Translate this page into:
Analysis of cardiovascular responses to head-up tilt testing

*Corresponding author: Dr M Kaur, MBBS, Resident in Aerospace Medicine, Institute of Aerospace Medicine IAF, Vimanapura, Bengaluru - 560 017, Karnataka, India. manucore17@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur M, Sinha B, Raju AVK. Analysis of cardiovascular responses to head-up tilt testing. Indian J Aerosp Med 2020;64(2):62-7.
Abstract
Introduction:
Head-up tilt (HUT) testing is a widely accepted tool in the clinical evaluation of patients presenting with episodic loss of consciousness. The test has assumed its importance in aviation environment, where a single episode of unconsciousness in-flight may have a catastrophic outcome. To rule out this, HUT is carried out in all cases of syncope as a part of aeromedical evaluation. The present study was undertaken to analyze the CVS response to HUT conducted over a period of 11 years at the Department of Space and Environmental Physiology at the Institute of Aerospace Medicine.
Material and Methods:
A total of 168 subjects had undergone HUT testing from 2002 to 2012. The testing equipment was a standard tilt table with a foot board support for the feet and restraint system at the level of chest, waist, and ankle to support the body during tilting. The testing protocol consisted of passive tilting to an angle of 70° from the horizontal position for 45 min in all the cases. The physiological parameters consisting of heart rate (HR) and blood pressure from the database were analyzed to understand the CVS response to HUT.
Results:
Out of the total 168 patients, 147 (88.5%) cases showed normal response. Twenty-one (12.5%) cases showed abnormal response. Out of the cases showing abnormal response, 14 cases had syncope with frank loss of consciousness and could not maintain the postural tone. The remaining seven cases showed postural orthostatic tachycardia syndrome (POTS), where the HR increased by more than 30 beats per minute.
Conclusion:
A retrospective analysis of 168 cases with history of syncope, in a period of 11 years, revealed an abnormal cardiovascular response to HUT in 12.5% of cases. The abnormal physiological responses were mostly consistent with syncope and POTS.
Keywords
Head-up tilt test
Neurocardiogenic syncope
Episodic loss of consciousness
Orthostatic stress
Postural orthostatic tachycardia syndrome
INTRODUCTION
Syncope is a sudden transient loss of consciousness with an inability to maintain the postural tone. The hemodynamic instability results from an acute fall in systolic blood pressure (BP) from normal to <70 mmHg or in mean arterial pressure to <40 mmHg, causing a transient cessation of cerebral blood flow for more than 8 s and temporary loss of consciousness.[1]
When the healthy individuals assume the upright position, gravity driven venous blood pooling causes decreased ventricular preload. As a compensatory mechanism, there is an increase in heart rate (HR) and Blood Pressure (BP) due to the activation of sympathetic neural system and inhibition of parasympathetic neural input. The normal physiological response to orthostatic stress is small increase in HR, a slightly decrease in BP and an elevated diastolic BP (DBP).[2] Excessive sympathetic stimulation in susceptible individuals may sometimes lead to withdrawal of sympathetic neural activity and reinforcement of vagal activity and this ultimately results in hypotension and bradycardia or both, which may lead to cerebral hypoperfusion leading to loss of consciousness.
Sudden transient loss of consciousness is dangerous for personnel involved in the high-risk settings such as aviation environment both military and civil, commercial painting, and marine diving. The high-risk group with a history of episodic loss of consciousness is thus required to be comprehensively evaluated. Head-up tilt (HUT) testing has become a widely accepted tool in the clinical evaluation of patients presenting with episodic loss of consciousness. At present, there is a substantial agreement that tilt table testing is an effective technique for providing direct diagnostic evidence indicating susceptibility to neurocardiogenic syncope.[3]
The purpose of the present retrospective study was to make a physiological assessment of the cardiovascular responses to tilt testing in the aircrew and others who underwent the HUT test in the Department of Space and Environmental Physiology at the Institute of Aerospace Medicine, Indian Air Force (IAM IAF) from 2002 to 2012.
MATERIAL AND METHODS
The present study was a retrospective analysis of the HUT test data carried out in the space and environmental physiology at IAM IAF from 2002 to 2012.
Subjects presenting with a history and clinical examination consistent with the diagnosis of syncope reported to the department were included in the study. Test prerequisite characteristics included a normal physical examination, electrocardiogram (ECG), echo-cardiogram, and a negative history of heart disease, seizures, or cardiac medications. Other causes of loss of consciousness were ruled out by carrying out hematological, biochemical, neurological, and psychological causes that may trigger syncope.
Akron Multipurpose Automatic Tilt Table (Model 9622, Huntleigh Akron, UK), an electronically operated tilt table with foot support was used for the HUT testing. The tilt angle of the table could be varied from 0° to 90° in 13 s duration by a hydraulic system. Three restraints were gently but securely attached to the patient’s chest, waist, and ankle regions to minimize the undesirable movement as well as to prevent falling of the subject in case of unconsciousness during the conduct of the test.
HR and BP of the patient were recorded by a Patient Monitor (KMA 900, Turkey). Single-lead electrocardiography was performed by attaching three electrodes on the patient’s anterior surface of the chest. HR was derived from R-R interval of the ECG wave and was displayed online. ECG recording was done continuously during the test. Noninvasive BP was measured with an appropriately sized cuff placed on left upper arm. The BP was measured by oscillometric method in the patient monitor. The inflation of manometer cuff was set up in auto mode at 2 min interval. SBP and DBP were recorded and displayed online. BP was recorded every 2 min at baseline, during tilt and recovery.
Initially, the patient remained in the supine position for 10 min for recording of their baseline cardiovascular parameters. After baseline recording, the patient was tilted to 70° tilt angle from horizontal position with their foot rested on a foot support. Tilt test was continued for 45 min for patients with negative test outcome and terminated before 45 min for the patients who had a positive response. The positive responses to tilt were classified into two different types in the present study, namely, frank syncope and postural orthostatic tachycardia syndrome (POTS). The positive response was defined to be syncope, if the patient developed frank syncope along with bradycardia, hypotension, giddiness, nausea, light headedness, visual disturbance, palpitations, and diaphoresis. Patients who developed syncope were returned to the supine position and allowed to recover. After a positive HUT test, patients were allowed to rest till recovery to baseline status. During this period, patients remained supine or sitting. The POTS was defined as the development of orthostatic symptoms that are associated with at least a 30 beat/min increase in HR or an absolute HR of ≥120 beats/min that occurs within the first 10 min of standing or upright tilt.[4]
The tilt test was carried out in the morning between 8 and 10 h in a dimly lit, sound attenuated room with the ambient temperature around thermo neutral zone (23–26°C). All the patients were tested in the morning hours following a overnight fast and restful sleep the previous night. The patients were familiarized with the test environment, equipment, and procedure. Written informed consent was obtained from each patient before conducting the HUT test on them. They were also explained the possible outcome of the tilt test and its consequences. They were asked to refrain from smoking and consuming coffee or tea 4 h before the test. They were also instructed not to consume alcohol in the previous night. They were advised to continue their routine medications they were taking, if any. However, certain drugs such as β-blockers, peripheral vasodilators, or any other drugs which are likely to interfere with the tilt test result were stopped for at least five half-lives before the test on consultation of the treating physician.
Data were analyzed using a professional statistical package Statistica 8.0. Data were first checked for normality by Shapiro–Wilks “W” Statistic. After ascertaining normality, HR and BP data were analyzed by one-way ANOVA and paired sample t-test. The level of significance was kept at P<0.05.
RESULTS
Out of the total of 168 cases, 92.8% (n = 156) were male and 7.2% (n = 12) were female. A total of 147 (85.5%) cases (male – 137; female – 10) showed a normal or negative response to HUTT, whereas 21 (12.5%) showed an abnormal or positive response. Out of these, 14 cases had frank syncopal attack (male – 12 and female – 2) and 7 cases showed POTS response (all males). Gender-wise outcome of HUT response is summarized in Table 1. The mean age of the male was 31.6 ± 10.94 years and that of female was 26.7 ± 12.58 years [Table 2].
| Gender | Negative response | Frank syncope | Postural orthostatic tachycardia syndrome | Total |
|---|---|---|---|---|
| Male | 137 | 12 | 7 | 156 |
| Female | 10 | 2 | 0 | 12 |
| Gender | Mean | SD | 95% CI | |
|---|---|---|---|---|
| Upper bound | Lower bound | |||
| Male | 31.6 | 10.94 | 29.85 | 33.31 |
| Female | 26.7 | 12.58 | 18.92 | 34.91 |
Number and percentage of positive cases as per time duration during which the hemodynamic instability occurred during HUT test are shown in Figure 1. The maximum number of positive cases was observed between 31 and 40 min (33%).
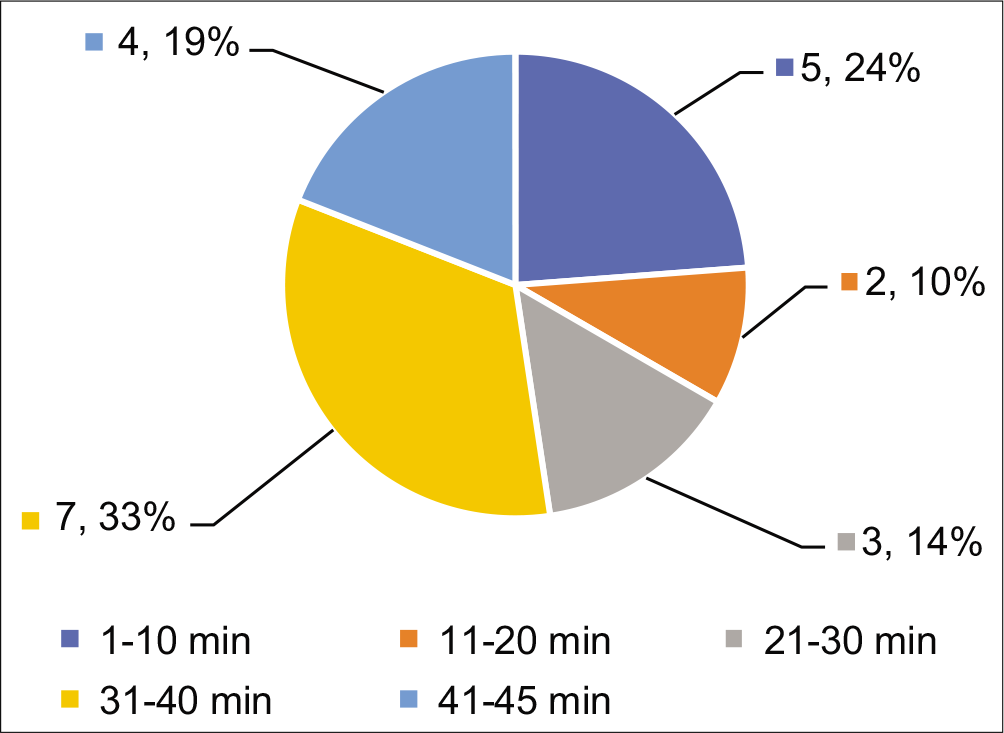
- Number and percentage of positive cases as per time duration of hemodynamic instability from start of tilt testing.
The next highest number of positive cases was found between 1 and 10 min (24%). Least number of positive cases was observed between 11 and 20 min (10%). Mean time of hemodynamic instability in individuals with outcome of POTS was about 28.3 ± 15.97 min, whereas the time to instability in cardiovascular parameters in positive cases was 26.7 ± 14.46 min.
Table 3 depicts the HR, SBP, and DBP responses during tilt test with variable outcomes. Values are given in mean ± SD. HR was significantly higher during tilt in individuals with POTS as compared to individuals showing normal or syncopal response. There was an average increase in HR by 40 bpm for cases showing POTS response as compared to an average increase in HR by 21 bpm and 20 bpm during syncopal and negative outcomes, respectively. There was a mean increase in SBP by 2 mmHg from baseline both during negative outcome and POTS. On the other hand, the SBP fell by 5 mmHg during syncopal outcome of tilt test. DBP increased on an average by 9, 3, and 6 mmHg, respectively, during tilt test with an outcome of negative, syncopal, and POTS, respectively. There was a greater narrowing down of PP in POTS (12 mmHg) as compared to negative outcome (7 mmHg) and syncopal outcome (8 mmHg). Furthermore, individuals with the development of POTS during tilt test had a higher resting baseline PP than the individuals with normal and syncopal outcome. MAP increased by 7 mmHg in individuals with negative outcome. MAP fall was highest in patients with syncopal outcome as compared to normal response. MAP increased on an average by 10 mmHg during POTS.
| Normal response | Syncope | POTS | ||||
|---|---|---|---|---|---|---|
| Baseline | HUTT | Baseline | HUTT | Baseline | HUTT | |
| HR (bpm) | 70.3±11.49 | 90.1±13.25 | 67.4±10.49 | 88.7±14.47 | 73.7±9.72 | 113.9±***/^^^7.61 |
| SBP (mmHg) | 123.7±14.14 | 126.0±12.62 | 116.1±12.09 | 111.2±15.71*** | 121.6±12.35 | 123.9±7.61 |
| DBP (mmHg) | 75.9±12.90 | 85.1±10.49 | 71.2±12.84 | 74.4±9.15*** | 72.3±7.54 | 78.8±10.55 |
| PP (mmHg) | 47.7±7.99 | 40.9±7.53 | 46.6±8.66 | 38.6±10.11 | 57.5±**/^^17.51 | 45.1±12.16 |
| MAP (mmHg) | 91.9±12.92 | 98.8±10.65 | 85.0±13.34 | 82.7±17.90*** | 83.2±19.42 | 93.2±11.80 |
The HR and BP response to tilt test in individuals with syncopal outcome during various phases of the tilt are shown in Table 4. Values are given in mean ± SD. Values within parentheses are the number of individuals who could complete the tilt test for such duration. There was a significant increase in HR during tilt from baseline continuously. During the last 5 min of tilt, there was a significant reduction in HR. SBP after an initial fall by 4 mmHg during the first 10 min of HUT increased by 4–5 mmHg during the next 20–30 min. SBP then started falling from 31 min onward. DBP increased by 4–8 mmHg during the first 20 min of tilt followed by slight attenuation during 31–40 min. However, DBP never decreased below baseline during tilt. There was a narrowing down of PP during tilt test and a significant narrowing down was observed during 41–45 min of tilt in POTS (20 mmHg↓). MAP when compared from baseline decreased by 2 mmHg during the first 10 min of tilt followed by an increase by 9 mmHg during 11–20 min. MAP decreased by 7 mmHg from baseline during 41–45 min of tilt test.
| Baseline (n=14) | 0–10 min (n=14) | 11–20 min (n=11) | 21–30 min (n=11) | 31–40 min (n=8) | 41–45 min (n=4) | ||
|---|---|---|---|---|---|---|---|
| HR (bpm) | 67.4±10.49 | 85.1±14.51*** | 89.5±16.74***$ | 93.7±18.54*** | 87.7±19.12*** | 62.9±15.74 | |
| SBP (mmHg) | 116.1±12.09 | 112.4±12.62 | 120.6±14.64 | 117.2±20.68 | 98.0±30.22 | 96.1±19.99 | |
| DBP (mmHg) | 71.2±12.84 | 75.2±9.99 | 80.0±8.53* | 73.6±12.95 | 73.2±13.49 | 72.0±7.89 | |
| PP (mmHg) | 46.6±8.66 | 38.1±9.86*** | 40.6±9.50* | 45.1±15.53 | 35.4±10.88* | 26.6±16.51* | |
| MAP (mmHg) | 85.0±13.34 | 83.0±17.69 | 93.5±10.00*$ | 87.2±16.71 | 85.0±16.21 | 78.3±9.34 | |
Table 5 shows HR and BP response to tilt test in individuals with negative outcome. There was a significant increase in HR during tilt from baseline continuously. During the last 5 min of tilt, there was a significant increase in HR from baseline by 23 bpm. SBP after an initial mean increased by 4 and 5 mmHg during the first 10 and 11–20 min of HUT, returned to baseline during 21–30 min, and maintained throughout tilt with a very little fluctuation. DBP increased by 10 and 11 mmHg during the first 10 min and 11–20 min of tilt. Thereafter, it varied by a little with a minor fluctuation of 2–5 mmHg. There was a significant narrowing down of PP during tilt test from baseline with a minor fluctuation of 1–2 mmHg throughout tilt. MAP increased significantly by 4–9 mmHg during tilt from baseline.
| Parameters | Baseline | 0–10 min | 11–20 min | 21–30 min | 31–40 min | 41–45 min |
|---|---|---|---|---|---|---|
| HR (bpm) | 70.3±11.49 | 86.9±13.54*** | 90.5±13.62***$$$ | 89.6±14.62*** | 92.3±15.71*** | 93.0±15.83*** |
| SBP (mmHg) | 123.7±14.14 | 127.7±15.45*** | 128.6±15.49*** | 123.0±12.09 | 125.5±12.22 | 127.3±13.47** |
| DBP (mmHg) | 75.9±12.90 | 86.0±14.10*** | 86.8±12.17*** | 82.1±10.77*** | 85.6±10.31*** | 87.3±12.68*** |
| PP (mmHg) | 47.7±7.99 | 41.6±7.88*** | 41.7±7.99*** | 40.8±8.52*** | 39.7±7.70*** | 39.6±10.32*** |
| MAP (mmHg) | 91.9±12.92 | 100.0±14.18*** | 100.8±12.76*** | 95.5±10.4*** | 98.9±10.26*** | 100.7±12.16*** |
HR and BP response in individuals who developed POTS during tilt test are shown in Table 6. Heart rate from baseline showed a mean increase by 34, 41, 42, 41, and 51 bpm during 0–10 min, 11–20 min, 21–30 min, 31–40 min, and 41–45 min of tilt test, respectively. SBP during tilt varied by about 2–6 mmHg from baseline. DBP always showed an increasing trend during tilt test. DBP increased by 6–18 mmHg during tilt test. There was a narrowing of PP during tilt test. PP fell by 11–18 mmHg during 45 min of the test. Mean arterial pressure showed an increasing trend over the period of tilt and increased by 6–16 mmHg during tilt.
| Parameters | Baseline (n=7) | 0–10 min (n=7) | 11–20 min (n=6) | 21–30 min (n=4) | 31–40 min (n=4) | 41–45 min (n=2) |
|---|---|---|---|---|---|---|
| HR (bpm) | 73.7±9.72 | 107.6±10.10*** | 114.8±13.26**$ | 116.1±7.79*** | 114.9±7.78** | 124.8±4.01*** |
| SBP (mmHg) | 121.6±12.55 | 125.4±14.73 | 119.7±20.38 | 125.1±17.57 | 121.5±16.09 | 127.2±29.93 |
| DBP (mmHg) | 72.3±7.54 | 79.5±9.48* | 78.9±14.53 | 85.7±7.53* | 78.9±13.21 | 90.0±28.28 |
| PP (mmHg) | 57.5±17.51 | 45.9±10.79 | 40.7±9.32 | 39.4±15.00 | 42.6±7.16 | 42.0±12.26 |
| MAP (mmHg) | 83.2±19.42 | 94.8±10.31* | 92.5±16.12 | 98.8±9.53 | 89.2±20.36 | 99.2±21.76 |
DISCUSSION
HUT is a sensitive and specific test to unmask the susceptibility to vasovagal reaction in patients with syncope of unknown origin.[5] The tilt testing has gained acceptance as a tool for assessing susceptibility to neurally mediated syncopal syndromes. Dikshit et al. suggested that 70° HUT test is extremely important to assess autonomic cardiovascular reflex status of individuals, especially the pilots and other professionals associated with high risk and having a history of syncope of unknown origin.[6] The American College of Cardiology/American Heart Association/Heart Rhythm Society and the European Society of Cardiology also advocate tilt table test for the diagnosis of syncope.[7,8] Very recently, researcher from Oklahoma Health Sciences Center, USA, has also reiterated the usefulness of tilt test for the diagnosis of neurocardiogenic syncope.[9]
On assuming upright posture, approximately 300–800 ml of blood is pooled toward dependent limbs due to gravity. About 25% of thoracic blood volume is rapidly displaced in the splanchnic and pelvic organs and lower extremities.[9,10] The shifting of blood toward dependent limbs causes a compensatory physiological change resulting in sympathetic activation and vagal inhibition which in turn, maintains the heart rate and BP. However, in some individuals, abnormal autonomic activity leads to bradycardia and hypotension ensuing cerebral hypoperfusion followed by syncope. The increase in HR by 20–21 bpm during orthostatic stress in individuals with negative outcome in the present study is similar to the findings reported by Dikshit,[11] Banerjee et al.,[12] and Tripathi.[13] These studies[11-13] have also documented an increase in SBP during orthostasis which is also in agreement with the findings of the present study. Sinha and Dubey reported an increase in HR by 19 bpm, SBP by <1 mmHg, DBP by 6 mmHg, and MAP by 10 mmHg during orthostatic stress for 10 min in endurance trained athletes.[14] Researchers from other countries have reported an increase in HR by 10–15 beat/min, a 5–10 mm Hg increase in DBP, and no change in systolic BP during normal response to tilt.[2,15]
Heart rate pattern during syncopal response was found to have an incremental pattern till 30 min of tilt which was followed by an opposing trend after 30 min. The HR did not show this kind of biphasic pattern in negative cases and was found to vary within 4–6 bpm throughout the tilt test. Comparatively, increase in HR in syncopal cases during the first 10–30 min of tilt was higher than negative cases. Attempts were made to predict the outcome of tilt test based on the changes in HR during early few minutes of tilt. Mallat et al. suggested that the heart rate increases ≤18 bpm during the first 6 min of tilt predicted a negative outcome with 100% specificity, 100% positive predictive value, and 88.6% sensitivity.[16] Movahed suggested that that failure to increase the heart rate equal to or <18 bpm during the first 10 min of HUT test can predict low probability of syncope.[17] During the first 10 min of tilt, our subjects with syncopal outcome exhibited an increase in HR by 18 bpm, whereas the subjects who had negative outcome had an increase in HR <18 bpm. However, it has also been documented in the literature that HR increase during the first few minutes of tilt testing was not a good predictor of test outcome.[18] For validating the premise of prediction of tilt test outcome based on early heart rate data, a prospective study with a large number of subjects is necessitated.
SBP during syncopal outcome was found to be maintained till 30 min of tilt followed by a precipitous fall thereafter. SBP during negative outcome was found to be maintained with a variation of 2–5 mmHg. The narrowing of pulse pressure during hemodynamic instability is worth mentioning. PP fell by a larger magnitude in positive cases after 30 min onward. This trend was not found during negative outcome. The reason for more narrowing of PP during positive outcome perhaps is brought about by a larger hemodynamic instability reflected by a larger fall in SBP and DBP. This instability was reflected in mean arterial pressure also.
It has been suggested in the literature that in addition to neurocardiogenic syncope, various other abnormal patterns of heart rate and BP responses to tilt test may be recognized during diagnostic tilt testing of patients with unexplained syncope.[15] One such response, which is commonly reported in the literature, is POTS and was first described by Low et al. of Mayo Clinic.[19] The HR increase in patients with POTS in the present study varied from 34–51 bpm up to 45 min of tilt. This increase in HR is way higher than the increase in HR of negative and syncopal outcome. Impaired vascular innervation, high plasma norepinephrine concentrations, α-receptor sensitivity, deconditioning, hypovolemia,[20] β-receptor hypersensitivity,[21] and baroreceptor dysfunction[22] have been attributed to reasons behind increase in HR. Low blood volume has been reported in the literature as one of the major causes of POTS.[23]
CONCLUSION
This retrospective analysis revealed that HUT was carried out among 168 subjects who were referred to the Department of Space and Environmental Physiology for the evaluation of episodic loss of consciousness. They were evaluated in an automated tilt table by making them passively stand at an angle of 70° from the ground for 45 min. The analysis revealed that 21 (12.5%) cases showed positive outcome. Of these, seven cases had POTS and remaining had neurocardiogenic syncope with frank loss of consciousness. The cardiovascular responses to HUT showed distinct differences among cases showing positive and negative outcomes.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Syncope: Current diagnostic evaluation and management. Ann Intern Med. 1990;112:850-63.
- [CrossRef] [PubMed] [Google Scholar]
- The head-up tilt table test and cardiovascular neurogenic syncope. Am Heart J. 1993;125:476-82.
- [CrossRef] [Google Scholar]
- Tilt table testing for assessing syncope. J Am Coll Cardiol. 1996;28:263-75.
- [CrossRef] [Google Scholar]
- The postural tachycardia syndrome: A brief review of etiology, diagnosis and treatment. Hell J Cardiol. 2002;43:47-52.
- [CrossRef] [Google Scholar]
- Usefulness of head-up tilt test in evaluating patients with syncope of unknown origin and negative electrophysiologic study. Am J Cardiol. 1990;65:1322-7.
- [CrossRef] [Google Scholar]
- Orthostatic tolerance of normal Indians and those with suspected abnormal cardiovascular reflex status. Aviat Space Environ Med. 1986;57:168-73.
- [Google Scholar]
- 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: A report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2017;70:e39-110.
- [Google Scholar]
- 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39:1883-948.
- [CrossRef] [Google Scholar]
- The tilt table test is useful for the diagnosis of vasovagal syncope and should not be abolished. J Clin Hypertens. 2020;22:686-9.
- [CrossRef] [PubMed] [Google Scholar]
- The pathophysiology of common causes of syncope. Postgrad Med J. 2000;76:750-3.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative cardiovascular responses to 70 head up tilt in pilots and non-pilots. Ind J Aerosp Med. 1983;1:36-42.
- [Google Scholar]
- Cardiovascular changes on 2 hours exposure to-6 deg head down tilt. Ind J Aerosp Med. 1991;35:1-5.
- [Google Scholar]
- Cardiovascular responses to orthostatic challenge in the endurance-trained services athletes. Ind J Aerosp Med. 1994;38:57-67.
- [Google Scholar]
- Sympatho-vagal modulation of cardiovascular functions of aerobic and resistance trained individuals in simulated microgravity. Ind J Aerosp Med. 2014;58:1-7.
- [Google Scholar]
- The normal response to prolonged passive head up tilt testing. Heart. 2000;84:509-14.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction of head-up tilt test result by analysis of early heart rate variations. Circulation. 1997;96:581-4.
- [CrossRef] [PubMed] [Google Scholar]
- Predictor of a negative tilt-table test result based on early heart rate variation in patients with a history of syncope. Am Heart Hosp J. 2007;5:247-9.
- [CrossRef] [PubMed] [Google Scholar]
- Early heart rate increase does not predict the result of the head-up tilt test potentiated with nitroglycerin. Rev Esp Cardiol. 2005;58:499-503.
- [CrossRef] [Google Scholar]
- Why do patients have orthostatic symptoms in POTS? Clin Auton Res. 2001;11:223-4.
- [CrossRef] [PubMed] [Google Scholar]
- Postural orthostatic tachycardia syndrome. Texas Hear Inst J. 2020;47:57-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperdynamic beta-adrenergic: Circulatory state. Arch Intern Med. 1970;126:1068-9.
- [CrossRef] [PubMed] [Google Scholar]
- Baroreflex control of muscle sympathetic nerve activity in postural orthostatic tachycardia syndrome. Am J Physiol Heart Circ Physiol. 2005;289:H1226-33.
- [CrossRef] [PubMed] [Google Scholar]
- A review of postural orthostatic tachycardia syndrome. Europace. 2009;11:18-25.
- [CrossRef] [PubMed] [Google Scholar]






