Translate this page into:
Effect of acute normobaric hypoxia on passively simulated illusions: A double-blind randomized study

*Corresponding author: Dr SK Iyer, MBBS, Resident in Aerospace Medicine, Institute of Aerospace Medicine IAF, Vimanapura, Bengaluru - 560017, Karnataka, India. driyersrihari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Iyer SK, Kumar A, Mohapatra SS. Effect of acute normobaric hypoxia on passively simulated illusions: A double-blind randomized study. Indian J Aerosp Med 2021;65(1):23-8.
Abstract
Introduction:
Number of accidents in the past four decades in rotary wing flying in high altitude areas in the Indian Air Force have been attributed to spatial disorientation (SD) or hypoxia or both. Although the two aviation stressors; hypoxia and SD, have been studied independently, literature is scant on the combined effects of the two notorious factors in military aviation.
Material and Methods:
In a double-blind randomized control design, 32 healthy volunteers divided into two groups (hypoxia group and normoxia group) of 16 subjects each, participated in the study. Subjects in the hypoxia group were exposed to normobaric hypoxia with pre-mixed gases in cylinders with nitrox gas (simulating altitude of 22,000 ft) and the normoxia group was exposed to normal air. Autokinesis time (AT) and vestibular adaptation time (VAT) during acceleration and deceleration, in both clockwise and counter-clockwise turns, were studied as surrogates for SD in both hypoxia group and normoxia group in Disorientation Simulator.
Results:
Mean AT showed a statistically significant decrease (t = −2.2, P = 0.039) in hypoxia group compared to normoxia group. Similarly, a statistically significant reduction (F = 5.989, P = 0.016) in mean VAT was observed in in hypoxia group compared to normoxia group. There was no significant difference in the VAT in clockwise and counter-clockwise yaw rotation in both the groups.
Conclusion:
A significant reduction in AT indicates that hypoxia may increase the onset of autokinesis early. The changes in VAT in hypoxic conditions bring out a possible effect of hypoxia on the adaptability of the vestibular system in the angular motion environment.
Keywords
Normobaric hypoxia
Spatial disorientation
Autokinesis time
Vestibular adaptation time
Passive illusions
INTRODUCTION
The Indian Armed Forces operate helicopter missions from the helipads located at very high altitudes. Such missions can expose the aircrew to hazardous effects of hypoxia, since these aircraft are not pressurized. Hypoxia for long has been recognized as a significant physiological threat in High Altitude Area (HAA) operations.[1] It has been documented that hypoxia is a silent operator in HAA operations which may lead to errors of judgment. These errors of judgment are difficult to establish as there are no aftereffects or signs that persist after cessation of exposure to hypoxia.[2] Unlike helicopters, aircrew in fighter aircraft is shielded to a certain extent from the effects of hypoxia by the inbuilt system of cabin pressurization and oxygen systems in fighters. A study conducted in the Indian Army Aviation on helicopters flying over HAA revealed 29 accidents. Out of this, 24% of all and 30% of human factors accidents were attributed to hypoxia as a contributory factor.[3] Ghosh emphasized that hypoxia was a worrying bane and stressed on the importance of preventing hypoxia and addressing the issue head-on and improve flight safety.[4] The human brain is very sensitive to hypoxia, and impairment of vision and neurocognitive responses are known to occur. It has been documented that cognitive functions such as working memory and decision making may be affected as low as 3000 m (9,843 ft) above sea level.[5] The operation of the aircraft in HAA becomes even more complex as the pilot can neither fly fully on visuals or fully on instruments and are thus more prone to Spatial Disorientation (SD).[6] A number of accidents in the past four decades in rotary wing flying in HAA have been attributed to SD or hypoxia or both.[3,4,7,8]
Although the two issues, hypoxia and SD, have been studied independently; there is very little, if any, literature available regarding the interplay or synergism between both the notorious factors in military aviation. An analysis of the causation of SD reveals that higher mental functions and central processing play a major role in the occurrence of the phenomenon. At the same time, mental performance is affected significantly by hypoxia. This implies that hypoxia may possibly affect visual and vestibular functions, the inputs from which are considered essential for orientation and disorientation in-flight. With this background, the present study was undertaken to examine the influence of hypoxia on propensity to develop SD. Autokinesis Time (AT) and Vestibular Adaptation Time (VAT) were taken as surrogate marker for SD.
MATERIAL AND METHODS
Subjects
Thirty-two healthy volunteers, matched with age and BMI, were included for the study. The mean age and BMI of the participants were 32.3 years and 25.16 kg/m2 respectively. History of any neuro-vestibular or ocular diseases, motion sickness, sleep disorders, and intake of medications were considered as exclusion criteria.
Materials
The study was conducted in the Department of Acceleration Physiology and Spatial Orientation (AP and SO) at the Institute of Aerospace Medicine (IAM) Indian Air Force. A system with ability to deliver mixture of nitrox gas was used to simulate Normobaric Hypoxia (NH) condition. The oxygen saturation corresponding to the desired simulated altitude was assessed using pulse oximetry. The symptoms of hypoxia experienced by the subjects were assessed by a questionnaire.[9] AirFox Diso® simulator was used to measure AT and VAT.
Experimental design
In a double-blind randomized designed, 32 subjects were divided into two groups with 16 subjects in each; Group A-hypoxic group and Group B-normoxic group. Group A was exposed to NH by means of providing a mixture of nitrox gas simulating an equivalent altitude of 22,000 ft (FiO2 9.1% – corrected for local altitude of 3000 ft); whereas, Group B was exposed to normal air.
Experimental protocol
Ethical clearance was obtained from the Institute Ethics Committee. The subjects were familiarized with the experiment to alleviate their apprehension, if any. An informed written consent was obtained from each participant. The subjects were advised not to consume tea/ coffee and smoke 2 h and not to consume alcohol 12 h before the study. A trial exposure in the AirFox Diso® was given 3 days before the actual study to familiarize them with the phenomenon of autokinesis and rotation in yaw axis for recording of AT and VAT, respectively. To double-blind the study, all the subjects were given the breathing mixture of gases. Randomization was carried out to assign the subject to Group A or Group B, testing for AT or VAT first and to ascertain whether clockwise or counterclockwise turns were to be provided first. The subjects were monitored on the Instructor Station by the researchers by means of a closed-circuit television and two-way communication. The following procedures were followed for recording of the outcome parameters:-
AT
To record AT, a white dot was provided on the screen with total dark conditions inside the simulator. The subject was advised to close his/her eyes, and to open on the command of the researcher. The stopwatch was started when the subject opened eyes and stopped the moment the subject reported any movement of the white dot (autokinesis).
VAT
Complete darkness was maintained inside the simulator. To record VAT for accelerations, the stopwatch was started immediately on clicking the start button for the turns in yaw axis of the simulator at 10 rpm. The subjects would perceive the turn and call out “Yes” the moment they stopped perceiving the turn. The stopwatch was stopped at this point of time and noted as VAT for acceleration (The rate of acceleration was 5 ms-2). For VAT during decelerations, the stopwatch was started the moment the turns of the simulator in the yaw axis was stopped. The subject now perceived the turn in the opposite direction and would call out “Yes” the moment they stopped perceiving it. The stopwatch was stopped at this point of time and noted as VAT for deceleration (The rate of deceleration was 5 ms-2). VAT scores were noted on four occasions. VAT during acceleration in clockwise and counterclockwise turns was noted as VAT1 and VAT3, respectively, and VAT during deceleration in clockwise and counterclockwise turns wa noted as VAT2 and VAT4, respectively.
Statistical analysis
Data were entered on MS Excel and were analyzed with IBM SPSS Version 26. Descriptive statistical analysis was carried out. Data were checked for normality using Shapiro-Wilk “W” Statistic. Comparison between the two groups was done using Independent t-test for autokinesis. Two-way ANOVA was used to analyze the data of VAT. Significance was assessed at p < 0.05.
RESULTS
The hypoxia symptoms reported by the subjects in the hypoxic group is depicted in Table 1. No symptoms were reported by the subjects in the normoxic group. The mean AT recorded in the hypoxic group was 12.92 ± 7.36 s; whereas, that in normoxic group was 22.25 ± 15.29 s. Independent t-test revealed that such a reduction in mean AT in hypoxic group was statistically significant (t = −2.2, P = 0.039) with an effect size of 0.71 (Cohen’s D). The same is depicted in Figures 1 and 2.
| Sl No. | Symptoms | Percentage | Sl No. | Symptoms | Percentage |
|---|---|---|---|---|---|
| 1. | Lightheaded | 75 | 13. | Euphoric | 12.5 |
| 2. | Thinking Slow | 18.75 | 14. | Physically Tired | 31.25 |
| 3. | Dizzy | 68.7 | 15. | Nervous | 6.25 |
| 4. | Faint | 37.5 | 16. | Sleepy | 62.5 |
| 5. | Warm | 68.7% | 17 | Restless | 25 |
| 6. | Numbness | 31.25 | 18. | Headache | 37.5 |
| 7. | Tingling | 25 | 19. | Irritable | 12.5 |
| 8. | Hands Shaking | 18.75 | 20. | Concentration Off | Not Applicable as |
| 9 | Palpitations | 43.75 | 21. | Coordination Off | Subjects were not |
| 10. | Vision Dim | 6.25 | 22. | Making Mistakes | performing any tas |
| 11. | Short of Breath | 75 | 23. | Mentally Tired | during the study |
| 12. | Weak | 0 | 24. | Reaction Slow |
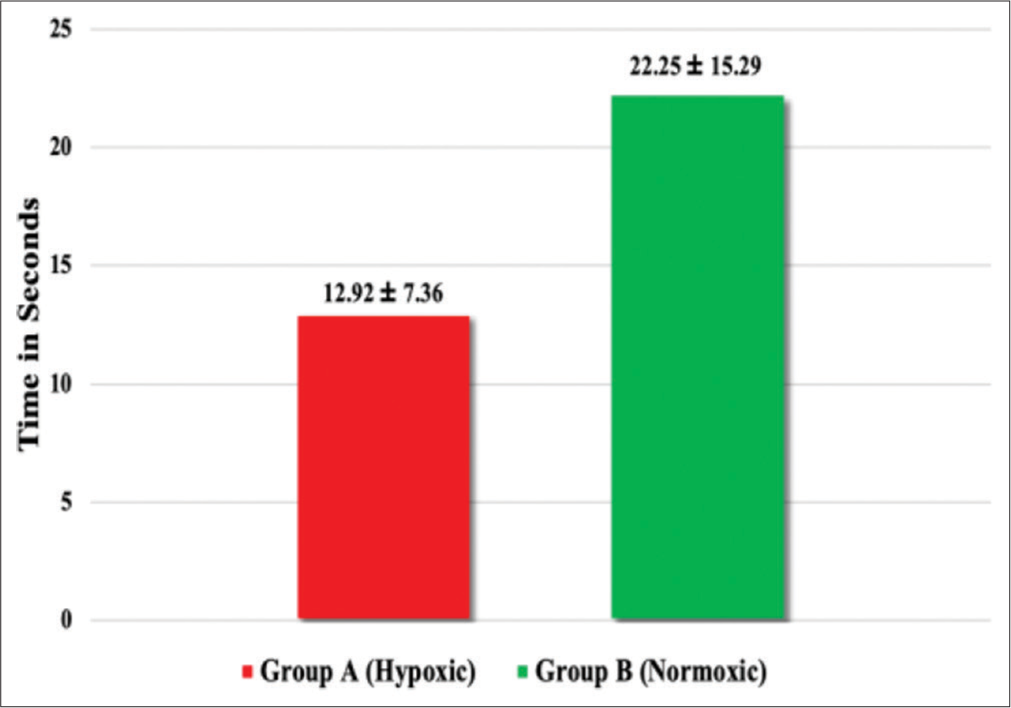
- Mean autokinesis time (s) hypoxia versus normoxia.
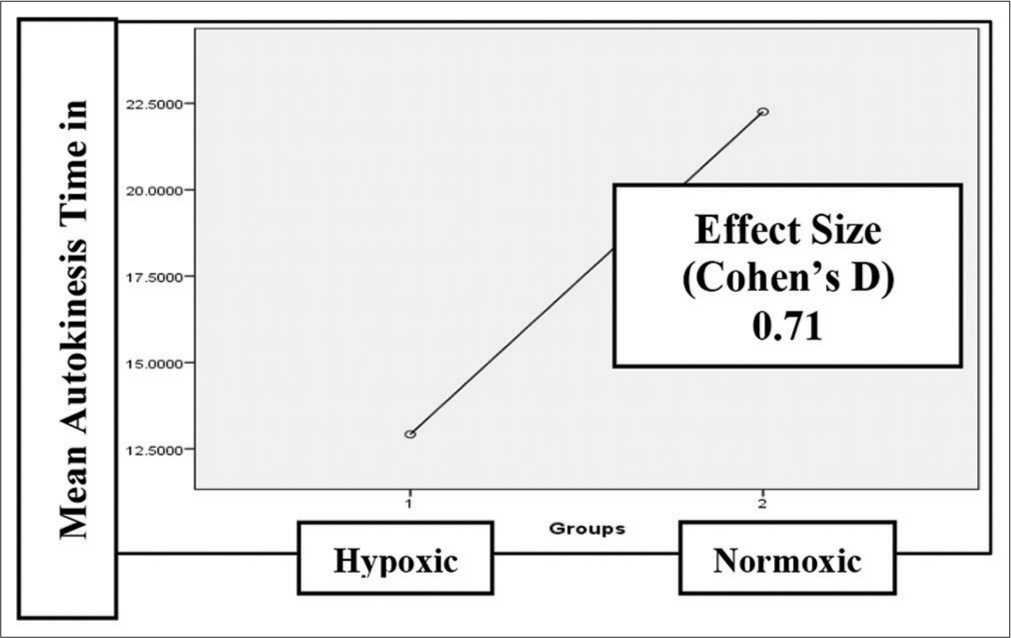
- Effect size for mean autokinesis time.
The mean scores of VAT recorded in four different conditions; acceleration and deceleration in clockwise and counterclockwise turns, referred to as VAT1, VAT2, VAT3, and VAT4, respectively, for both the groups are presented in Figure 3, and effect size in Figure 4. There was no significant difference in the VAT in clockwise and counter-clockwise yaw rotation (F = 0.207, P = 0.892). However, the mean VAT showed a significant reduction in hypoxic vi-a-vis normoxic condition (F = 5.989, P = 0.016).
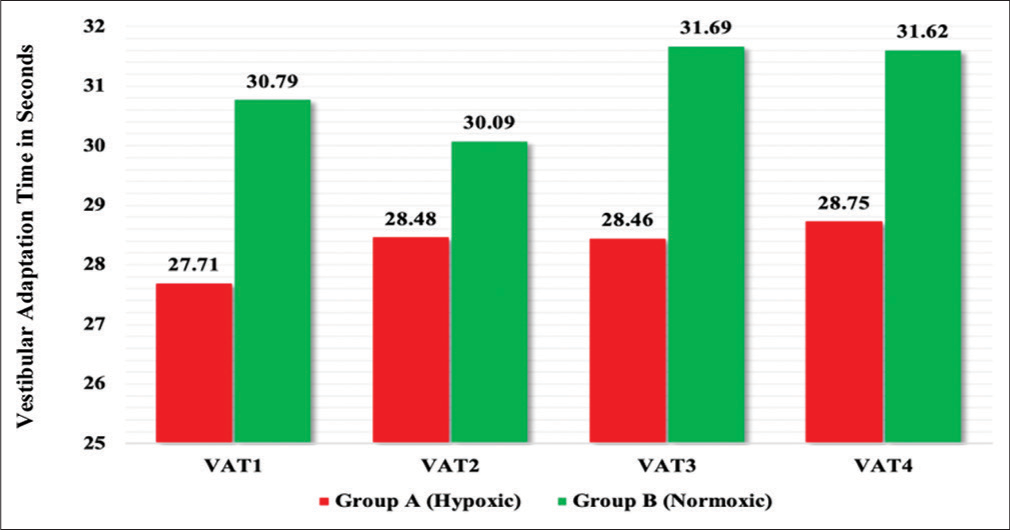
- Mean scores of vestibular adaptation time (s) between hypoxic group and normoxic group.

- Vestibular adaptation time effect size between hypoxic group and normoxic group.
DISCUSSION
This experiment was conducted to assess the effect of acute NH on its propensity for SD. Time for AT and VAT during acceleration and deceleration in both clockwise and counterclockwise turns was used as surrogate for SD. A double-blind randomized control study was designed and a total of 32 age-matched and BMI-matched subjects (16 each in hypoxic and normoxic groups) participated. The hypoxic group was exposed to NH by means of providing a mixture of nitrox gas simulating an equivalent altitude of 22,000 ft (FiO2 9.1%); whereas normoxic group was exposed to normal air.
In our study, we chose to simulate NH simulating an altitude of 22,000 ft as the testing condition. This was because, helicopter flying in high altitude operation does not exceed beyond this altitude. Further, simulating normobaric conditions, we did not intend to expose our subjects to serious ill effects of hypobaria, namely, decompression sickness. The advantages of normobaric over hypobaric hypoxia have been well documented in literature. Study by Kumar et al. at this institute has concluded the usability of NH simulation even in hypoxia indoctrination of aircrew.[9,10] The symptoms of hypoxia could be reproducible in normobaric conditions similar to hypobaric hypoxia. The results of our study also brought out almost all symptoms of hypoxia in varying manifestations [Table 1]. We did not include SpO2 as an absolute measure of hypoxia as the reliability of pulse oxymeter with the oxygen saturation below the critical value was questionable and hence, might not reflect the true physiological compromise due to hypoxia.[11]
Although the participants in our study were non-aircrew, the mean AT in normoxic conditions was similar to that reported by Sannigrahi et al. among aircrew subjects.[12] This indicates that individuals, whether aircrew or nonaircrew, are equally susceptible to onset of autokinesis.
Even though the exact mechanism of autokinesis is not understood, it is suggested that autokinesis may occur due to involuntary drifting of the eyes due to inadequate and inappropriate vestibular stabilization, as well as that checking the drift necessitates unrecognized oculomotor efferent activity which has sensory correlates that create the illusion.[13-15] The results of our study clearly indicated a significant reduction in mean AT in hypoxic conditions compared to normoxia. This implies that hypoxia tends to make individuals more prone to the autokinetic illusion by reducing the time for onset of autokinesis. In an operational setting, if the aircrew are flying at higher altitudes without supplementary oxygen, they need to be instructed to shift the gaze much more frequently and avoid prolonged fixation on the target source of light and should monitor the flight instruments to help resolve the conflict in perception.
Majority of studies on VAT or vestibular adaptation have been investigated in clockwise rotation only.[16,17] During the course of training given to flying cadets, aircrew and non-aircrew in the Disorientation Simulator at IAM IAF, there has been an anecdotal experience that the “coriolis effects” experienced during counter-clockwise turns were not the same as clockwise turns. Hence, in this study, VAT was noted in both clockwise and counterclockwise turns. However, no significant difference was observed in the VAT in clockwise and counter-clockwise yaw rotation, contrary to our belief.
Similar to AT, we observed a significant reduction in the mean VAT scores in hypoxic condition compared to normoxic condition. Although the effect size of various corresponding mean VAT scores between hypoxic and normoxic groups were small to medium, there was a reduction in the mean VAT scores in the hypoxic group [Figure 4]. Another finding in the study which was considered important, though not statistically significant, was a higher value of VAT scores during deceleration compared to that during acceleration in hypoxic condition [Figure 4]. The changes in the VAT could be attributed to the effects of hypoxia on ability of the vestibular system to adapt to the motion environment. The reduction in mean VAT scores in the hypoxic conditions and the apparent increase in VAT scores during deceleration may mean that hypoxia does have an effect on the vestibular system. This also means that the reduction in AT in the hypoxic group may also possibly be due to the involvement of the vestibular system. Since hypoxia is known to affect the neurological system, the reduction in AT could also have been due to the involvement of the oculomotor system as has been suggested earlier in the mechanism of autokinesis. We could not comment on the exact mechanism within the scope of the present study.
CONCLUSION
A significant reduction in AT indicates that hypoxia may increase the onset of autokinesis early. The changes in VAT in hypoxic conditions bring out a possible effect of hypoxia on the adaptability of the vestibular system in the angular motion environment.
Acknowledgment
We are thankful to Dr Rahul Pipraiya who had immense contribution in conceiving the study and planning the protocol. We are also thankful to technical staff in the Department of Acceleration Physiology and Spatial Orientation, Institute of Aerospace Medicine, Indian Air Force to help conduct the study.
Declaration of patient consent
The authors certify that they have obtained all necessary consent from the participants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Hypoxia and hyperventilation In: Ernsting J, Rainford DJ, Gradwell DP, eds. Aviation Medicine (5th ed). Oxford: Butterworth Heinemann; 2016. p. :49-63.
- [Google Scholar]
- Hypoxia: The silent operator in helicopter flying. Indian J Aerosp Med. 2001;45:76-82.
- [Google Scholar]
- Aircraft accidents on Indian army aviation-a general review since its inception. Indian J Aerosp Med. 2010;54:7-12.
- [Google Scholar]
- Hypoxia and coriolis illusion in pilots during simulated flight. Aerosp Med Hum Perform. 2016;87:108-13.
- [CrossRef] [Google Scholar]
- Flying in high altitude areas: An operator's view point. Indian J Aerosp Med. 1994;38:22-4.
- [Google Scholar]
- Survey of aircraft accidents over Siachen glacier. Indian J Aerosp Med. 1992;36:32-4.
- [Google Scholar]
- Spatial disorientation: Decades of pilot fatalities. Aviat Space Environ Med. 2011;82:717-24.
- [CrossRef] [Google Scholar]
- A Comparative Study of Hypoxia Induced by Hypobaric Chamber Training Viš-A-Viš Normobaric Reduced Oxygen Breathing Device in Normal Healthy Individuals as Hypoxia Awareness Training Tool. Dissertation for Doctor of Medicine. Rajiv Gandhi University of Health Sciences;
- [Google Scholar]
- Hypobaric and normobaric hypoxia training in aircrew: A comparative study. Indian J Aerosp Med. 2013;57:28-36.
- [Google Scholar]
- Autokinesis illusion in fighter flying revisited. Indian J Aerosp Med. 2020;64:56-61.
- [CrossRef] [Google Scholar]
- Visual illusions in flight In: Zarchan P, Previc FH, Ercoline WR, eds. Spatial Disorientation in Aviation (1st ed). Virginia: American Institute of Aeronautics and Astronautics; 2004. p. :283-322.
- [CrossRef] [Google Scholar]
- Spatial orientation in flight In: Jefferey RD, Johnson R, Stepanek J, Fogarty JA, DeHart RL, eds. Fundamentals of Aerospace Medicine (4th ed). Philadelphia, PA: Williams and Wilkin; 2008. p. :142-205.
- [Google Scholar]
- Optics and vision In: Ernsting J, Rainford DJ, Gradwell DP, eds. Aviation Medicine (5th ed). Oxford: Butterworth Heinemann; 2016. p. :263-80.
- [Google Scholar]
- An assessment of neuro-vestibular function elicited by motion in yaw axis in differently trained individuals following simulated microgravity In: Dissertation for Doctor of Medicine. Rajiv Gandhi University of Health Sciences; 2020.
- [Google Scholar]
- Comparative Study on Vestibular Adaptation Time and Psychological Parameters at Different Rates of Angular (Yaw) Motion. In: Dissertation for Doctor of Medicine. Rajiv Gandhi University of Health Sciences; 2019.
- [Google Scholar]






