Translate this page into:
Analysis of incapacitation during +Gz induced loss of consciousness

*Corresponding author: Dr MD Sharma, MBBS, MD (Aerospace Medicine), Station Medicare Centre, Air Force Station Srinagar, Indian Air Force, Srinagar - 190001, J & K, India. mdaeromed@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma MD, Biswal P, Taneja N, Agarwal A. Analysis of incapacitation during +Gz induced loss of consciousness. Indian J Aerosp Med 2021;65:91-96.
Abstract
Introduction:
Occurrence of G induced loss of consciousness (G-LOC) during centrifuge training is a known entity. The Indian Air Force is currently undertaking high G training of its fighter pilots in High Performance Human Centrifuge (HPHC) which has significantly higher operational capabilities. The study aimed to analyse the incapacitation periods and myoclonic jerks associated with G-LOC occurring during HPHC training.
Material and Methods:
Records of episodes of 161 G-LOC during closed loop Rapid Onset Rates (ROR) runs over a period of 7 years from 2011 to 2017 were analyzed. The video recordings of these G-LOC episodes were assessed in terms of the participant demographics, +Gz onset rates, incapacitation periods, and presence or absence of myoclonic jerks during the G-LOC episodes. Descriptive statistics was applied to analyze the incapacitation periods and the duration of the myoclonic flail movements. Single tailed t-test was used to analyze the difference between the incapacitation periods of the aircrew who suffered myoclonic flail movements and those who did not. One-way ANOVA was carried out to assess the differences in incapacitation periods, if any, between aircrew of different age groups. Significance was set at P < 0.05.
Results:
Of these 161 episodes of G-LOC, 43.5% were seen in trainee aircrew. The mean Absolute Incapacitation Period (AIP), Relative Incapacitation Period (RIP) and Total Incapacitation Period (TIP) was 6.9 ± 2.3 s, 12.2 ± 4.7 s, and 19.1 ± 5.5 respectively. Age and flying experience did not show any significant effect with any of the incapacitation periods (p>0.05). The TIP correlated better with the RIP than with the AIP (Pearson’s correlation values of 0.9 and 0.52 respectively). Myoclonic flail movements were witnessed in 25.5% of G-LOC episodes with an average duration of 5.3 s and more than 50% occurring at ≥8Gz. The mean duration of RIP was significantly higher (P=0.03) when G-LOC was associated with myoclonic flail movements, whereas, the duration of AIP did not show any significant difference.
Conclusion:
The shorter incapacitation periods observed in the study compared to that reported in most of the previous studies could be attributed to the faster Gz offset rates of the present HPHC. Episodes of G-LOC having myoclonic movements were found to have higher relative incapacitation periods. Even though these movements were associated with G-LOC occurring at higher Gz levels, the durations were independent of the Gz levels.
Keywords
G-LOC
HPHC
Incapacitation period
Myoclonic flail movements
INTRODUCTION
G induced loss of consciousness (G-LOC) is a well reported aeromedical entity among aircrew flying high-performance aircraft.[1] It has been defined as “a state of altered perception wherein (one’s) awareness of reality is absent as a result of sudden, critical reduction in cerebral blood circulation caused by increased G force.”[2] In-flight G-LOC in high-performance aircraft can have disastrous consequences.[1]
Occurrence of in-flight G-LOC can be effectively prevented by aeromedical indoctrination of fighter aircrew on ground based centrifuge training. The Indian Air Force has been imparting centrifuge training to its combat aircrew at the Institute of Aerospace Medicine (IAM) Indian Air Force (IAF) since 1991.[3] The primary objective of centrifuge training is to improve an aircrew’s skill to perform Anti-G Straining Maneuver (AGSM) during exposure to high G stress. The other objectives are to impart an understanding of acceleration physiology, to inculcate a better appreciation of factors with potential to reduce G-tolerance, indoctrinate on physical conditioning program, and to build their confidence in their own ability to tolerate high G-stress.[1,3] Even though centrifuge training is conducted in a safe and controlled environment under direct supervision, occurrence of G-LOC during such training is a known eventuality.[1,4]
The period of G-LOC has been divided into Absolute Incapacitation Period (AIP), which is the period of complete unconsciousness and the Relative Incapacitation Period (RIP), which is a variable period of confusion and disorientation following return of consciousness and ends by the aircrew being able to make purposeful movements to recognized stimuli. Together, these form the Total Incapacitation Period (TIP).[5] The TIP is the actual period for which the aircrew would remain practically incapacitated in the event of an in-flight G-LOC. In the centrifuge study conducted at the USAF School of Aerospace Medicine, the duration of AIP has been documented to be 15 s (range of 9–20.5 s).[4] Other studies have described an average AIP of 12 s (range of 2–38 s) and an average RIP of 15 s (range 2–97 s).[6] Forster, in his study conducted in the US Navy, reported an average AIP of 7 s and an RIP of 9 s.[7] In another study conducted in the US Navy, the AIP and TIP during ROR centrifuge runs were found to be 5.8 ± 2.5 s and 15.2 ± 6.7 s, respectively.[8] Wilson et al.[9] reported mean AIP and RIP of 13.9 s and 15.1 s, respectively. A previous study carried out at this centre with an older human centrifuge revealed AIP and RIP of 10.3 ± 4.2 s and 6.9 ± 3.7 s, respectively, with a TIP of 17.2 ± 5.8 s during ROR runs.[10]
G-LOC has also been classified as Type-I and Type-II. Type 1 G-LOC is characterized by a short duration and the absence of convulsive type movements. Longer periods of unconsciousness with associated convulsive movements (flail) and frequently, recognizable dream-like states characterize Type II G-LOC episodes.[11] Hence, not only the periods of incapacitation but also the myoclonic convulsive movements have significant operational relevance in cases of in-flight G-LOC. The IAF has conducted many studies on G-LOC, A-LOC, Gz tolerance, and incapacitation periods.[10,12,13] However, most of these studies are based on the older centrifuge with different Gz onset and offset rates. With centrifuge training currently being undertaken in the advanced High Performance Human Centrifuge (HPHC) with Gz onset and offset rates more in line with those experienced in actual aircraft, a similar study analyzing incapacitation periods and myoclonic jerks was the aim of this study.
MATERIAL AND METHODS
The study was conducted in the Department of Acceleration Physiology and Spatial Orientation at IAM, IAF which is home to the HPHC manufactured by M/s AMST Systemtechnik GmBH, Austria. The HPHC is capable of generating acceleration onset and offset rates of up to 10 G/s. The peak G attainable for human subjects is +9 Gz. It is also capable of simulating multi-axial acceleration with peak attainable values of ±6 Gy and ±10 Gx. The centrifuge has both closed loop (pilot-in-control) and open loop (pilot not in control) modes. Majority of centrifuge runs are carried out in the closed loop mode with pilot controlled Gz onset rates and the pilot being required to chase a target aircraft projected on the out-of-the-window display. The centrifuge runs are controlled by a team of three controllers, one of whom is a physician trained in Aerospace Medicine. The aircrew undergoing the centrifuge run is under constant video monitoring.
In the present study, records of 161 G-LOC episodes during closed loop ROR runs, spanning a period of 7 years from 2011 to 2017 were analyzed. The number of aircrew was 160 as one aircrew had suffered G-LOC twice. The video recordings of these G-LOC episodes were studied in terms of the participant demographics, +Gz onset rates, incapacitation periods and presence or absence of myoclonic jerks during the G-LOC episodes.
The video recording of each LOC episode was viewed independently by each investigator several times and the durations of incapacitation (AIP, RIP, and TIP) as well as was duration of myoclonic flail movements were measured. The maximum discrepancy allowed between the inter-observer measurements was 1.0 s. In the event of a discrepancy, the video recording was re-viewed together by the investigators and a consensus was arrived at the periods of incapacitation and the myoclonic jerk. The time of absolute incapacitation was defined as the time from rolling of the aircrew’s eyeballs or sudden slumping of the head or a combination of these to the aircrew trying to purposefully raise his head from a slumped position. The relative incapacitation period was defined as the period from the aircrew trying to raise his head from a slumped posture to the time when he gave a definite verbal response to repeated calls from the centrifuge controller.
Descriptive statistics was applied to analyze the incapacitation periods and the duration of the myoclonic flail movements. Single tailed t-test was used to analyze the difference between the incapacitation periods of the aircrew who suffered myoclonic flail movements and those who did not. Oneway ANOVA was carried out to assess the differences in incapacitation periods, if any, between aircrew of different age groups. Significance was set at P < 0.05.
RESULTS
The mean age of the aircrew who had suffered G-LOC in the HPHC was 25.6 ± 3.69 years. The mean flying experience was 474.5 h. The distribution of the age and flying experience of the aircrew is shown in Figures 1 and 2, respectively. Of the 161 episodes of G-LOC included in the study, 43.5% were seen in aircrew undergoing advanced jet training. Among the trained aircrew, 29.2% were observed in aircrew flying non-high performance aircraft whereas the remaining (27.3%) were seen in those flying high performance fighter aircraft.

- Age distribution of aircrew suffering G-LOC (n=161). G-LOC: G induced loss of consciousness.

- Distribution of flying experience (n=161).
Figure 3 shows the distribution of the +Gz levels at which various G-LOC episodes occurred. As is evident, maximum number of G-LOC episodes occurred at +Gz levels > 6.5G.
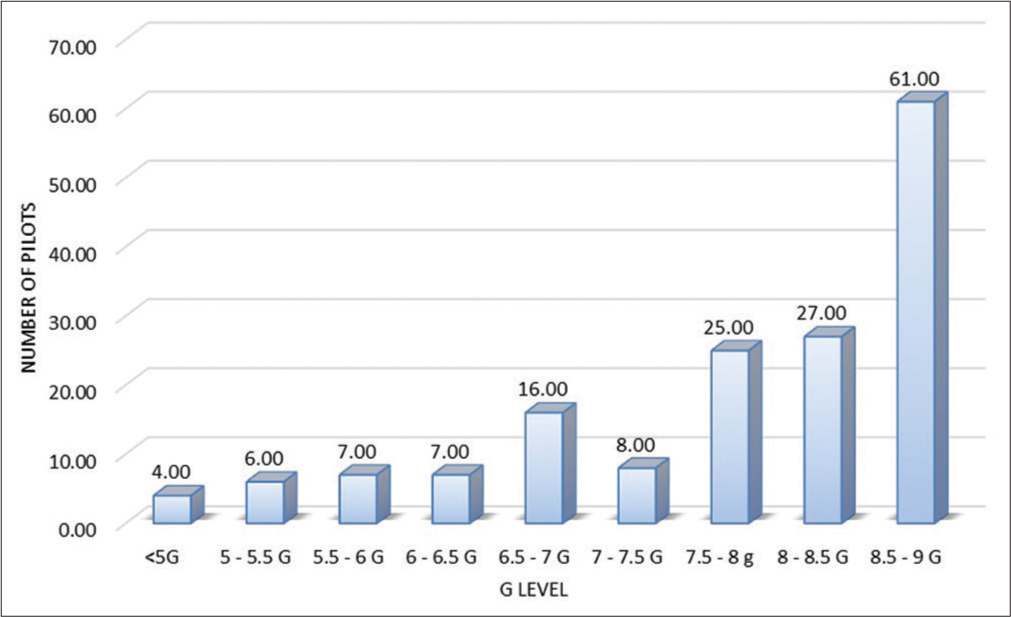
- G-LOC at various Gz levels (n=161). G-LOC: G induced loss of consciousness.
The average durations of incapacitation are listed in Table 1. The mean AIP was found to be 6.9 ± 2.3 s (range 3.4–16 s), whereas the mean RIP was 12.2 ± 4.7 s (range 3–37.8 s). The mean TIP was found to be 19.1 ± 5.5 s (range 11.9–44.9 s).
| Incapacitation period | Mean duration (s) | SD |
|---|---|---|
| AIP | 6.9 | 2.3 |
| RIP | 12.2 | 4.7 |
| TIP | 19.2 | 5.5 |
G-LOC: G induced loss of consciousness, AIP: Absolute incapacitation period, RIP: Relative incapacitation period, TIP: Total incapacitation period
Age and flying experience did not show any significant correlation with any of the incapacitation periods (P > 0.05). There was also no significant difference in the incapacitation periods between different age groups [Table 2]. The TIP correlated better with the RIP than with the AIP (Pearson’s correlation values of 0.9 and 0.52, respectively).
| Incapacitation period | F value | P value |
|---|---|---|
| AIP | 0.42 | 0.74 |
| RIP | 1.50 | 0.22 |
| TIP | 1.64 | 0.18 |
AIP: Absolute incapacitation period, RIP: Relative incapacitation period, TIP: Total incapacitation period
Of all the G-LOC episodes, myoclonic flail movements were witnessed in 41 (25.5%) (Type-II G-LOC). Of these, 22 episodes (53.6%) occurred at G levels of +8 Gz or more. The average duration of the myoclonic flail movements was 5.3 s (range 2.2–9.7 s). The average duration of myoclonic movements at G levels <8 Gz was 5.64 s, whereas that at levels ≥8 G were 5.06 s. The difference between the two was not statistically significant. All episodes of myoclonic movements occurred during recovery from G-LOC while the centrifuge was slowing down.
The mean AIP in aircrew suffering Type-I and Type-II G-LOC was 6.91s and 6.99s, respectively. The difference was not statistically significant. However, the mean RIP in aircrew who had Type-II G-LOC (13.38 s) was significantly more than those who had Type-I G-LOC (11.81 s) with P = 0.03 [Table 3].
| G-LOC type | Mean AIP (s) | P value | Mean RIP (s) | P value |
|---|---|---|---|---|
| Type-I | 6.91 | 0.42 | 11.81 | 0.03 |
| Type-II | 6.99 | 13.38 |
G-LOC: G induced loss of consciousness, AIP: Absolute incapacitation period, RIP: Relative incapacitation period
DISCUSSION
The average absolute and relative incapacitation periods in this study were found to be lesser than those described in the previous studies.[4,6,8,9] On the contrary, these periods were also more than what has been described by Forster.[7] Surprisingly, the incapacitation period, especially the RIP in the present study was more than that described by Modak et al.,[10] even though the centrifuge on which that particular study was conducted, had significantly slower onset and offset rates (1 Gz/s). Sensory stimuli, especially auditory cues, can hasten the recognition of G-LOC.[11] Even though Modak conducted his study on a centrifuge with 1 Gz/s offset rate, the subject was required to deactivate an audio alarm, which was activated on the onset of G-LOC. The present centrifuge does not have this feature. The subjects in Forster’s study were also required to turn off an audio alarm on regaining consciousness. The presence of these auditory stimuli can explain the shorter RIPs in these previous studies.
Majority of G-LOC episodes (65.2%) occurred in the age group of 20–25 years. It is also pertinent to note that, maximum episodes (40.9%) occurred in aircrew with 200–400 h of flying experience. This suggests that relatively inexperienced pilots might suffer a higher incidence of G-LOC as compared to the more experienced ones. However, the study also observed that age and flying experience did not correlate with the incapacitation periods. This possibly indicates no influence of these factors, once the G-LOC had occurred. Although reduction in the duration in incapacitation periods has been reported with previous G-LOC episodes,[7] information on the repeated occurrence of G-LOC on the same aircrew was insufficient in our study for any meaningful comparison.
Four aircrew suffered G-LOC at G levels <+5 G. This can be attributed to various factors such as the innate G tolerance, quality of the AGSM, empty stomach, and fatigue. Impact of these variables could not be studied within the scope of the present study. Moreover, Modak et al.[10] has described a 4.2 ± 0.47 Gz ROR tolerance of Indian aircrew without anti G suits. An aircrew at the lower end of this G tolerance spectrum, even with an inflated anti G suit, could theoretically suffer from G-LOC at levels <5 G.
The AIP did not correlate well with the TIP as compared to RIP since the former is physiologically determined and is not influenced much by extraneous factors.[11] The incapacitation periods are a function of the Gz onset and offset rates of the human centrifuge. Faster Gz offset rates leading to lower relative incapacitation periods has been proven.[14] It is also known that these periods are longer in GOR runs as compared to ROR runs.[7,10] The RIP, which is more variable than the AIP, is proportional to the rate of cerebral reperfusion. A faster Gz offset rate leads to a quicker cerebral reperfusion, thereby, leading to a shorter RIP. Since, all of the G-LOC episodes led to termination of the centrifuge runs, the rate of offset of Gz was 2 Gz/s in all these runs. Faster Gz offset rates are likely to reduce the incapacitation periods further. Some studies have analyzed the acceleration profiles of combat aircraft[15-19] and the Gz onset and offset rates of this centrifuge are similar to those described in our study. Hence, these incapacitation periods appear to be quite realistic and are of operational relevance.
The minimum achievable TIP is around 7 s.[11] Although probably not achievable in a centrifuge or in an actual aircraft, it is possible to bring down the incapacitation periods due to G-LOC from the present accepted values by faster Gz offset rates and incorporation of alarm systems in the centrifuges or even in aircraft. The audio alarm, connected to a pressure sensor on the control stick, can be activated by the reduction in grip pressure on the stick, the moment the aircrew starts to lose consciousness, with the resulting loss of muscle tone. Incorporation of such an audio alarm system is under consideration at our Institute.
In the present study, flail movements were observed in only 25.5% of G-LOC episodes. This is lesser than the 70% and 31% incidence reported by Whinnery in various studies.[20,21] The lower incidence in the present study can also be explained by the faster offset rates of the centrifuge. The duration of flail movements in the present study is in agreement with the previous studies.[22]
Type- II G-LOC episodes are known to have longer incapacitation periods.[11] The results of this study support this finding. However, there was no significant difference in the AIP between Type-I and Type-II G-LOCs. This can be explained by the fact that the Gz onset rates, although controlled by the pilot, were largely similar due to the nature of the target tracking task in the centrifuge. Similarly, the offset rates were uniform in all runs and the run terminations were undertaken by the physician controlling the runs. The efforts of the run controllers were directed towards preventing G-LOC and terminating the runs as soon as the first signs of the aircrew losing consciousness became evident. Hence, the AIP remained largely similar in both the groups. Moreover, the AIP is physiologically determined[10] and hence does not vary much in contrast to RIP, as this appears to be a function of rate of cerebral reperfusion. Werchan proposed the differential perfusion deficit hypothesis for cerebral blood flow during G-LOC.[23] This hypothesis suggests that the areas of the brain that is located near the top of the skull will be most susceptible to hypoperfusion under +Gz acceleration. These areas will also be the last to regain blood flow during recovery from G-LOC. Whinnery and Shaffstall[4] also proposed that myoclonic convulsions are related to a functional caudal reticular formation which becomes disinhibited by a non-functional cerebral cortex.
The relative paucity of EEG correlates of G-LOC recovery also points toward a subcortical origin of these myoclonic movements. The upper motor neurons in the motor cortex influence the spinal cord circuits by two routes: Direct projections to the spinal cord and indirect projections to brainstem centers that in turn project to the spinal cord. The reticular formation is one of the major destinations of these projections from the motor cortex. The indirect projections from the motor cortex through the brainstem centers influence motor behavior that involves the use of primarily proximal muscles. In contrast, the direct projections from the motor cortex to the spinal cord enable the speed and agility of movements than is possible using the indirect pathways alone.[24] The fact that the myoclonic flail movements during G-LOC recovery involve proximal muscle groups of the upper limbs, points toward mediation through these indirect pathways.
Since G-LOC is the result of cerebral hypoperfusion, the myoclonic convulsions occurring during recovery may be a variant manifestation of post hypoxic myoclonus (PHM). The myoclonus that occurs almost immediately after a hypoxic episode is called acute PHM. Some EEG features of acute PHM resemble those described by Wilson et al. during recovery from G-LOC.[25] However, it needs to be noted that PHM is a distinct clinical entity indicating a poor prognosis in a patient suffering a hypoxic cerebral insult. Hence, this finding needs to be treated with caution. Alternatively, these myoclonic jerks could be a manifestation of physiological myoclonus.[26] Further investigation into the electrophysiological activity during G-LOC recovery would shed more light on this aspect.
CONCLUSION
The present study revealed shorter incapacitation periods than most of the previous studies. This could be attributed to the faster Gz offset rates of the present HPHC. Moreover, since this study was carried out on operational pilots, with closed loop runs (pilot-in-control), the results appear to be more realistic. Centrifuge studies continue to provide vital insights into the entire spectrum of signs and symptoms associated with G-LOC. Further studies need to be carried out into the mechanism of the other phenomena associated with G-LOC, especially the myoclonic flail movements, to have a more complete understanding of this aeromedical stressor.
Acknowledgment
The authors would like to thank Dr MK Nayak, Dr R Chaurasia and Dr G Ghosh for their help in collecting the data for this study.
Declaration of patient consent
Participant’s consent not required as participants identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- G-induced loss of consciousness: Definition, history, current status. Aviat space Environ Med. 1988;59:2-5.
- [Google Scholar]
- Incapacitation time for +Gz-induced loss of consciousness. Aviat Space Environ Med. 1979;50:83-5.
- [Google Scholar]
- Observations on the neurophysiologic theory of acceleration (+Gz) induced loss of consciousness. Aviat Space Environ Med. 1989;60:589-93.
- [Google Scholar]
- Human response to acceleration In: Davis JR, Johnson R, Stepanek J, Fogarty JA, eds. Fundamentals of Aerospace Medicine (4th ed). Philadelphia, PA: Lippincott Williams & Wilkins; 2008. p. :90.
- [Google Scholar]
- A Database to Evaluate Acceleration (+Gz) Induced Loss of Consciousness (G-LOC) in the Human Centrifuge. In: Report No NAWCADWAR-93089-60 Naval Air Warfare Center. 1993. p. :24.
- [Google Scholar]
- G-LOC recovery with and without G-suit inflation. Aviat Space Environ Med. 1994;65:249-53.
- [Google Scholar]
- EEG correlates of G-induced loss of consciousness. Aviat Space Environ Med. 2005;76:19-27.
- [Google Scholar]
- Centrifuge training vis-à-vis G-LOC incidents: An upate. Indian J Aerosp Med. 2002;46:42-50.
- [Google Scholar]
- Converging research on +Gz induced loss of consciousness. Aviat Space Environ Med. 1988;59:9-11.
- [Google Scholar]
- Almost loss of consciousness (ALOC): A closer loof at its threat in fighter flying. Indian J Aerosp Med. 2004;48:17-21.
- [Google Scholar]
- Human tolerance to high sustained +Gz during simulated aerial combat manoeuvre. Indian J Aerosp Med. 1996;40:7-15.
- [Google Scholar]
- The effect of Gz offset rate on recovery from acceleration induced loss of consciousness. Aviat Space Environ Med. 1990;61:929-34.
- [CrossRef] [Google Scholar]
- Analysis of multi-axis acceleration profile in a supermanoeuverable aircraft. Indian J Aerosp Med. 2006;50:7-12.
- [Google Scholar]
- Acceleration stress during combat dynamics of a supermanoueverable aircraft: A comprehensive analysis of 72 Air Combat Manouevre (ACM) sorties. Indian J Aerosp Med. 2010;54:10-4.
- [Google Scholar]
- Analysis of combat acceleration profiles of MiG-21, MiG-29 and Mirage 2000 aircraft. Indian J Aerosp Med. 1996;40:1-6.
- [Google Scholar]
- Analysis of combat acceleration profile of two air superiority fighter aircraft. Indian J Aerosp Med. 1997;41:1-4.
- [Google Scholar]
- Recognising +Gz-indused loss of consciousness and subject recovery from unconsciousness on a human centrifuge. Aviat Space Environ Med. 1990;61:406-11.
- [Google Scholar]
- Characterization of the resulting incapacitation following unexpected +Gz-induced loss of consciousness. Aviat Space Environ Med. 1987;58:631-6.
- [Google Scholar]
- Some neurological signs and symptoms produced by centrifugal force in mran. J Physiol. 1945;104:10P-1P.
- [Google Scholar]
- Total and regional cerebral blood flow during recovery from G-LOC. Aviat Space Environ Med. 1996;67:751-8.
- [Google Scholar]
- Post-hypoxic myoclonus: Current concepts, neurophysiology, and treatment. Tremor Other Hyperkinet Mov (NY). 2016;6:409.
- [CrossRef] [Google Scholar]
- Myoclonic disorders: A practical approach for diagnosis and treatment. Ther Adv Neurol Disord. 2011;4:47-62.
- [CrossRef] [PubMed] [Google Scholar]






