higher than those who slept well. This finding is following the bidirectional negative influence of sleep and sedentary behavior found among adults studied by Liao .[28] Hence, it is essential to create awareness about this bidirectional association, and promote PA levels and sleep hygiene practices for optimum performance and better health outcomes, especially during the pandemic. A similar interventional approach by Wilson et al. during pandemic among commercial airline aircrew have found to positively influence all parameters of PA and sleep quality during the pandemic.[29]
It is evident from the study that a crisis situation like pandemic can reduce PA in aircrew especially in young trainees, which, in turn, can impair sleep quality. Although the study did not find any alarming sleep related issues in aircrew, it is suggested that during such crisis, supervisors should be extra vigilant to identify signs of fatigue in aircrew. The importance of pre-flight medicals cannot be overlooked and should be conducted in a befitting manner, especially during such disease pandemics. Involvement of health professionals in spreading awareness regarding the importance of PA and sleep hygiene practices should be encouraged.
CONCLUSION
PA levels have been affected by the COVID-19 pandemic among military aircrew. However, aircrew who regularly engaged in sports/games managed to involve in moderate to vigorous PA despite the restrictions. Aircrew with better sleep quality was found significantly engaging in higher PA levels and lesser sitting time. Sedentary behavior was assessed as sitting time increased in trainee aircrew, aircrew who were not involved in active flying and in aircrew with bad sleep quality.
The observed difference between the instructor aircrew and trainee aircrew as well as based on flying experience and age categorization in all the PA parameters, namely, PA levels, total PA MET-min/week, and Kcal/week as well as sitting time may not be representative due to unequal sample distribution. However, future studies might provide insight into the differences. This study being a pilot cross-sectional study of a single center military aircrew, the findings of this study cannot be generalized. Even though the validated IPAQ-SF scoring protocol adjusts the over-reported PA levels and underestimated sitting time, the limitations of recall bias and lack of matched-control groups are the limitations of this subjective survey. However, the preliminary findings of this pilot study are indicating the need to conduct detailed robust research involving a large sample of military aircrew cohort incorporating other confounders to comprehend their PA levels and sleep quality better and to plan appropriate preventive and promotive strategies if required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet. 2017;390:2643-54.
- [CrossRef] [PubMed] [Google Scholar]
- World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451-62.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of COVID-19 pandemic in the quality of sleep by Pittsburgh sleep quality index: A systematic review. Ciênc Saúde Coletiva. 2021;26:1457-66.
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity as a predictor of the level of stress and quality of sleep during COVID-19 lockdown. Int J Environ Res Public Health. 2021;18:5811.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of physical activity on sleep: A meta-analytic review. J Behav Med. 2015;38:427-49.
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity during COVID-19 induced lockdown: Recommendations. J Occup Med Toxicol. 2020;15:25.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction of physical activity levels during the COVID-19 pandemic might negatively disturb sleep pattern. Front Psychol. 2020;11:586157.
- [CrossRef] [PubMed] [Google Scholar]
- Can exercise affect immune function to increase susceptibility to infection? Exerc Immunol Rev. 2020;26:8-22.
- [Google Scholar]
- Effects of sleep and circadian rhythm on the human immune system: Sleep, rhythms, and immune functions. Ann N Y Acad Sci. 2010;1193:48-59.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis. Obes Rev. 2020;21:e13095.
- [CrossRef] [PubMed] [Google Scholar]
- Association of timing and balance of physical activity and rest/sleep With risk of COVID-19: A UK biobank study. Mayo Clin Proc. 2021;96:156-64.
- [CrossRef] [PubMed] [Google Scholar]
- A survey of the sleep status among military pilots. Med J Chin Peoples Lib Army. 2012;37:141-5.
- [Google Scholar]
- Investigation and analysis of sleep quality and occupational stress among military pilots. Chin J Convales Med. 2015;11:1214-16.
- [Google Scholar]
- Relationships between physical fitness, demands of flight duty, and musculoskeletal symptoms among military pilots. Mil Med. 2015;180:1233-8.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.sites.google.com/site/theipaq/scoring-protocol [Last accessed on 2021 Aug 07]
- ACSM's Guidelines for Exercise Testing and Prescription (10th ed). Netherlands: Wolter Kluwer; 2018.
- [Google Scholar]
- The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur Heart J. 2019;40:3547-55.
- [CrossRef] [PubMed] [Google Scholar]
- Meeting USDHHS physical activity guidelines and health outcomes. Int J Exerc Sci. 2017;10:121-7.
- [Google Scholar]
- Physical activity and all-cause mortality: What is the dose-response relation? Med Sci Sports Exerc. 2001;33:S459-471. discussion S493-4
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity recommendations and decreased risk of mortality. Arch Intern Med. 2007;167:2453-60.
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity, health benefits, and mortality risk. ISRN Cardiol. 2012;2012:718789.
- [CrossRef] [PubMed] [Google Scholar]
- Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019;73:2062-72.
- [CrossRef] [PubMed] [Google Scholar]
- Physical inactivity and sitting time prevalence and trends in Mexican adults. Results from three national surveys. PLoS One. 2021;16:e0253137.
- [CrossRef] [PubMed] [Google Scholar]
- Joint prevalence of sitting time and leisure-time physical activity among US adults, 2015-2016. JAMA. 2018;320:2036-8.
- [CrossRef] [PubMed] [Google Scholar]
- Increased physical activity improves sleep and mood outcomes in inactive people with insomnia: A randomized controlled trial. J Sleep Res. 2015;24:526-34.
- [CrossRef] [PubMed] [Google Scholar]
- Investigating the within-person relationships between activity levels and sleep duration using Fitbit data. Transl Behav Med. 2021;11:619-24.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of a 17-week lifestyle intervention on health behaviors among airline pilots during COVID-19. J Sport Health Sci. 2021;10:333-40.
- [CrossRef] [PubMed] [Google Scholar]







