Translate this page into:
Teaching Series : Aviation Medicine Electrocardiographic abnormalities in aircrew-I
Electrocardiography is used routinely amongst aviators for screening for cardiovascular diseases. Baseline electrocardiography is considered Class 1 (appropriate) indication for use in aircrew as a screening test as per American College of Cardiology/American Heart Association guidelines [1]. Electrocardiographic (ECG) abnormalities are one of the commonest abnormalities detected during routine medical evaluation of asymptomatic aircrew. This series is an attempt to give a background of some of the commonest ECG abnormalities and elucidate the methods of evaluation and their aeromedical disposition. About 10% of ECG’s may have some variation from ‘normal’ which may be a normal variant or some frank abnormality [2]. Some of the commonest ECG findings seen are rhythm disorders like sinus bradycardia, sinus arrhythmia, abnormalities of conduction like AV blocks and bundle branch blocks, and others like axis deviation, ST-T changes etc.
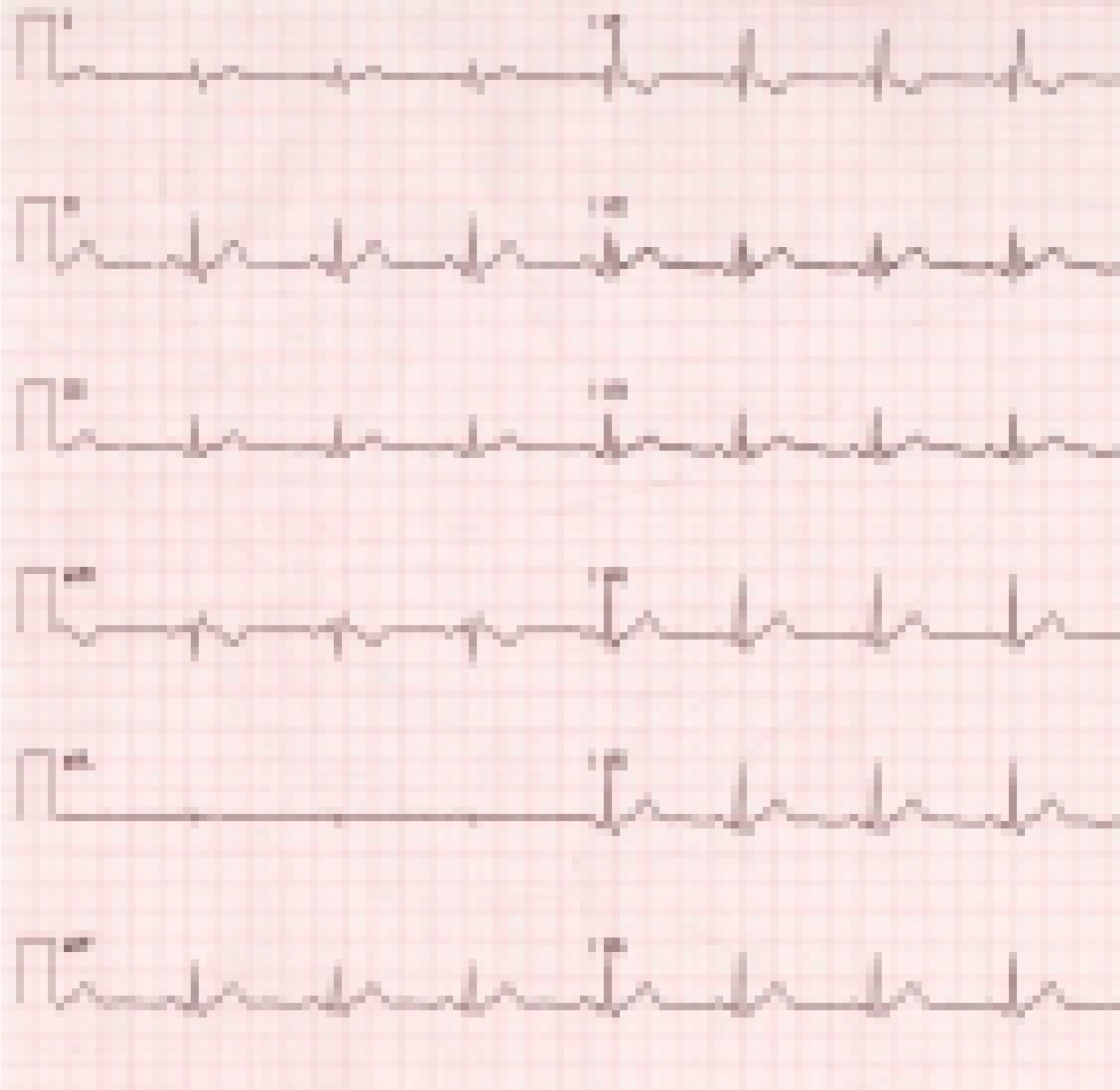
Clinical problem. The following is an ECG recording of a 35 yr old commercial pilot taken during routine medical examination prior to renewal of licence. The individual is asymptomatic, has no coronary risk factors and exercises regularly- jogs 3-5 km most of the days of the week. Clinical examination revealed a mesomorphic individual, normotensive and unremarkable systemic examination except for a prominent split of the second heart sound. Previous ECG’s have been reported as normal.
His resting ECG shows Right Bundle Branch Block. The characteristics of RBBB are:-
A late intrinsicoid deflection rsR' in V1
Early intrinsicoid S wave in V6
Wide S wave in LI
RBBB can be complete or incomplete based on the duration of QRS complex ( >0.12 and < 0.12s respectively) [3].
The mechanism of RBBB
Normally the major portion of the normal QRS complex is contributed by the right ventricle [3]. Therefore there is minimal distortion of the early portion of the QRS complex and marked distortion of the late portion of the QRS contributed by the right ventricle in RBBB. As the right ventricle is activated via the impulses from the left ventricle there is a late prominent R’ wave in V1.
Approach to a case of RBBB
Unlike LBBB, RBBB is a relatively benign condition. It is one of the commonest ECG abnormalities detected during routine medical examinations with an incidence of 0.2% to 0.4% with increasing prevalence with advancing age [2]. The cause of these conduction abnormalities is fibrosis of the Purkinje fibres. Other factors like ischaemia and lengthening of the tract due to chamber dilatation can contribute to conduction blocks. Follow up of a large number of individuals with RBBB has indicated that it is by and large non progressive if underlying heart disease is excluded [4,5]. But when RBBB exists with a heart disease, it invariably indicates a fairly advanced disease and can be seen in the following conditions:-
Acute pulmonary thromboembolism
Coronary artery disease
Right sided pathologies like cor pulmonale
Myocarditis
Surgically induced following cardiac interventions
Congenital disorders like Brugada syndrome (where it is associated with ST elevation) and congenital heart disease like atrial septal defect.
Keeping these in mind, the following approach to cases of RBBB is suggested:-
History. Detailed history of cardiovascular and respiratory symptoms, family history and cardiovascular risk factors.
Examination. In the absence of structural heart disease there is no abnormality on examination except for wide splitting of the second heart sound. While wide splitting of the second heart sound is often heard, fixed splitting of the second heart sound can be associated with an atrial septal defect. Remember that the abnormalities of the second heart sound must be heard in the sitting position since splitting is often wide in normals while supine.
-
Investigations
ECG. Associated changes with RBBB are to be looked for e.g., ST-T changes, axis deviation- left axis deviation indicates associated LAHB which will make it a bifascicular block.
Exercise stress testing. All aircrew with RBBB should undergo exercise stress testing to rule out inducible ischaemia. It has to be kept in mind that exercise induced ST depression with T- wave inversion is a common finding in leads V1-V3 in RBBB and is nondiagnostic. Of more diagnostic significance is ST depression in V5 or V6, II and avF, reduced exercise capacity and inability to adequately increase systolic blood pressure [6].
2D Echocardiography. To look for chamber enlargements, right ventricular strain, regional wall motion abnormalities, valvular heart disease and congenital disorders like atrial septal defect.
The above non invasive investigations would suffice to rule out any cardiac disorder and depending on their results further investigations like nuclear imaging, coronary angiography and electrophysiological studies may be indicated.
Aeromedical disposal
Aviators can be assessed fit for RBBB if there is no underlying heart disease and all the above investigations are normal since the overall prognosis would then be good [7].
As per the guidelines adopted by the Indian Air Force, the absence of a structural heart disease must be excluded by investigations at a specialist centre. If all investigations are normal and the block is considered idiopathic, persistent and non-progressive after a period of observation in medical category A4G3 for 12 to 24 weeks, full category can be awarded. However, if it is a fresh detection especially in later age groups, all investigations to rule out Coronary Artery Disease must be carried out. If these are negative, medical category A2G2(P)/ A4G2 (P)/ BEE(P) can be awarded. In the latter instance, fitness to fly fighters will be decided on the clinical merits of each case [8].
The above civil aircrew underwent TMT and 2 D echocardiography, which were normal and was declared fit for flying duties with no restrictions.
References
- Guidelines for Eectrocardiography: A report of the American College of Cardiology/ American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Committee on Electrocardiography) J Am Coll Cardiol. 1992;19:473.
- [Google Scholar]
- Marriot’s Practical Electro cardiography (10th ed). Lippincot: Williams & Wilkins; 2001.
- [Google Scholar]
- The frequency and prognostic significance of electrocardiographic abnormalities in clinically normal individuals. Prog Cardiovas Dis. 1981;23:299-319.
- [Google Scholar]
- Exercise Stress Testing In: Braunwald’s Heart Disease: A textbook of Cardiovascular medicine Zipes, Libby, Bonow, Braunwald eds (7th ed). Elsevier Saunders; 2005. p. :170.
- [Google Scholar]
- Cardiology In: Clinical Aviation Medicine (3rd ed). Castle Connolly: Graduate Medical Publishing; 2000. p. :151.
- [Google Scholar]
- Manual of Medical Examinations & Medical Boards In: IAP 4303 (3rd edition). New Delhi: Air Headquarters; 2003.
- [Google Scholar]





