Translate this page into:
Effects of post short nap sleep inertia on cognitive and psychomotor task performance

*Corresponding author: Dr DR Bhatt, MBBS, MD (Aerospace Medicine), Flight Surgeon, Army Aviation Squadron, Ganderbal - 191201, J & K, India drajbhatt@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhatt DR, Tripathy NK, Shekhar BM, Divya N. Effects of post short nap sleep inertia on cognitive and psychomotor task performance. Indian J Aerosp Med 2021;65:74-80.
Abstract
Introduction:
Sleep inertia, a detrimental effect of daytime nap, may affect cognitive functions following awakening. The present study aimed to assess the effects of sleep inertia on cognitive and psychomotor tasks following short nap of 30 min taken in the afternoon hours, a realistic probability in the aerospace operational environment.
Material and Methods:
In a repetitive measure design, 30 healthy male volunteers having adequate sleep the previous night, were tested for changes in cognitive and psychomotor performance following 30 min of nap after lunch at the Sleep-cum-Group confinement lab. Post nap longitudinal testing for dual task (DT) test and Stroop test was carried out in periodic intervals for 40 min. DT response time (DTRT), DT lag error (DTLE), DT correct clicks (DTCC) and response time difference (Stroop Effect [SE]) were analyzed as performance measures.
Results:
There was a significant increase in DTRT (χ2 =11.13, P = 0.011) in the post-nap period as compared to pre-nap baseline values. No significant changes were observed in other parameters vis DTLE, DTCC, and SE. Post-hoc analysis revealed that the increase of DTRT was significant at 6 min post-nap session; following which the changes were not statistically significant.
Conclusion:
Sleep inertia was found to affect speed component of the task rather than accuracy in a post-nap period of 30 min. The effect was significant at 6 min following awakening and after that, the effects got dissipated. Although nap can be an effective strategy for sleep-alertness management, the effects of sleep inertia have to be borne in mind, especially during sustained military operations.
Keywords
Sleep inertia
Nap
Psychomotor task
Cognitive performance
Dual task lag error
INTRODUCTION
Loss of adequate sleep due to sustained and continuous air operations have the potential of developing fatigue and resultant decrement in pilot performance. A pilot is required to operate with speed, precision, and accuracy for successful operations; however, all these factors are likely to be affected due to sleep loss. In addition, such conditions are conducive for pilot errors and hence, are likely to affect aerospace safety. For a healthy individual, approximately 8 h of sleep in a day is considered the basal requirement. Sleep serves the restorative function by permitting the brain and the body to rest and recuperate from the daily wear and tear. This, in turn, maintains human performance under various situations. A decrement in quantity, as well as quality of sleep, thus affects these functions and results in decrement in performance.
To ensure effective performance in the subsequent period, strategic naps have been used as an effective countermeasure both in military as well as commercial civil flying. Napping has been specifically helpful during periods of extended wakefulness such as sustained and continuous military operations, night operations, shift work, and long-haul air operations. However, sleep inertia, a period of transitory hypo-vigilance, confusion, disorientation, and impaired cognitive and behavioral performance,[1,2] could result in significant decrement in pilot performance specifically in demanding situations such as complex and challenging aviation tasks. Such situations may arise in aviation environment quite often. During these conditions, if the pilot is awakened from nap and asked to perform the task immediately, the situation can be dangerous, thus compromising flight safety. The optimum nap duration in an operational scenario should depend on the duration and magnitude of sleep inertia.[2,3] Sleep inertia can last from 5 to 35 min depending on many variables[4] such as; (a) abruptness of awakening,[5,6] (b) time between awakening and task performance,[6] (c) type of task,[7] (d) stage of sleep from which the individual woke up,[8] and (e) previous sleep deprivation, if any.[9]
In general, a short nap of 30 min is often taken in the post-lunch afternoon hours. Such a practice is in existent and routinely being followed, especially, if there is a planned flying mission in the subsequent period. Examination of the effects of sleep inertia on the aviation-specific cognitive and psychomotor tasks in the period following a 30-min short afternoon nap was the aim of the study.
MATERIAL AND METHODS
Subjects
A total of 30 healthy male volunteers with an age of 33 ± 5.4 years participated in the study with a written informed consent. History of any sleep or medical disorders, taking any drugs, and consumption of alcohol in the past 24 h prior were excluded from the study. Ethical clearance was obtained from Institute Ethics Committee.
Materials
Materials used in the study were; (a) Actigraph (Philips Respironics Spectrum Plus Actiwatch)[10] to monitor pattern and quality of restful sleep in the previous night of the study, (b) Groningen Sleep Quality Scale (GSQS)[11] to assess the quality of sleep in the previous night; it comprises a set of 15 questions (true/false types) which subject has to answer and scoring done accordingly, (c) Karolinska Sleepiness Scale (KSS)[12] to assess the subjective sleepiness; participants were required to answer the question “How do you feel at this moment?” out of 9-point scale ranging from “Extremely alert” to “very sleepy, great effort to keep awake, fighting sleep,” (d) EEG machine (Alice® PDx™ Portable Sleep Diagnostic System)[13] to qualitatively assess the nap and post-nap period, (e) Psychometric Evaluation Designed for Aviators (pSuMEDhA) – an indigenously designed software based cognitive and psychomotor tasks;[14] from the cognitive and psychomotor battery of tests of pSuMEDhA, dual task test (DTT) and Stroop test (ST) were used. Outcome measures assessed were - DT response time (DTTR), DT correct clicks (DTCC), DT lag error (DTLE), and difference in response time between two phases of ST - Stroop Effect (SE).
Experimental protocol
The study was conducted at the Sleep-cumGroup Confinement Laboratory at the Institute of Aerospace Medicine. The participants were explained about the test procedure prior to the study, were asked to wear the Actigraph watch, and advised to have a restful sleep in the night prior to start of the test. On the day of the experimentation, the participants reported to Sleep Lab at 0800 h and were asked to fill up the GSQS Questionnaire. Then the participants were advised to report to their normal place of work and do only routine works not involving strenuous activities. They were asked to report back to sleep laboratory at 1330 h after having their lunch. Their level of sleepiness was assessed using KSS and then, EEG electrodes were attached at C3 and C4 locations on the scalp for standard Bipolar EEG recording using 10/20 International System. DT Test (DTT) and ST (a total of 09 min) were conducted between 1330-1400 h that was labeled as pre-nap baseline data. The participants were then allowed to take 30 min of nap in the sleep lab under controlled environment. They were woken up after 30 min using a sound alarm. Following that 1st data set comprising DTT and ST was done 3 min after nap and then repeated longitudinally at an interval of 06 min till completion of study protocol i.e. 40 min post-awakening. EEG recording continued for the entire duration of nap as well as post-nap till completion of the study. Experimental design is illustrated in Figure 1.

- Experimental design.
Data analysis
Data was compiled and analyzed using IBM SPSS ver 26. Sample size estimation was done using G Power ver 3.1.9.4. All the parameters were checked for normal distribution, using visual inspection of histograms and normality Q-Q plots. Non-parametric tests (Friedman test) were used to make statistical inference as data were not normally distributed. Not normally distributed quantitative variables were summarized by median and interquartile range. Pair-wise comparisons were done using post-hoc test using the Nemenyi Test method for P-value correction. P < 0.05 was considered as statistically significant.
RESULTS
The scores of GSQS obtained between 0800 h and 0900 h revealed a score of “zero” for 27 participants and “one” for 3 participants. The scores of KSS obtained between 1330 and 1400 h showed a score of 0–2 for three participants and score of 3–5 for 27 participants.
DTT
Response Time
The data pertaining to changes in mean response time in DTT is presented in Table 1. The data is depicted in line diagram and Box-and-Whisker plot in Figures 1 and 2, respectively. The DTT showed a significant increase (χ2 =11.13, P = 0.011) in the post-nap period. Post-hoc pairwise analysis (Nemenyi Test) revealed that the increase in DTT was significant only between pre-nap period vis-à-vis 6 min post-nap timepoint. No significant difference was observed at 21 min and 36 min post-nap timepoints.
| Time point | DTT -response time (dual task) (ms) | Friedman test | |||
|---|---|---|---|---|---|
| Mean (SD) | Median (inter quartile range) | Range | X2P-value | P-value | |
| Pre-nap | 536.43 (60.98) | 541.50 (89.75) | 420.00-649.00 | 11.13 | 0.011 |
| 6 min | 573.57 (60.23) | 569.00 (81.50) | 438.00-718.00 | ||
| 21 min | 557.87 (44.12) | 541.00 (65.00) | 470.00-656.00 | ||
| 36 min | 565.27 (59.81) | 568.00 (76.50) | 432.00-688.00 | ||

- Line diagram showing change in DTT in ms over time.
Correct Clicks
The mean correct clicks (dual task) decreased in the post-nap period as compared to the pre-nap period. However, the change was not statistically significant (Friedman Test: χ2 = 7.1, P = 0.068). The data are presented in Table 2 and Figure 3.
| Time point | Correct clicks (dual task) | ||
|---|---|---|---|
| Mean (SD) | Median (inter quartile range) | Range | |
| Pre-nap | 4.17 (2.02) | 4.00 (2.75) | 1.00-8.00 |
| 6 min | 3.17 (1.86) | 3.00 (2.00) | 0.00-8.00 |
| 21 min | 3.83 (1.74) | 4.00 (1.75) | 1.00-7.00 |
| 36 min | 3.67 (1.97) | 3.00 (3.00) | 1.00-8.00 |

- Line diagram showing change in correct clicks over time.
Lag Error
The mean lag error (dual task) decreased post-nap period as compared to pre-nap period. However, the change was not statistically significant (Friedman Test: χ2 = 1.3, P = 0.724). The data is presented in Table 3 and Figure 4.
| Timepoint | Lag error | (dual task) | Friedman test | |
|---|---|---|---|---|
| Mean (SD) | Median (inter quartile range) | x2 | P-value | |
| Pre-nap 6 min 21 min 36 min | 8.63 (1.97) 8.55 (1.35) 8.62 (1.31) 8.87 (4.82) | 8.63 (1.90) 8.19 (2.09) 8.25 (1.83) 7.96 (1.45) | 1.3 | 0.724 |

- Line diagram showing change in lag error (dual task) over time.
Stroop Test
The mean response time difference Stroop Error (SE), showed an increment in the post-nap period as compared to pre-nap period. However, the change was not statistically significant (Friedman Test: χ2 = 5.7, P = 0.127). The data are presented in Table 4 and Figure 5.
| Timepoint | SE (ms) | Friedman test | ||
|---|---|---|---|---|
| Mean (SD) | Median (inter quartile range) | X2 | P-value | |
| Pre-Nap | 50.33 (40.60) | 42.50 (29.75) | 5.7 | 0.127 |
| 12 min | 57.27 (47.48) | 47.50 (56.50) | ||
| 27 min | 67.77 (48.64) | 56.00 (65.75) | ||
| 42 min | 54.47 (51.33) | 34.50 (62.50) | ||
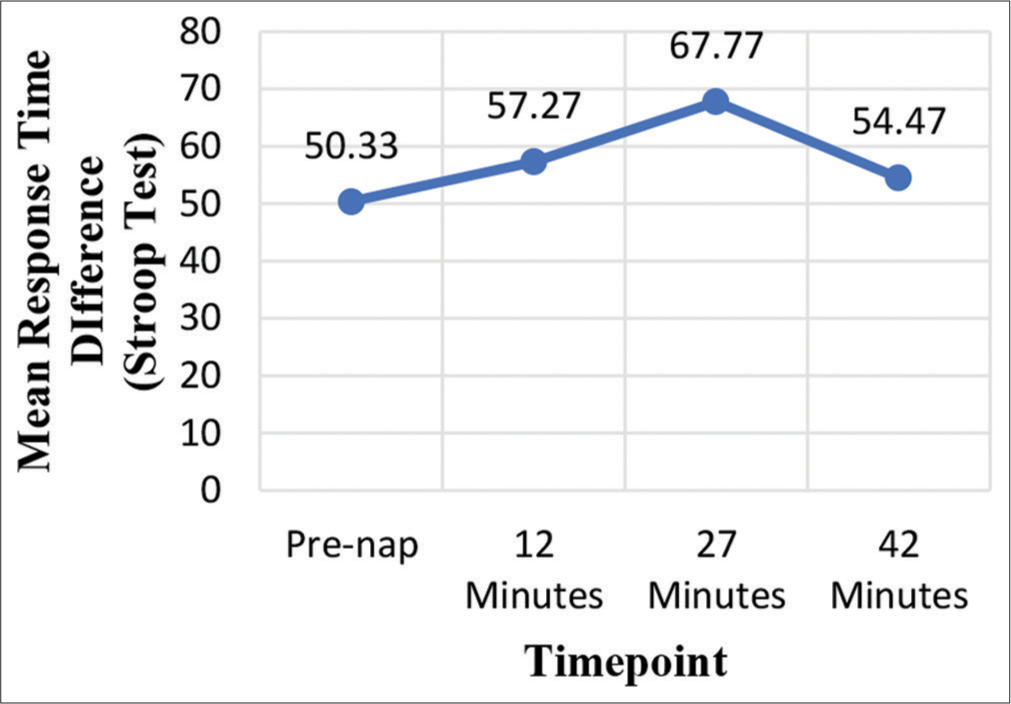
- Line diagram showing SE over time.
DISCUSSION
Numerous studies have been conducted in the past on sleep physiology and human performance. Whereas the consequences of sleep deprivation on performance have been the focus of research, studies on the effects of sleep inertia on performance are scant. Similarly, while emphasis has been given to the effects of the onset of sleep on sleep physiology; little attention has been given to the effects of sleep in the subsequent awakening period. Most studies on sleep inertia have been done in various conditions of sleep deprivation of varying periods, either in night or day. However, to maintain alertness during a long-duration mission or night flying, short-duration afternoon nap following a normal sleep the previous night, is a more realistic probability. More often or less, aircrew generally resort to 30 min of nap following lunch. Studies on the effects of sleep inertia on performance following such short duration naps are relatively scant. With this background, the present study was undertaken to understand the effects of sleep inertia on cognitive and psychomotor performance occurring in the most probable realistic situation.
In a repetitive measure design, 30 healthy volunteers having adequate sleep in the previous night were tested longitudinally for changes in cognitive performance following 30 min of nap in the afternoon hours after lunch. From the GSQS, it could be inferred that all our participants had good quality of sleep in the previous night. The pre-nap performance data was taken as the baseline values to study the effects in the post-nap period. None of the participants in pre-nap assessment had a score more than 6 in KSS scores, indicating that none of the participants had abnormal sleepiness during the baseline recording.[12] Two cognitive tests vis DTT and ST from the pSuMEDhA test batteries were used as these tests are sensitive to detect any decrement related to psychomotor and cognitive functions. EEG was used to qualitatively monitor the nap and post nap-period.
The results of the effects of sleep inertia on DTT revealed that there was a significant increase in mean DTRT in the post nap period [Table 1 and Figures 2 and 6], whereas, the changes in mean DTCC and mean DTLE were not statistically significant [Tables 2 and 3; and Figures 3 and 4]. Thus, it can be concluded from the above findings that sleep inertia following 30 min nap could affect response time even though accuracy can be preserved. This finding is in consonance with the previous studies which have shown that sleep inertia affects the speed component rather than accuracy.[1,14-18] Studies have shown that the lapses or the lag errors (accuracy) are not important features of the sleep inertia but are associated with sleep loss induced microsleeps.[16,17] However, there are several other studies documenting equal effects of sleep inertia on both speed and accuracy measures[9,19,20] or greater effects on accuracy.[21] Differences in the type of tasks, time of testing, the duration and timing of sleep, and instructions to the subjects (e.g. instructed to perform as fast and/or as accurately as possible) may account for these variations. The interference test scoring to study the SE was used in the study as has been used as the most favored parameter by many authors.[22-24] In the present study, sleep inertia effects were not observed on interference phenomenon tested by ST [Table 4 and Figure 5]. Hence, it can be deduced that executive functions remained unaffected due to sleep inertia induced by 30 min nap.

- Box-and-Whisker Plot showing change in DTT in ms over time.
Further Post-hoc analysis revealed that the increase in response time (DTRT) was only statistically significant at 6 min post-nap period, whereas this was not statistically significant following that [Table 5]. Thus, it could be inferred that sleep inertia dissipation might occur early following 30 min nap. It is also to be appreciated that effects of sleep inertia could be task dependent.[2,25-28] The above observation is well supported by the findings of previous studies. 30 min nap taken in the afternoon were part of experimental protocol in two similar studies.[27,28] Performance was significantly lower compared to pre-nap levels at 5 min post-nap[27] and worse than subsequent testing points.[28] Compared to prenap and the no-nap condition, at 35-min post-nap, no differences were observed for most performance measures in both the studies. However, both subjective and objective sleepiness were decreased compared to those in the no-nap condition at 65-min post nap.[27,28] These findings suggest that sleep inertia was evident for at least 5 min after a 30-min afternoon nap and that advantages of the nap appeared after 60 min.
| Comparison of response time (dual task) at various timepoints vs pre-nap | Mean (SD) of difference (ms) | Median (inter quartile range) of difference (ms) | P-value |
|---|---|---|---|
| 6 min - Pre-nap | 37.13 (73.80) | 31.00 (51.50) | 0.010 |
| 21 min - Pre-nap | 10.17 (66.99) | 25.50 (85.50) | 0.481 |
| 36 min - Pre-nap | 28.83 (72.03) | 29.50 (69.00) | 0.075 |
Post hoc pairwise tests for Friedman test performed using Nemenyi Test method for P-value correction.
Our study had certain limitations; (a) the study did not include a control group with no nap condition. That could have additionally provided the data to further validate the findings of the present study. (b) Data on sleepiness scale was only taken in pre-nap period. Inclusion of sleepiness scale along with objective tasks in post-nap period would have enabled subjective appreciation of sleepiness and alertness and could have been correlated with performance measures. (c) EEG was used in the study only for qualitative assessment of sleep in the nap period. Quantitative EEG analysis could have provided neurophysiologic correlates of effects of sleep inertia.
CONCLUSION
Based on the results of our study, two important conclusions could be drawn on the effects of sleep inertia following a 30-min post-nap period, in well-rested individuals the previous night. These are; (a) Sleep inertia was found to affect speed component of the DT rather than accuracy. The effects of which might get dissipated after 6 min of post-nap period. (b) Executive functions might not be affected by sleep inertia as there was no significant SE in the post-nap period. The results of the present study may be validated in operational conditions using aviation-specific tasks and flying-related performance measures. Nevertheless, though nap can be an effective strategy for sleep-alertness management, the effects of sleep inertia have to be borne in mind, especially during sustained military operations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr NK Tripathy is the Executive Editor of the Journal. He does not have any conflicts of interest.
References
- Sleep inertia: Best time not to wake up? Chronobiol Int. 1993;10:109-18.
- [CrossRef] [PubMed] [Google Scholar]
- Time course of sleep inertia after nighttime and daytime sleep episodes. Arch Ital Biol. 1995;134:109-19.
- [Google Scholar]
- Sleep loss and fatigue in residency training: A reappraisal. J Am Med Assoc. 2002;288:1116-24.
- [CrossRef] [PubMed] [Google Scholar]
- A review of short naps and sleep inertia: Do naps of 30 min or less really avoid sleep inertia and slow-wave sleep? Sleep Med. 2017;32:176-90.
- [CrossRef] [PubMed] [Google Scholar]
- Are you awake? Cognitive performance and reverie during the hypnopompic state In: Bootzin R, Kihlstrom J, Schacter D, eds. Sleep and Cognition. Washington, DC: American Psychological Society; 1990. p. :159-75.
- [CrossRef] [Google Scholar]
- The effects of sleep inertia on decision-making performance. J Sleep Res. 1999;8:95-103.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of slow-wave sleep (SWS) deprivation and time of night on behavioral performance upon awakening. Physiol Behav. 1999;68:55-61.
- [CrossRef] [Google Scholar]
- Fatigue in Aviation Sustained Operations, the Utility of Napping, and the Problem of Sleep Inertia USA: Army Aeromedical Research Lab; 2002.
- [Google Scholar]
- Relationship between sleep inertia and sleepiness: Cumulative effects of four nights of sleep disruption/restriction on performance following abrupt nocturnal awakening. Biol Psychol. 1988;27:245-58.
- [CrossRef] [Google Scholar]
- United States: Philips Respironics Inc. Available from: https://www.usa.philips.com/ [Last accessed on 2021 March 15]
- [Google Scholar]
- Effect of simulated dawn on quality of sleep-a community-based trial. BMC Psychiatry. 2003;3:14.
- [CrossRef] [PubMed] [Google Scholar]
- Subjective sleepiness is a sensitive indicator of insufficient sleep and impaired waking function. J Sleep Res. 2014;23:242-54.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of sleep inertia on cognitive performance following a 1-hour nap. Work Stress. 1995;9:528-39.
- [CrossRef] [Google Scholar]
- Comparing sleep-loss sleepiness and sleep inertia: Lapses make the difference. Chronobiol Int. 2008;25:725-44.
- [CrossRef] [PubMed] [Google Scholar]
- Sleep inertia: Performance changes after sleep, rest and active waking. Cogn Brain Res. 2005;22:323-31.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of self-awakening from nocturnal sleep on sleep inertia. Biol Psychol. 2010;83:15-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prepared by the Sleep Disorders Classification Committee, Roffwarg HP. Sleep. 1979;2:1-137.
- [Google Scholar]
- State transitions between wake and sleep, and within the ultradian cycle, with focus on the link to neuronal activity. Sleep Med Rev. 2004;8:473-85.
- [CrossRef] [PubMed] [Google Scholar]
- Selective slow-wave sleep deprivation and time-of-night effects on cognitive performance upon awakening. Psychophysiology. 2000;37:440-6.
- [CrossRef] [PubMed] [Google Scholar]
- The stroop color-word test: A review. Acta Psychol (Amst). 1966;25:36-93.
- [CrossRef] [Google Scholar]
- Half a century of research on the Stroop effect: An integrative review. Psychol Bull. 1991;109:163-203.
- [CrossRef] [PubMed] [Google Scholar]
- Sleep inertia In: Sleep Medicine Reviews. Vol 4. United States: WB Saunders Ltd; 2000. p. :341-53.
- [CrossRef] [PubMed] [Google Scholar]
- Time-course of sleep inertia upon awakening from night time sleep with different sleep homeostasis conditions. Aviat Space Environ Med. 2000;71:225-9.
- [Google Scholar]
- The short-term benefits of brief and long naps following nocturnal sleep restriction. Sleep. 2001;24:293-300.
- [CrossRef] [PubMed] [Google Scholar]
- A brief afternoon nap following nocturnal sleep restriction: Which nap duration is most recuperative? Sleep. 2006;29:831-40.
- [CrossRef] [PubMed] [Google Scholar]






