Translate this page into:
Cumulative sleep restriction and subsequent recovery sleep: Effects on subjective sleepiness, vigilance, and executive functions

*Corresponding author: Swapnil Mishra, Flight Surgeon, 37 (I) R&O Flight (Army Aviation), Ladakh, India. yuvrajswapnil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mishra S, Tripathy NK, Biswal P, Raghunandan V. Cumulative sleep restriction and subsequent recovery sleep: Effects on subjective sleepiness, vigilance, and executive functions. Indian J Aerosp Med 2023;67:22-7. doi: 10.25259/IJASM_14_2022
Abstract
Objective:
Cumulative partial sleep loss is more often practical eventually among aircrew. The sleep loss encountered on the weekdays is generally compensated by taking restorative sleep on the weekends. This study aimed to examine the subjective appreciation of sleepiness and cognitive performance pertaining to vigilance and executive functions during cumulative sleep restriction for a period of 05 days and then following 3 consecutive nights of recovery sleep.
Material and Methods:
In a repeated measures design, 14 healthy volunteers were longitudinally followed up twice on a day (morning and afternoon) on their subjective sleepiness (Stanford Sleepiness Scale), vigilance, and executive functions (Mackworth Clock Test and Stroop Test of Psychometric Evaluation Design for Aviators test battery, respectively) over a period of 5 days with 2 h of sleep restriction each night. These parameters were again assessed following 3 consecutive nights of restorative recovery sleep.
Results:
Subjective appreciation of sleepiness was significantly increased by accumulating sleep debt (F = 8.368, P < 0.001). Stroop Effect and Reaction Time did not show any significant changes; however, cumulative sleep loss significantly affected accuracy measures (F = 2.388, P = 0.04) and attention lapses (F = 2.816, P = 0.018). Following restorative sleep, the subjective sleepiness and accuracy scores did not show any significant difference from that of baseline. However, lapses continued to be significantly higher than the baseline values (P = 0.012).
Conclusion:
Cumulative sleep loss over a period of 5 days resulted in more sleepiness and a decrement in vigilance measures even though the executive functions remained intact. The persistence of attention lapses indicated incomplete recovery of vigilance functions following 3 days of restorative sleep.
Keywords
Cumulative sleep restriction
Recovery sleep
Sleepiness
Vigilance
Executive functions
INTRODUCTION
Sleep loss and resultant fatigue is a potential flight safety issue in aviation operations both military and civil.[1] Studies have shown that fatigue has contributed to approximately 20% of aviation accidents.[2] Among the various effects of sleep deprivation, the effects on psychomotor cognitive domains can have significant implications in aircrew performance and hence, disastrous consequences in highly demanding occupations like aviation.[2] Sleep loss in aircrew can be acute or chronic. Acute sleep loss is when sleep obtained in 24-h period is less than the physiologically required amount or habitual total.[3] In contrast, partial sleep loss amounts to when some amount of night’s sleep is lost as per the desired sleep requirement. When partial sleep loss is obtained repeatedly on consecutive occasions, it is called chronic or cumulative sleep loss.[4]
The effects of acute sleep loss on aircrew performance have been studied extensively.[5-7] However, studies on cumulative sleep restriction are scant, specifically in the Indian Air Force. The effects of cumulative sleep restriction are as severe as acute sleep loss of a complete single night’s sleep. A study on cumulative sleep loss has indicated significant effects on waking neuro-behavioral functions which tend to accumulate in a dose response manner.[3] In another study, increasing sleep debt was found to increase daytime sleep pressure indicated by the assessment of multiple sleep latency tests and maintenance of wakefulness tests.[8] Chronic sleep restriction has also been reported to affect vigilance[9] and memory.[10] Studies have also used the subjective perception of sleepiness and quality of sleep as measures of sleep deprivation.[11,12] The effects of recovery of cognitive functions have also been studied on restorative sleep following decrement due to cumulative sleep loss.[13]
In aviation operations, chronic partial sleep loss is more often a practical eventuality than total sleep deprivation. The sleep debt encountered on the weekdays is generally restored by taking recovery sleep on the weekends. It is thus important to look for specific psychomotor cognitive measures which are likely to change under these naturalistic situations in which the aircrew operates. Examination of changes in daytime sleepiness, cognitive performance pertaining to vigilance, and executive functions over a period of 5 days of cumulative sleep restriction and subsequent recovery following 3 consecutive nights of restorative sleep were the desired objective of the study.
MATERIAL AND METHODS
Subjects
Fourteen healthy volunteers (four females and ten male) between 25 and 38 years of age (31.4 ± 4.53 years) participated in the study. The presence of history of sleep disorder, head injury, psychiatric and neurological abnormalities, obesity, drug intake, and extremes of morningness/eveningness chronotypes (assessed by Owl and Lark questionnaire) were excluded from the study.
Materials
Stanford sleepiness scale (SSS)
SSS was used to assess daytime sleepiness. It is a quick, easy, and self-administered questionnaire having a 7-point Likert scale rating with seven being the sleepiest and 1 being the most alert. The SSS measures how alert a person is at that moment in time. Possible scores range from 1 (“Feel active and vital; alert, wide awake) to 7 (“Almost in reverie; sleep onset soon; lost struggle to remain awake”).
Psychomotor cognitive performance tasks
A psychometric evaluation design for aviators (pSuMEDhA), designed indigenously at the Institute of Aerospace Medicine, is a laptop-based psychomotor cognitive test battery. The two tests of pSuMEDhA used in the present study were Mackworth Clock Test and Stroop Test. Mackworth Clock Test is a 15 min vigilance task where the subject is shown a clock with a rotating dot. The subject has to hit the spacebar when the dot misses the clock while rotating. The test gives reaction time, correct clicks (accuracy), and missed clicks (lapses). Stroop Test is a 5 min task consisting of two phases of 2½ min each. Word Red, blue, green, and yellow are displayed on the screen in these four different colors which. The meaning of the color and font color are not necessarily the same. In the first phase, the subject has to click the named color out of the four colors displayed on the screen. In the second phase, the subject has to click the color of the word which conveys the color in its meaning as well. The second phase indicates suppression of learned response which is quantified as a difference in reaction time between Phase 2 and Phase 1. This is termed as Stroop effect and is a measure of executive functions.
Study protocol
The experimentation was designed as a longitudinal repetitive measure design. The protocol was approved by the Institute Ethics Committee. All the participants were briefed on the study protocol and written informed consent was taken. For each participant, the experiment lasted for a total of 14.5 days and involved three phases. In the preparatory phase, the time to bed and the wake up time of the subjects were established. The subjects were given practice sessions so that the subjects get used to the test administration, and also to allow the practice and learning effects to normalize. The baseline values were recorded for subjective sleepiness (SSS) and cognitive performance measures (Stroop Test and Mackworth Clock Test) at 0900–0930 h (morning) and again at 1500–1530 h (afternoon–post lunch circadian effect). This was followed by the sleep restriction phase (D1, D2, D3, D4, and D5), in which the time to bed of subjects was delayed by 2 h; while keeping time to wake up the same as in the previous week, thereby subjecting them to 2 h of partial sleep restriction daily. Since the subjects continued to have 2 h of restricted sleep consecutively for five nights, it amounted to a total of 10 h of cumulative sleep restriction over a period of 5 days. On each day, the subjects were assessed twice; once in the morning (0900–0930 h) and once in the afternoon (1500–1530 h) on the subjective sleepiness and cognitive performance measures. Following this, subjects were advised to have 3 nights of restorative recovery sleep, akin to the rest period after a routine work week of an aircrew, which constituted the recovery phase. Assessments were again repeated in the morning and after hours on Monday to see the effects of recovery sleep on the test parameters.
Statistical analysis
Statistical analysis was done using IBM SPSS software, version 20. Two Factor Univariate General Linear Model was applied to each of the dependent variables. Significant F statistics with post hoc analysis was carried out using Tukey’s HSD between the days of sleep restriction and recovery.
RESULTS
Subjective sleepiness (SSS scores)
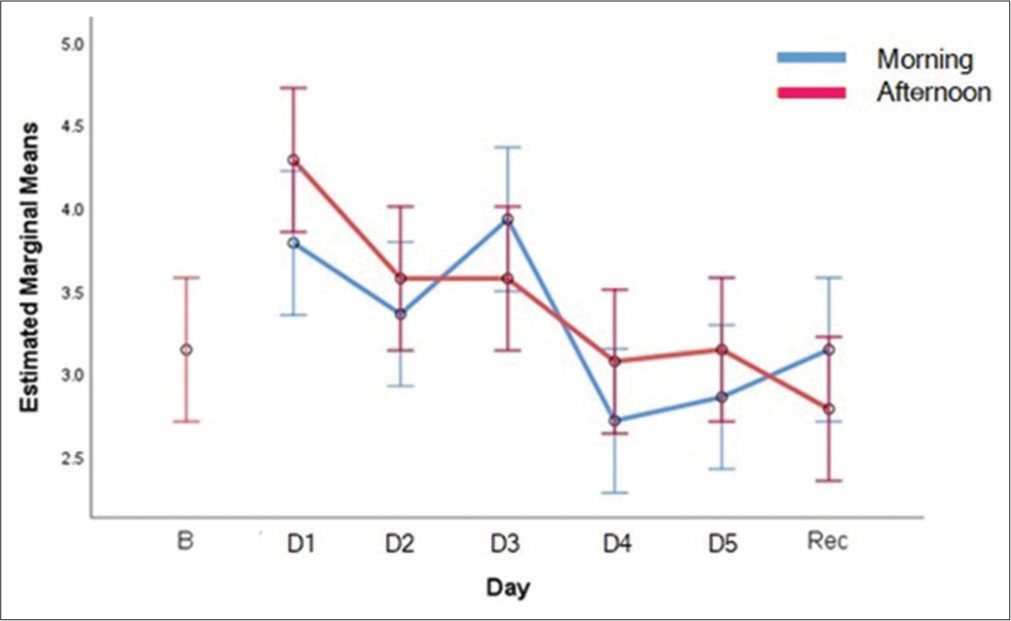
There was a statistically significant difference in the subjective perception of sleepiness across the days (F(6,169) = 3.539, P = 0.004) and time of the day (F(1,169)= 7.094, P = 0.008). However, no interaction effect was seen between day of study and time of the day. Trend of SSS is shown in [Figure 1] and Tukey’s post hoc analysis in [Table 1]. It can be observed that there is no significant difference (P = 0.252) in the subjective sleepiness between baseline and following recovery sleep.

- Means of Stanford sleepiness scale scores with sleep restriction and recovery sleep.
| Day | Baseline | D1 | D2 | D3 | D4 | D5 | Recovery |
|---|---|---|---|---|---|---|---|
| Baseline | - | 0.252 | 0.008 | 0.008 | 0.000 | 0.000 | 0.252 |
| D1 | 0.252 | - | 0.868 | 0.868 | 0.311 | 0.036 | 1.00 |
| D2 | 0.008 | 0.868 | - | 1.00 | 0.969 | 0.525 | 0.868 |
| D3 | 0.008 | 0.868 | 1.00 | - | 0.969 | 0.525 | 0.311 |
| D4 | 0.000 | 0.311 | 0.969 | 0.969 | - | 0.969 | 0.311 |
| D5 | 0.000 | 0.036 | 0.525 | 0.969 | 0.969 | - | 0.036 |
| Recovery | 0.252 | 1.00 | 0.868 | 0.311 | 0.311 | 0.036 | - |
SSS: Stanford sleepiness scale
Vigilance function
There was no statistically significant difference in the reaction time across the days (F(5,169) = 0.971, P = 0.437) or between times of the day (F(5,169) = 0.181, P = 0.671). Accuracy Scores as measured by correct clicks on Mackworth clock test showed a statistically significant decrement across the sleep restriction periods (F(5,169)=2.388, P = 0.04). However, no significant difference was observed between the time of the day (F(1,169) = 0.183, P = 0.669) or any interaction effect (F(5,169) = 0.367, P = 0.870). The trend of correct responses is depicted in [Figure 2]. Post hoc analysis revealed that the D3 scores were significantly different than D4 (P = 0.032) and D5 (P = 0.053). Furthermore, D4 values were significantly different from D1 values. No significant difference was observed between the baseline values and that following recovery sleep [Table 2]. Lapses as measured by missed clicks on Mackworth Clock test were found to be significantly higher with sleep restriction (F(5,169) = 2.816, P = 0.018). No significant difference was observed between the time of the day (F(1,169) = 1.489, P = 0.224) or any interaction effect (F(5,169) = 0.628, P = 0.679). The trend pattern of missed responses is shown in [Figure 3]. Lapses were significantly higher on D4 and D5 in comparison to baseline and D1 in post hoc analysis. It was also observed that lapses were significantly higher following recovery sleep compared to baseline values [Table 3].
- Means of correct responses with sleep restriction and recovery sleep.
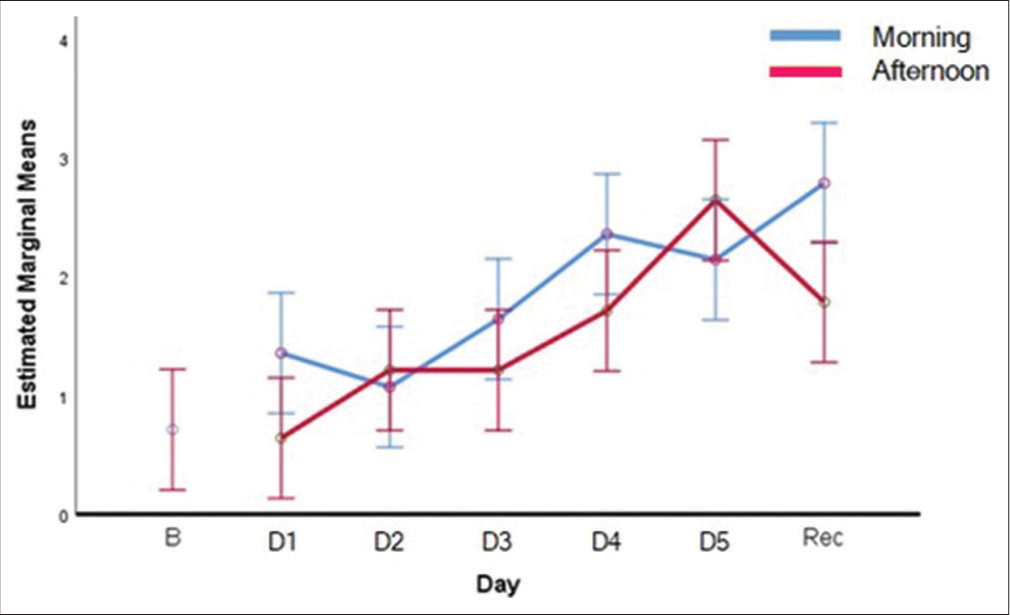
- Means of missed clicks (Lapses) with days of sleep restriction and recovery sleep.
| Day | Baseline | D1 | D2 | D3 | D4 | D5 | Recovery |
|---|---|---|---|---|---|---|---|
| Baseline | - | 0.172 | 0.517 | 0.151 | 0.472 | 0.614 | 0.885 |
| D1 | 0.172 | - | 0.472 | 0.943 | 0.038 | 0.062 | 0.131 |
| D2 | 0.517 | 0.472 | - | 0.428 | 0.172 | 0.250 | 0.428 |
| D3 | 0.151 | 0.943 | 0.428 | - | 0.032 | 0.053 | 0.114 |
| D4 | 0.472 | 0.038 | 0.172 | 0.032 | - | 0.829 | 0.565 |
| D5 | 0.614 | 0.062 | 0.250 | 0.053 | 0.829 | - | 0.719 |
| Recovery | 0.885 | 0.131 | 0.428 | 0.114 | 0.565 | 0.719 | - |
Significant difference across D3 and D4, D1 and D4
| Day | Baseline | D1 | D2 | D3 | D4 | D5 | Recovery |
|---|---|---|---|---|---|---|---|
| Baseline | - | 0.646 | 0.491 | 0.252 | 0.035 | 0.008 | 0.012 |
| D1 | 0.646 | - | 0.778 | 0.399 | 0.043 | 0.007 | 0.012 |
| D2 | 0.491 | 0.778 | - | 0.574 | 0.080 | 0.015 | 0.025 |
| D3 | 0.252 | 0.399 | 0.574 | - | 0.233 | 0.059 | 0.093 |
| D4 | 0.035 | 0.043 | 0.080 | 0.233 | - | 0.550 | 0.622 |
| D5 | 0.008 | 0.007 | 0.015 | 0.059 | 0.550 | - | 0.833 |
| Recovery | 0.012 | 0.012 | 0.025 | 0.093 | 0.622 | 0.833 | - |
Significant differences across D4, D5 and recovery sleep with Baseline and D1
Stroop effect
There was no statistically significant difference in the stroop effect as measure of executive functions (inhibition of the pre-potent response) of the individual across the days (F(5,169) = 0.990, P = 0.434), between times of the day (F(5,169) = 0.01, P = 0.92) as well as interaction effect between day of study and time of day (F(5,169) = 0.202, P = 0.961).
DISCUSSION
Cumulative sleep loss and associated daytime sleepiness can commonly occur in a routine work week. Aviators are at additional risk for the same in view of extended working hours and circadian de-synchrony due to operational requirements. This may result in cumulative sleep loss. In addition, the possibility of chronic sleep loss which may be cumulative over time among aircrew cannot be ruled out in the present era of social media dependence. In real world scenarios, there is a tendency for the individuals to restore their chronic partial sleep deficits over the weekends. However, recovery sleep has not been found adequate for recovering the sleep debt accumulated in some instances.[13,14] This experimental condition was specifically chosen taking into consideration the naturalistic situations in which the aircrew operate and the potential likelihood of accumulating sleep deprivation. In the present study, in a repeated measures design, 14 healthy volunteers were longitudinally followed up twice on a day (morning and afternoon) on their subjective appreciation of sleepiness and performance measures on selected cognitive tests of pSuMedHA test battery (vigilance and executive functions) over a period of 5 days with 2 h of sleep restriction each night and the changes following three consecutive nights of restorative recovery sleep.
The subjective appreciation of sleepiness was assessed in the study using SSS. The findings were clearly indicative of an increase in subjective appreciation of daytime sleepiness with the increment in sleep restrictions [Figure 1]. A significant effect on sleepiness was also observed indicating the post-lunch circadian effect on the perception of sleepiness. However, no interaction effect was observed between the day of study and the time of the day. This means that the post-lunch circadian effect was not significantly affected by the increasing sleep dept.
It can further be inferred from [Figure 1] that the trend in subjective sleepiness got relatively flattened between D2 and D5. Paired comparisons revealed some interesting findings in this regard. The increase in sleepiness became significant on D2 onwards (4 h of sleep restriction) and thereafter, remained non-significant between D3 and D5 even though the increasing sleepiness was significantly higher with accumulating sleep restriction across the days than baseline. These findings are in consonance with the observations in the previous studies[8,15] on chronic partial sleep deprivation which suggest that subjective sensation of sleep is subject to some degree of habituation and mild sleep debt would not affect the subjective appreciation of sleepiness. Further it was observed that no significant difference in sleepiness was observed between baseline and that following recovery. This means that if the 5 days period of sleep restriction is followed by three consecutive nights of restorative sleep, an individual will not perceive unduly higher sleepiness in the daytime.
Literature review suggests that sustained vigilance and executive functions are one of the major domains affected by chronic partial sleep deprivation.[7,8,15,16] Accordingly, Mackworth Clock Test and Stroop Test (the specific subsets pSuMedHA test battery) were used to assess these measures, respectively, in the present study. The vigilance measures assessed by the Mackworth Clock Test were reaction time, accuracy scores (correct clicks), and lapses (missed clicks).[17] Similarly, measures of executive functions assessed by the Stroop Test were Stroop effect. The delay in the reaction between the congruent and incongruent phases of the Stroop test has been the primary outcome variable. The Stroop effect is a delay that indicates the inhibition of the pre-potent reaction and was the outcome variable in this study.[18]
Stroop effect was not significantly affected by the day of study. Various studies mention that the effects of sleep loss may be missed in cognitive measures due to a failure to understand that sleep deprivation increases variability within subjects (i.e., state instability) and between subjects (i.e., differential vulnerability to the effects of sleep deprivation).[19,20] Response inhibition, as an executive function might have been affected by higher inter-subject variability when the effect of cumulative sleep loss is considered. This could have been one of the reasons why no effect was observed on the Stroop effect. Within subject variability caused by state instability could also have affected the findings. For example, the nature of the test might lead to higher arousal and thus preserve executive functions.
Reaction time did not show any significant changes with cumulative sleep restriction; however, correct clicks significantly declined. Thus, it can be stated that with chronic sleep debt, the response time remained intact but at the cost of accuracy. Similarly, a few important observations were made in the analysis of attention lapses. First, the increase in lapses were significantly higher with cumulative sleep restriction of 5 days with a relatively linear pattern [Figure 3]. Second, the increase in lapses was only significant on D4 amounting to 8 h of partial sleep restriction which further increased on day 5 with 10 h of sleep restriction [Table 3]. Third, the increase in lapses remained significant even following three consecutive nights of recovery sleep.
The above findings are considered important in the context of reported literature which suggests that routine repetitive measures, like lapses in vigilance tasks, are known to be sensitive to sleep loss even when it is partial and chronic.[10] Lapses in performance have generally been assumed to be due to micro sleeps[11] and these have the potential to significantly affect aircrew performance and consequent flight safety implications. Further, the finding of incomplete recovery on attention lapses following adequate recovery sleep observed in the present study is in consonance with the previous study. Belenky et al. found that after 3 days of recovery sleep following chronic, mild-to-moderate sleep restriction, lapses measured using psychomotor vigilance did not return to baseline, thus indicating slow or incomplete recovery after a period of cumulative sleep debt. This has been hypothesized to be due to adjustments made by the brain to function optimally during periods of cumulative sleep loss.[13] Persistence of attention lapses has potential implications in aviation operations specifically in the context of the findings of normal appreciation of sleepiness following recovery sleep. With the setting of habituation which is seen in similar studies on cumulative sleep restriction,[11,15] the aircrew might be subjectively not sleep deprived while he or she is still susceptible to attention performance deficits.
CONCLUSION
Cumulative sleep loss over a period of 5 days resulted in more sleepiness and a decrement in vigilance measures even though the executive functions remained intact. An effect of habituation was observed on the 4th day (8 h of accumulated sleep debt) on the subjective perception of sleepiness which returned to baseline following recovery sleep. The lapses were significant on 4th day onward. However, the persistence of attention lapses indicated incomplete recovery of vigilance functions following 3 days of restorative sleep.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Fatigue countermeasures in aviation. Aviat Space Environ Med. 2009;80:29-59.
- [CrossRef] [PubMed] [Google Scholar]
- Fatigue in aviation: A survey of the awareness and attitudes of Indian air force pilots. Int J Aviat Psychol. 2007;17:275-84.
- [CrossRef] [Google Scholar]
- Neurocognitive consequences of sleep deprivation. Semin Neurol. 2009;29:320-39.
- [CrossRef] [PubMed] [Google Scholar]
- Sleep debt: Theoretical and empirical issues. Sleep Biol Rhythms. 2003;1:5-13.
- [CrossRef] [Google Scholar]
- Meta-analysis of the relationship between total sleep deprivation and performance. Chronobiol Int. 1992;9:132-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of sleep deprivation on performance: A meta-analysis. Sleep. 1996;19:318-26.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of sleep deprivation on decision making: A review. J Exp Psychol Appl. 2000;6:236-49.
- [CrossRef] [PubMed] [Google Scholar]
- The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117-26.
- [CrossRef] [PubMed] [Google Scholar]
- Effects Of Sleep Schedules On Commercial Motor Vehicle Driver Performance. United States: Department of Transportation Federal Motor Carrier Safety Administration 2000
- [CrossRef] [PubMed] [Google Scholar]
- Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519-28.
- [CrossRef] [PubMed] [Google Scholar]
- Daytime sleepiness: Quantification of a behavioral state. Neurosci Biobehav Rev. 1987;11:307-17.
- [CrossRef] [PubMed] [Google Scholar]
- Sleepiness: Evaluating and quantifying methods. Int J Psychophysiol. 2001;41:251-63.
- [CrossRef] [PubMed] [Google Scholar]
- Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: A sleep dose-response study. J Sleep Res. 2003;12:1-12.
- [CrossRef] [PubMed] [Google Scholar]
- Physiological arousal and attention during a week of continuous sleep restriction. Physiol Behav. 2008;95:353-64.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of rapid versus slow accumulation of eight hours of sleep loss. Psychophysiology. 2001;38:979-87.
- [CrossRef] [PubMed] [Google Scholar]
- Fatigue and driving: Disentangling the relative effects of time of day and sleep deprivation. Australasian Road Safety Research, Policing and Education Conference In: Adelaide, South Australia, Fatigue and Driving. 2008. p. :713-9.
- [Google Scholar]
- The Mackworth clock test: A computerized version. J Psychol. 2000;134:153-61.
- [CrossRef] [PubMed] [Google Scholar]
- Working-memory capacity and the control of attention: The contributions of goal neglect, response competition, and task set to stroop interference. J Exp Psychol Gen. 2003;132:47-70.
- [CrossRef] [PubMed] [Google Scholar]
- Dealing with inter-individual differences in the temporal dynamics of fatigue and performance: Importance and techniques. Aviat Space Environ Med. 2004;75(Suppl 3):A147-54.
- [Google Scholar]
- Nonlinear mixed-effects modeling: individualization and prediction. Aviat Space Environ Med. 2004;75(Suppl 3):A134-40.
- [Google Scholar]






