Translate this page into:
Antihypertensives in Fighter Flying: IAF Experience
Abstract
Background:
Fighter flying is a highly stressful job that requires optimal physical and mental fitness. With the advent of highly maneuverable and agile fighter aircraft, the task of the aircrew has become more demanding. The global epidemic of life style diseases viz. hypertension, dyslipidemia is not only the concern of medical fraternity alone but of the Indian Air Force (IAF) too. Prevalence of hypertension in IAF aviator community is expectedly showing a rising trend. The use of antihypertensive drugs (Thiazide, ARB and ACE inhibitor) in fighter flying has recently been authorized in the IAF. However, follow up data is sparse.
Case Details:
A total of eleven fighter IAF pilots were incidentally detected with primary hypertension. They were evaluated according to the laid down procedures and guidelines of the organization. Necessary investigations were carried out to rule out any target organ damage. After initial observation in non-flying category, eight pilots were upgraded to restricted flying category after successfully withstanding ‘simulated aviation stresses’. They were further upgraded to almost full flying category with annual review at the nodal aeromedical center of the organization.
Discussion:
Long term use of antihypertensive medications and their adverse effect profiles in flying environment are required to be monitored at regular intervals to reduce the chance of sudden inflight incapacitation. Optimal performance in a stressful environment like a fighter cockpit needs to be ensured with regular follow-up data, cardiac profile and adverse effect profile (if any). In 82% cases ARBs were prescribed and in 36% cases existing antihypertensive drugs were changed to ensure compatibility with fighter flying. It has been re-emphasized that permitted medications are compatible with fighter flying and there has been no evidence of side effects or in flight problems. This evidence based approach strongly recommends continuation of the present policy to preserve trained manpower in the fighter squadrons.
Keywords
Antihypertensive medication
Fighter pilot
Flight safety
Evidence based approach
Introduction
Fighter flying requires high degree of physical and mental fitness. With the advent of highly maneuverable and agile fighter aircraft it has become even more challenging. The global epidemic of life style diseases viz. hypertension, dyslipidemia is not only the concern of medical fraternity alone but of the Indian Air Force (IAF) too. It is worth mentioning that well controlled blood pressure is almost never a risk factor for sudden incapacitation rather it is the secondary complications of hypertension that are of aeromedical significance. The increased prevalence of hypertension in both military and civil aircrew is a matter of concern. This has resulted in the employability restrictions for aircrew and financial loss to the state. The successful trials of newer and safer drugs have encouraged the use of these drugs in fighter aircrew across the globe. Recently, the Indian Air Force has authorized use of certain antihypertensive drugs [Thiazide, Thiazide type diuretics, Angiotensin Receptor Blockers (ARBs) & Angiotensin Converting Enzyme Inhibitor (ACEi)] in fighter flying. Though the present follow up data is sparse but the positive results are encouraging and have boosted the confidence of the organisation regarding the use of antihypertensive medications in fighter aircrew. The aim of this study is to critically analyse the follow-up data as well as the flying experience, disability profile and metabolic profile. An attempt has been made to find out the correlation of hypertension with other factors and discuss the aeromedical implications of anti-hypertensives use amongst fighter aircrew.
Hypertension: Potential hazards & aeromedical implications
Hypertension, the most prevalent risk factor for arterial disease in the industrialized world [1], is a frequently encountered clinical condition among the aircrew. Arterial systolic and diastolic blood pressures are continuous variables that can be influenced by a host of extraneous factors. It is an established fact that various physiological factors viz. stress, anxiety, exercise, diet, posture, ambient temperature etc can elevate blood pressure even in the absence of any organic pathology.
The Eighth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-8) offers excellent background information as well as recommendations for classification, risk stratification and therapy. It mentions that ‘Pre-hypertension’ is not a disease, but it identifies those who are likely to progress to Stage 1 or Stage 2 HTN in the future [3, 4]. This classification of hypertension is listed in Table 1 below:
| Category | Systolic (mmHg) | Diastolic (mmHg) | |
|---|---|---|---|
| Normal | <120 | And | <80 |
| Pre-hypertension | 120-139 | Or | 80-89 |
| Stage I hypertension | 140-159 | Or | 90-99 |
| Stage II hypertension | ≥ 160 | Or | ≥ 100 |
Diagnosis of HTN should be based on atleast three blood pressure readings taken on different days. Attempts should be made to measure the blood pressure in controlled and standardized conditions [5]. Evidence from clinical trials indicate that antihypertensive medications should be initiated in patients less than 60 years old if the systolic BP is persistently >140 mmHg and the diastolic BP is persistently >90 mmHg despite non-pharmacological therapy [6, 7]. The existing aeromedical guidelines of the organisation mandate absence of target organ damage viz., hypertensive retinopathy, hypertensive nephropathy etc for categorizing an aviator in Stage I HTN.
24-hour Ambulatory Blood Pressure Monitoring (ABPM), is the best tool to rule out White coat HTN, but is not being used extensively as a diagnostic tool at present. Number of studies have supported the use of ABPM for assessing the risk of coronary events [8, 9]; any deviation from the normal pattern of BP fall or/ ‘dipping’, during sleep significantly aggravates the risk [9]. White coat HTN could be relatively benign in the short term [9] but studies have shown that it is of high concern for long-term risk of developing sustained HTN [10, 11]. Systolic BP is considered as powerful risk predictor than diastolic BP. It has been estimated that for each 10 mmHg rise in systolic BP, there is an associated 30% increase in coronary mortality risk. The cardiovascular diseases have been ascribed as the single most common medical cause for termination of career in civil aviation industry as well [12]. Reassuringly, numerous therapeutic trials have demonstrated that effective treatment of HTN reduces the risk substantially and relatively rapidly [13]. The effect of treatment is greatest and realized most rapidly for stroke, but there is also good evidence for a reduction in coronary events of the order of at least 25 per cent with effective management of hypertension [5].
With the change in the life style and increasing trend of ‘Metabolic syndrome’, constant medical review of aircrew is deemed essential. Fighter flying being quite strenuous and requiring very high level of fitness, a further cautious approach is required for permitting a pilot to fly in the high risk environment with a clinical condition like this. Long term use of antihypertensive medications, their adverse effects, especially in flying environment needs to be monitored at regular intervals to reduce the risk of sudden in-flight incapacitation.
Antihypertensive drugs for fighter flying: Desired qualities
The antihypertensive drugs should have following desirable qualities to make them compatible for fighter flying:
To be administered by oral route only
Devoid of side effects that may cause distraction during flying viz. itching, nausea, headache etc.
It should not compromise sensory, motor, coordinative, basal ganglionic and higher mental functions.
It should not compromise +Gz tolerance, cardiovascular and autonomic reflexes involved in maintenance of blood pressure during G exposure.
Commonly prescribed antihypertensive drugs: Aeromedical implications
Diuretics: Diuretics are considered as a very safe class of drugs. However, in some instances it is known to cause hypokalemia induced cardiac arrhythmias besides causing increased frequency of urination. Loop diuretics cause hypokalemia more commonly and to a larger extent as compared to thiazide diuretics [14]; hence loop diuretics are not compatible with the aviation duties while thiazide can be permitted for flying only if serum potassium levels are monitored frequently and timing of the drug intake is such that diuretic effect is during non-flying hours. Carbonic anhydrase inhibitors due to lower potency and uncommon oral use are not permitted in fighter flying.
Angiotensin Converting Enzyme (ACE) inhibitors: ACE inhibitors are widely used in general population as well as flying due to their safety record. The only side effect is dry cough (rarely) which does not affect all people and hence unlikely to be a major cause of concern [15]. Few studies on fighter aircrew have suggested that they can reduce +Gz tolerance [16]. However, this has not been borne out in actual practice.
Angiotensin Receptor Blockers (ARBs): ARBs are also considered as a safe class of antihypertensives due to their negligible side effects. They have shown efficacy which is comparable to ACE inhibitors but avoid the side effects such as cough [17]. Except for uricosuria with Losartan, they appear to have neutral metabolic effects as well [18]. They are unlikely to reduce +Gz tolerance and are thus permitted for fighter flying.
Calcium Channel Blockers (CCBs): CCBs are not permitted in fighter flying as they cause direct relaxation of vascular tone and thus affect the +Gz tolerance of the aircrew.
Sympatholytics: Alpha blockers carry significant risk of postural drop in BP, thus likely to reduce +Gz tolerance. Beta blockers reduce HR, hence decrease cardiac output and in addition it is known to cause fatigue and impotence. Due to significant vasodilator effect, it can also cause reduction in +Gz tolerance. Such a profile of adverse effects makes this class of antihypertensives a poor choice for aviators [15].
Alpha 2 agonist: This group of drug is not permitted in fighter flying due to potential side effects viz., sedation, drowsiness, depression, degradation of psychomotor performance etc [19].
Other classes (Direct vasodilators, Ganglion blockers, Potassium channel openers, Renin inhibitors): These group of antihypertensives are also not permitted in fighter flying due to potential side effects and uncommon oral use.
Thus, the recommended drugs which can be prescribed for fighter aircrew includes Thiazide diuretics, ACE inhibitors and ARBs only.
International considerations
The USAF has permitted unrestricted high performance aircraft flying with use of single drug from the group of diuretics (Thiazide with/ without Triamterene), ACE inhibitors (Lisinopril or Ramipril) and ARBs (Losartan or Telmisartan) [20]. Concerns that ACE inhibitors might have an adverse effect on +Gz tolerance have not been borne out by experience in the US Air Force [21]. With ACE inhibitor (Lisinopril), aviator flying high performance aircraft needs to undergo centrifuge testing as soon as possible once BP is controlled [21]. The US Navy accepts these agents for high performance aircraft flying without mentioning the requirement of G-tolerance testing [22].
IAF guidelines
The IAF has permitted fighter aircrew to fly on antihypertensive medications which includes Thiazide diuretics, Thiazide type diuretics, ACE inhibitors (e.g. Enalapril 20 mg/ day: max dose) and ARBs. The laid down guidelines for evaluation, treatment and disposal of hypertensive fighter aircrew includes nonpharmacological remedies viz. dietary modifications like salt & alcohol restriction, weight reduction and regular exercise with careful evaluation during annual medical examinations for pre-hypertension class. However, aircrew with Stage I HTN without any co-morbidities, any target organ damage and on single drug therapy can be upgraded to restricted flying category after initial observation in ground category for 12 weeks to observe for any side effects and idiosyncratic reactions. Prior to the upgradation, BP should be well controlled on medications without any evidence of side effects of the drug and the aircrew should have successfully completed the High G training profile in centrifuge at IAM, Bangalore. This High G training profile includes centrifuge exposure at 9G for five seconds. Subsequently the aircrew can be further upgraded to almost full flying category. Thereafter, the aircrew is recommended for annual review by Medicine specialist / Cardiologist for next five years at one of the nodal medical evaluation centre only. Since, Stage II HTN cases require combination/ multi drug therapy, hence they are deemed unfit for fighter flying.
Need for centrifuge run before return to cockpit
Diuretics are known to cause hypokalaemia which may result in cardiac arrhythmia, especially on exposure to +Gz stress. However, the chance of hypokalemia with Thiazide or/ Thiazide type diuretics is remote. Studies have also suggested that ACE inhibitors can reduce +Gz tolerance thus affecting the aviator’s capability to withstand the +Gz stress. Hence, a check for G tolerance and endurance would be deemed appropriate for all cases on antihypertensives prior to declaring them fit for the fighter cockpit [5]. At present, IAF database on the detailed effects of drugs under high +Gz conditions is lagging due to small sample size. It is worth mentioning that the response of drugs may vary with ethnicity and genetic predisposition. Thus, it is prudent to progress with an evidence based approach by assessing the G tolerance and the response of drugs under high G stress in Indian ethnic group before declaring them fit for fighter cockpit. The successful completion of 9G for five seconds ensures that the aircrew is at par with their drug free counterparts.
Our Experience
Since the inception of this policy IAM has evaluated 11 fighter pilots with Essential HTN till Jun 2016. The descriptive analysis of these cases is presented in Table 2 below:
| Age (Yrs) | Flying history (Current Aircraft/ Total flying hours) | Co-morbidities | Medication | Remarks |
|---|---|---|---|---|
| 50 | Mirage 2000/ 2250 hrs | Dyslipidemia | Ramipril 2.5 mg OD Atorvastatin 20 mg OD |
Gradually upgraded |
| 42 | MiG 21/ 1607 hrs | Overweight Fatty liver Gd II | Telmisartan 40 mg OD | Upgraded but found to have Fatty liver Grade II during 2nd follow up |
| 32 | MiG 21/ 650 hrs | Overweight | Losartan 50 mg OD | Upgraded |
| 40 | Su 30 MKI/ 2080 hrs | - | Losartan 50 mg OD | Upgraded |
| 25 | Hawk/ 260 hrs | Dyslipidemia | Losartan 50 mg OD Atorvastatin 10 mg OD | Upgraded, Recommended Statins on two occasions, restricted flying category for dyslipidemia in last follow-up |
| 38 | Jaguar/ 2500 hrs | - | Natrilx SR 1.5 mg OD | Upgraded |
| 39 | Heron (RPA)/ 1100 hrs | - | Telmisartan 20 mg OD | Upgraded |
| 44 | Jaguar/ 1296 hrs | - | Losartan 25 mg OD | Upgraded |
| 47 | Jaguar/ 2700 hrs | Dyslipidemia DM type 2 | Losartan 50 mg OD Atorvas 10 mg HS Metformin 500 mg OD |
Not subjected to centrifuge run due to co-morbidities Unfit for fighters |
| 39 | MiG-21/ 2300 hrs | DM type 2 CSOM (Right) with TM perforation Overweight |
Losartan 25 mg OD | Not subjected to centrifuge run due to co-morbidities Temporary unfit for fighters |
| 44 | MiG-27/ 2600 hrs | - | Losartan 50 mg BD | Incomplete HPHC evalua- tion due to unwillingness Unfit for fighters |
Amongst eleven fighter aircrew with potential for upgradation, two aircrew were not subjected to centrifuge run due to associated co-morbidities (DM type 2, CSOM with TM perforation) while one could not complete the required run due to fatigue and unwillingness and was thus declared unfit for fighters. Rest eight fighter aircrew who were subjected to centrifuge evaluation successfully achieved the required target of 9G for five seconds (Fig 1).
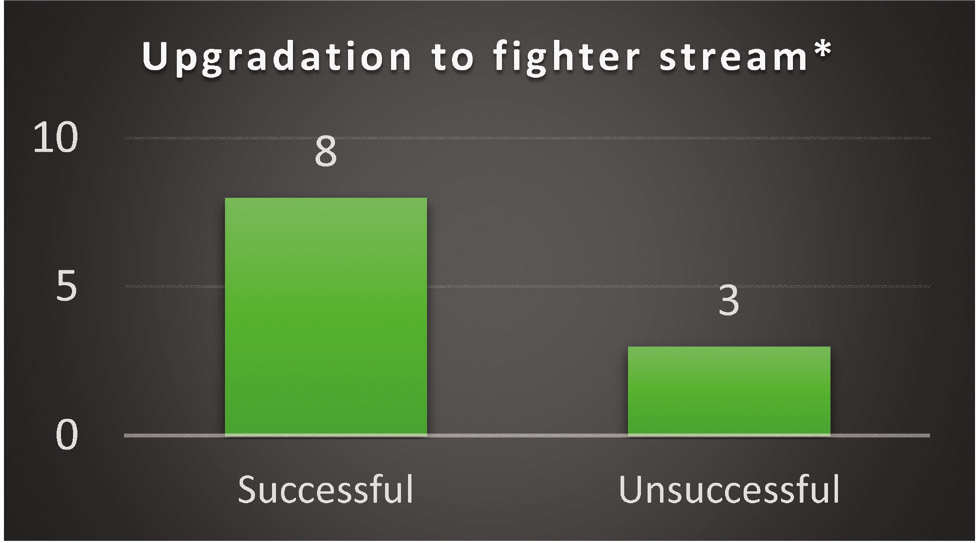
- Upgradation to fighter stream
- * Two pilots were not subjected to centrifuge run due to associated comorbidities and one pilot was unwilling for completing the target profile
The detailed analysis of the available data revealed that there is a higher prevalence of HTN in senior group of participants while overweight was found to be higher in relatively younger subjects. Dyslipidemia (27.3%), DM (9.1%) and overweight (36%) (18% overweight alone + 18% overweight with comorbidities) were found to be the associated co-morbidities. All the aircrew were advised life style modifications along with anti-hypertensive medications for optimal pharmacological outcome. Details of metabolic profile during upgradation is presented in Table 3 while Fig 2 depicts the prescribed antihypertensive medications.
| Ht (cm) | Wt (kg) | BMI (kg/m2) |
Overweight | Lipid profile (Total Cholesterol/ Triglyceride/ HDL/ LDL) |
|---|---|---|---|---|
| 170 | 69 | 23.87 | - | 195/ 147/ 53/ 113 |
| 170 | 81 | 28.02 | Yes | 165/ 110/ 46/ 97 |
| 174 | 78 | 25.76 | Yes | 197/ 103/ 49/ 127 |
| 175 | 78 | 25.46 | Yes | 215/ 130/ 69/ 129 |
| 176 | 76 | 24.54 | - | 196/ 137/ 64/ 105 |
| 166 | 68 | 24.67 | - | 168/ 106/ 47/ 99 |
| 185 | 77 | 22.49 | - | 168/ 85/ 43/ 108 |
| 174 | 75 | 24.77 | - | 195/ 126/ 49/ 121 |
| 165 | 61 | 22.40 | - | 152/ 93/ 45/ 88 |
| 175 | 83 | 27.12 | Yes | 190/ 106/ 43/ 126 |
| 169 | 68 | 23.8 | - | 176/ 110/ 49/ 105 |
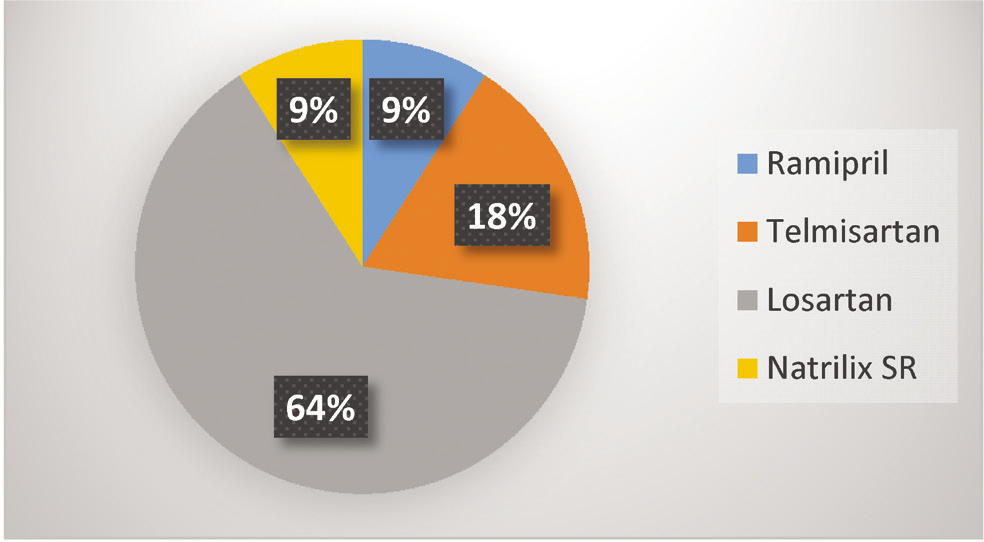
- Prescribed antihypertensive drugs
Co-morbidities in the aircrew are shown in Fig 3 while Fig 4 depicts the change of antihypertensives for fighter compatibility.
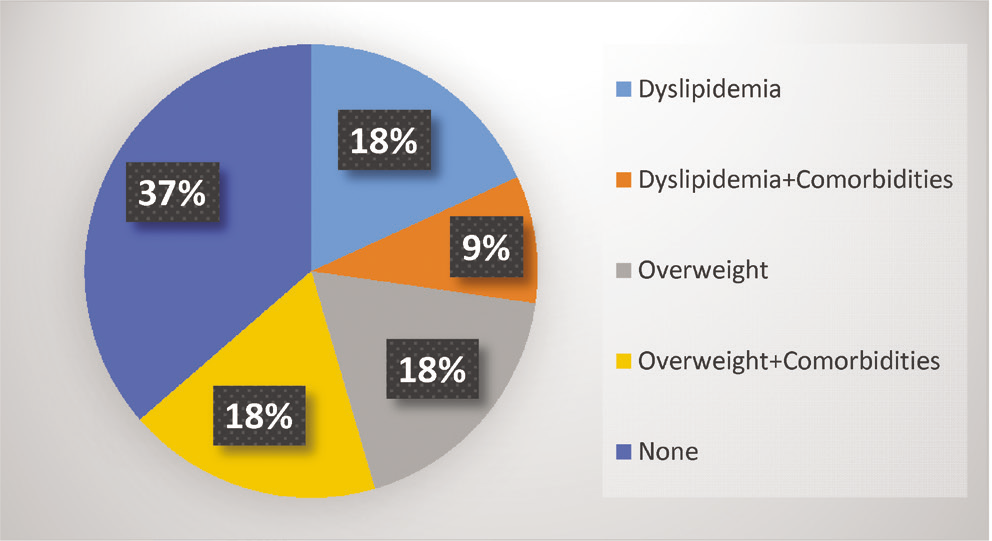
- Co-morbidities
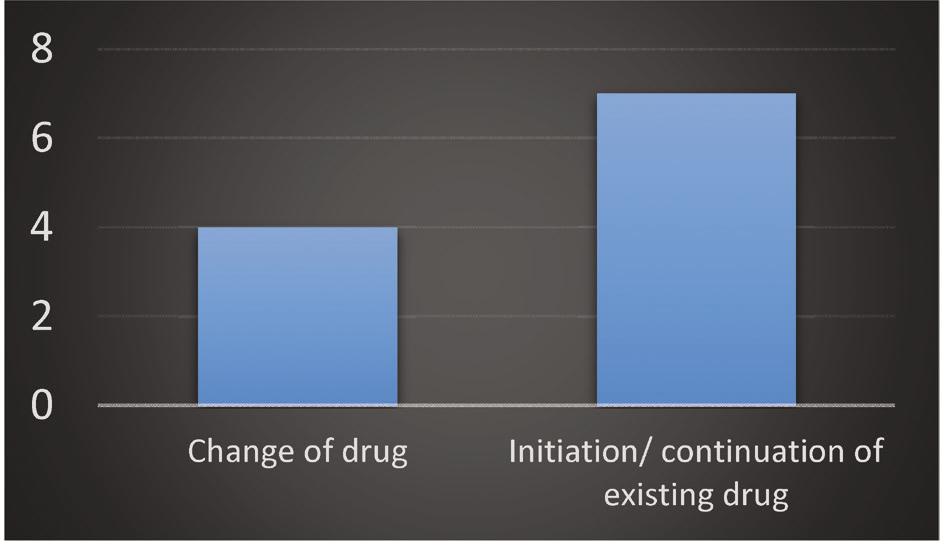
- Change of antihypertensives for fighter compatibility
Discussion
The amendment to existing guidelines for aircrew of IAF allows the use of specific anti-hypertensive medications in fighter flying. Amongst eleven fighter aircrew with potential to be upgraded to fighter flying, two aircrew were not subjected to centrifuge run due to associated co-morbidities and were declared unfit for fighter flying while one aircrew did not complete the required centrifuge run due to fatigue and unwillingness and thus was also made unfit for fighters. The aircrew who did not complete the centrifuge run was out of active flying for more than 10 years and this could be the reason for his poor physical conditioning resulting in inability to pull 9G. This aircrew was also not likely to come back to active flying due to his seniority and thus he chose not to give a further try after a period of observation and physical conditioning. At present the follow up data is scanty and thus it will be too early to make any conclusive remarks about the suitability of the drugs. However, the current analysis has shown a positive trend with favourable outcome. The aircrew were advised for regular follow up and it is expected that within a period of 2-3 years we may have adequate follow-up data.
Hypertension is more common amongst the obese and overweight than normal weight population and thus a significant proportion of hypertensive people in the general population are found to be overweight [23]. Cross-sectionally, higher weight is associated with higher BP levels and prospectively, baseline weight and weight gain predict higher BP. This suggests that weight gain may pathophysiologically contribute to BP elevation [24]. Correlation between dyslipidemia and HTN is also a well established fact [25] as is evident in the present study as well. Diabetes mellitus and HTN are inter-related diseases which strongly predispose an individual to atherosclerotic cardiovascular disease [26]. In this study, the correlation of associated co-morbidities viz. overweight, dyslipidemia, DM type 2 with HTN is in accordance with the existing literature.
In spite of this limited follow-up duration, it is worthwhile to mention that amongst the eight pilots who were upgraded to fighters, six pilots are carrying out their assigned duty quite comfortably. Two aircrew were placed in non-flying medical categories because of freshly detected co-morbidities. This fact stresses upon the necessity of lifestyle modifications and physical exercise over and above the use of antihypertensive medications. Hence, the onus of this downgradation cannot be put on the primary disease i.e. hypertension which is adequately controlled with the prescribed antihypertensives with favourable outcome in aviation scenario.
The result of this study, though encouraging, needs to be backed up with further follow up data and studies with a large number of subjects since the number of subjects were limited. Moreover, the existing policy of upgrading a hypertensive aircrew after 24 weeks also needs a relook in view of the pharmacokinetics of the antihypertensive drugs.
Conclusion
It can be safely inferred that the permitted medications are compatible with fighter flying and there has been no evidence of side effects with potential aeromedical implications. Though the present data is small but is good enough to boost the confidence of both Aerospace Medicine and aircrew fraternity. Further follow up of the existing cases and addition of new cases will support the evidence based approach and rationale of selecting the specific anti-hypertensive medications. It is strongly recommended to continue the present policy to preserve trained manpower in the fighter squadrons and their optimum utilization.
References
- Hypertension prevalence and blood pressure levels in 6 European countries, Canada and the United States. Journal of the American Medical Association. 2003;289:2363-2369.
- [Google Scholar]
- Clinical Aerospace Cardiovascular Medicine In: Dehart RL, ed. Respiratory Physiology. Fundamentals of Aerospace Medicine. 1985. p. :331.
- [Google Scholar]
- Hypetension In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, eds. Pharmacotherapy: A pathophysiologic approach Vol 3. (9th ed). New York: McGraw-Hill Medical; 2014.
- [Google Scholar]
- Essential hypertension In: Alldredge BK, Corelli RL, Ernst ME, Guglielmo BJ, Jacobson PA, Kradjan WA, Williams BR, eds. Koda-Kimble and Young’s Applied Therapeutics: The Clinical Use of Drugs Vol 14. (10th ed). Philadelphia: Lippincott Williams & Wilkins; 2013.
- [Google Scholar]
- 2014; Evidence based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8) 2014. JAMA [Internet]. [cited 2015 Jan 26]; 311(5) 507-520 Available from: http://jama.jamanetwork.com/article.aspx?articleid=1791497 Accessed on 30 Oct 16
- [Google Scholar]
- Overview of hypertension in adults. UpToDate [Internet]. Philadelphia: Wolters Kluwer Health [updated 2015 Jan, cited 2015 Jan 26]. [About 15p.]. Available from: http://www.uptodate.com/contents/overview-of-hypertensionHTN-inadults?source=search_result&search=hypertensionHTN&selectedTitle=1%7E150#H28 Accessed on 30 Oct 16
- [Google Scholar]
- Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Journal of the American Medical Association. 1999;282:539-546.
- [Google Scholar]
- Ambulatory blood pressure: An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793-801.
- [Google Scholar]
- Isolated office hypertension: A prehypertensive state? Journal of Hypertension. 1996;14:327-332.
- [Google Scholar]
- White-coat hypertension as a cause of cardiovascular dysfunction. Lancet. 1996;348:654-657.
- [Google Scholar]
- International regulation of medical standards In: Ernsting’s Aviation Medicine (Fourth). p. :556-562.
- [Google Scholar]
- Blood pressure, stroke and coronary heart disease: part 2. Lancet. 1990;335:827-838.
- [Google Scholar]
- The efficacy and safety of diuretics in treating hypertension. Ann Intern Med. 1995;122:223-226.
- [Google Scholar]
- Antihypertensive Drugs in Aircrew. In Medication for Military Aircrew: Current Use Issues and Strategies for Expanded Options. RTO Technical Report. 2001;14:5-14.
- [Google Scholar]
- The effect of Captopril on +Gz tolerance of normotensives. Aviat Space Environ Med. 1992;63:706-708.
- [Google Scholar]
- Experience with angiotensin II antagonists in hypertensive patients. Clin Exper Pharmacol Physiol 1996(Suppl 3):S99-104.
- [Google Scholar]
- Angiotensin II antagonists: efficacy, duration of action, comparison with other drugs. J Human Hypertens. 1998;12:271-274.
- [Google Scholar]
- Psychomotor performance and antihypertensive treatment. Br J Clin Pharm. 1994;37:165-172.
- [Google Scholar]
- Lisinopril for the treatment of hypertension in aviators. www.dtic.mil/cgi-bin/GetTRDoc?AD=ADA361212 Accessed on 16 Dec 16
- [Google Scholar]
- Overweight and Hypertension: A Review. http://circ.ahajournals.org/content/39/3/403.short Accessed on 25 Sep 16
- [Google Scholar]
- Lipitension: Interplay between dyslipidemia and hypertension. Indian J Endocrinol Metab. 2012;16(2):240-245.
- [Google Scholar]
- Diabetes Mellitus and Associated Hypertension. Vascular Disease, and Nephropathy. http://hyper.ahajournals.org/content/26/6/869 Accessed on 25 Sep16
- [Google Scholar]






