Translate this page into:
Air sickness in trainee aircrew of Indian Air Force: Our experience with desensitisation
Abstract
Air Sickness (AS) is a common presentation during basic flying among most of the trainee pilots. Incidence of AS in the Indian Air Force (IAF) ranges between 30 to 40%. About 9% continue to have persistent AS and do not adapt spontaneously to aviation. They require intervention and are referred to No 2 Aero Medical Training Centre (AMTC) for desensitisation therapy (DT). A retrospective analysis of the available records was done to evaluate the incidence of AS and the success rate of DT at AMTC. Incidence of chronic AS requiring DT was 6.40% and 12.85% among male and female trainees, respectively. Success percentage after DT was 78.30% and 88.88% among males and females, respectively. DT helped 79.13% of airsick trainees to successfully complete basic flying training during the period of study. The remaining airsick trainee pilots were suspended from flying training. AS in trainee pilots is a major physiological problem leading to performance decrement. Various Air Forces have primarily adopted DT and graded exposure to flying as time-tested and a proven method of retrieving airsick trainee pilots. DT in IAF includes combination of counselling, physical and ‘yogic’ exercises, and desensitisation on Barany’s chair. This is followed by gradual exposure to straight and level flying. A trainee pilot is said to be successfully desensitised when he does not have any symptoms of AS and successfully completes basic flying training. Comparison of our results with those of other Air Forces shows that our success rates are comparable.
Keywords
Air sickness
desensitisation therapy
yogic exercises
Exposure of an unadapted person to real or apparent motion stimuli may lead to Motion Sickness (MS) [1]. The severity depends not only on the frequency, magnitude, direction and duration of motion, but also on the body posture and other characteristics of the individual and the environment [2]. The individual susceptibility to MS is critical in selection of personnel such as airmen, astronauts and sailors for work in MS provoking environment [3]. Air Sickness (AS) in trainee pilots is a major physiological problem. This leads to performance decrement and possible future suspension from flying training. This, in turn, leads to attrition and substantial economic loss to the organisation [4]. An incidence rate of 11% was reported among student pilots during WW II [5]. Dobie reported that 38.7% student pilots show some degree of AS and 14.6% showed signs of severe AS to cause significant performance decrement [6]. There is a transient increase in the frequency of AS when provocative manoeuvres like spin or aerobatics are undertaken [7].
An incidence of 30-40% AS amongst abinitio trainee pilots of Indian Air Force (IAF) has been reported in earlier studies. About 8-9% of airsick trainees have persistent AS and do not adapt fast enough. This also affects their training [8, 9]. These trainees require intervention and are referred to 2 Aero Medical Training Centre (AMTC) for desensitisation therapy (DT). This study was carried out to analyse the incidence and outcome of the desensitisation methods used at AMTC from 1994 to 2004.
Material and Methods
The subjects (n=115) for this study were airsick trainees undergoing basic flying training on a piston engine aircraft. Their average age was 21 years. All were medically fit for flying. DT is offered to all the trainees undergoing basic flying training at Air Force Academy, who manifest characteristic symptoms of AS viz. vomiting in all the first three familiarization sorties and or with recurrence of vomiting twice any time during the basic flying training after initial DT at AMTC.
An Aviation Medicine Specialist interviews the AS trainee reporting to AMTC about the episodes of AS. Necessary inputs are sought from the flying instructors about the sortie profiles and symptoms of his pupil. Details of past history of MS and any organic ailment enhancing susceptibility to MS are also elicited. A thorough physical examination is done for trainees to rule out any evident pathology. If no organic pathology is found, trainees are accepted for supervised DT.
A counselling and didactic session is conducted for each trainee before commencing DT. This includes an explanation of AS and DT; emphasis is also laid on expectations from trainees for better results. They are introduced to yogic exercises and physical exercise therapy (PET) schedule. Trained personnel demonstrate the yogic exercises and the PET routine. Trainees practice the exercise schedule under supervision till they can perform it correctly. The yogic exercises includes ‘Surya Namaskar’, ‘Pranayama’, ‘Sarvangasana’, and ‘Shavasana’ [9]. PET is discussed in detail subsequently.
Deshmukh et al’s schedule of cross-coupled Coriolis stimulation by PET is utilized for DT [11, 12]. This includes a set of four exercises. The first exercise is turning about vertical axis in standing posture while keeping one arm raised vertically up in a set of five rotations each in clockwise and anticlockwise directions. The second exercise involves the subject bending forward at waist level and rotating in clockwise and anticlockwise directions five times at near uniform rate at intervals of 30-45 seconds. The third exercise involves the subject walking forward at a moderate pace to complete 20 steps, then turning around to return to the original spot while rotating the head in clockwise and anticlockwise direction. The fourth exercise involves the subject lying supine on a flat surface and raising both legs together to assume a near vertical, head-down position. The body rests only on shoulders and head. The complete duration of PET is about 20 minutes. Once correct technique is perfected, trainees exercise once daily under supervision. They are expected to repeat them twice at their own convenience and are advised to conduct the learnt exercises preferably on empty stomach or at least 2-3 hours after food.
Barany’s rotation chair is used to simulate cross-coupled Coriolis stimuli [13]. In this ground-based simulation of AS, trainee sequentially tilts his head anteriorly, posteriorly and laterally while seated and rotating about the z-axis. Rotation speed is gradually increased from 5 to 15 rpm. Five rotations in clockwise and anticlockwise direction at 15 rpm form a set. They are administered 25 sets three times a day, thus totalling 75 sets each day, for five days. Trainees assess their own symptoms and subjective improvement. Whenever they do not tolerate the symptoms, the run is terminated to allow them rest for an hour before commencing the next session.
In-flight desensitisation after successful completion of ground-based DT is done with gradual reintroduction to flying. Flying instructors are briefed to avoid any aerobatics, hard turns or other provocative manoeuvres for the first two sorties. A verbal feedback from the trainee and the flying instructor is obtained about reappearance of symptoms. In case any trainee has recurrence of symptoms, he undergoes another 7 days of DT, similar to the initial schedule.
Criteria for successful DT are absence of vomiting or other symptoms of AS in flight and successful completion of basic flying training.
Results
From 1994 to 2004, 115 airsick trainees reported to AMTC for desensitisation therapy (Figure 1). The incidence of AS among male and female trainees was 6.4% (n=106) and 12.85% (n=9), respectively. The outcome of DT for AS is shown in Table 1. The overall success rate was 79.13% (n=91). Figure 2 shows the comparison of outcome of DT in the IAF since 1983. As is evident, combination of yogic exercise, PET and desensitisation with Barany’s chair in the past decade has had the best outcome, a success rate of 79.13%. Figure 3 compares the outcome of different Air Forces utilizing DT for AS. The comparison is made despite the premise that there are differences in treatment protocol and the aircraft used for basic flying training and in-flight desensitisation.
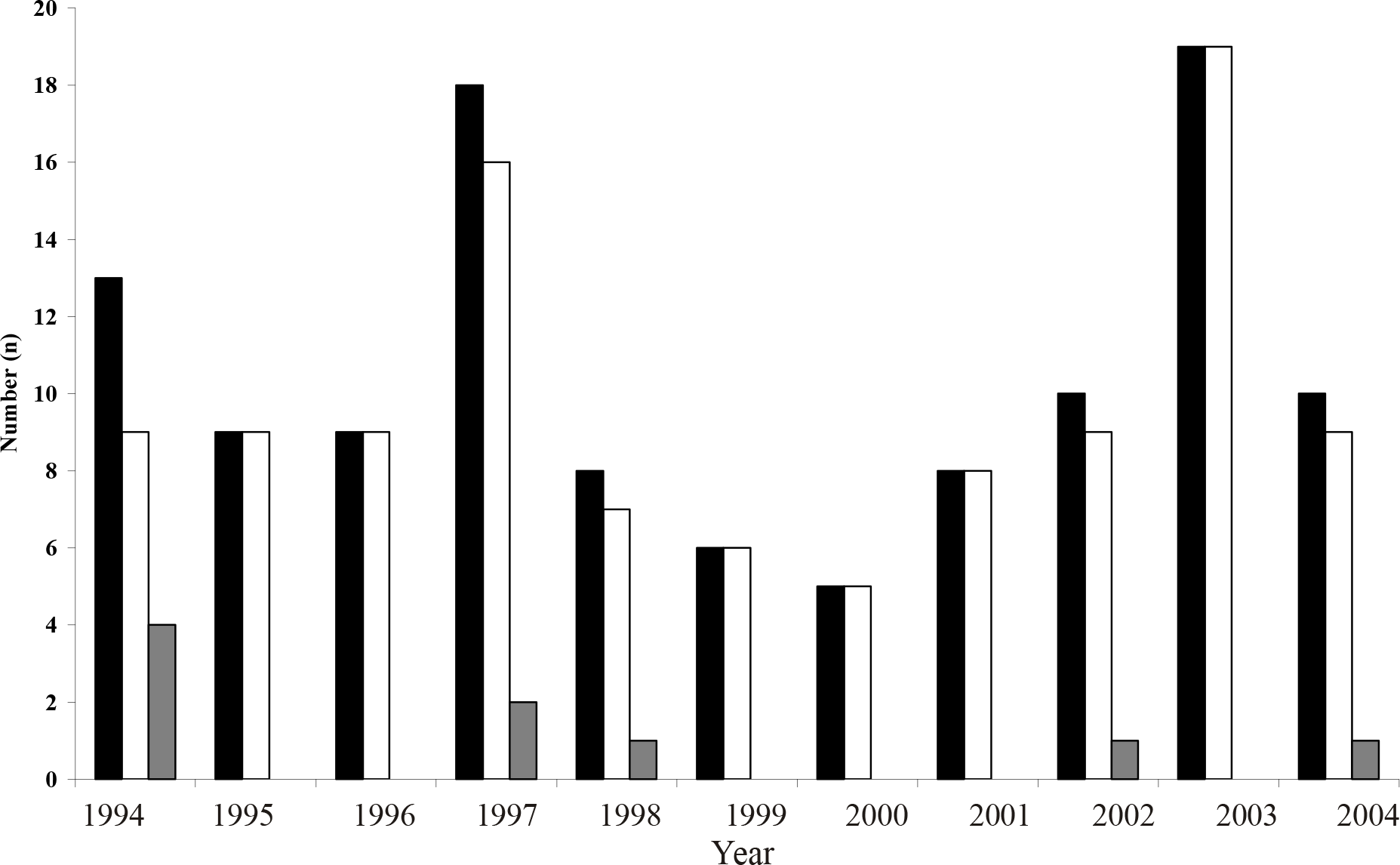
- Number of air sick trainee pilots for desensitisation therapy from 1994 till 2004
-
Legend : Black Rectangle: Total Number; Blank Rectangle: Males; Grey Rectangle: Females
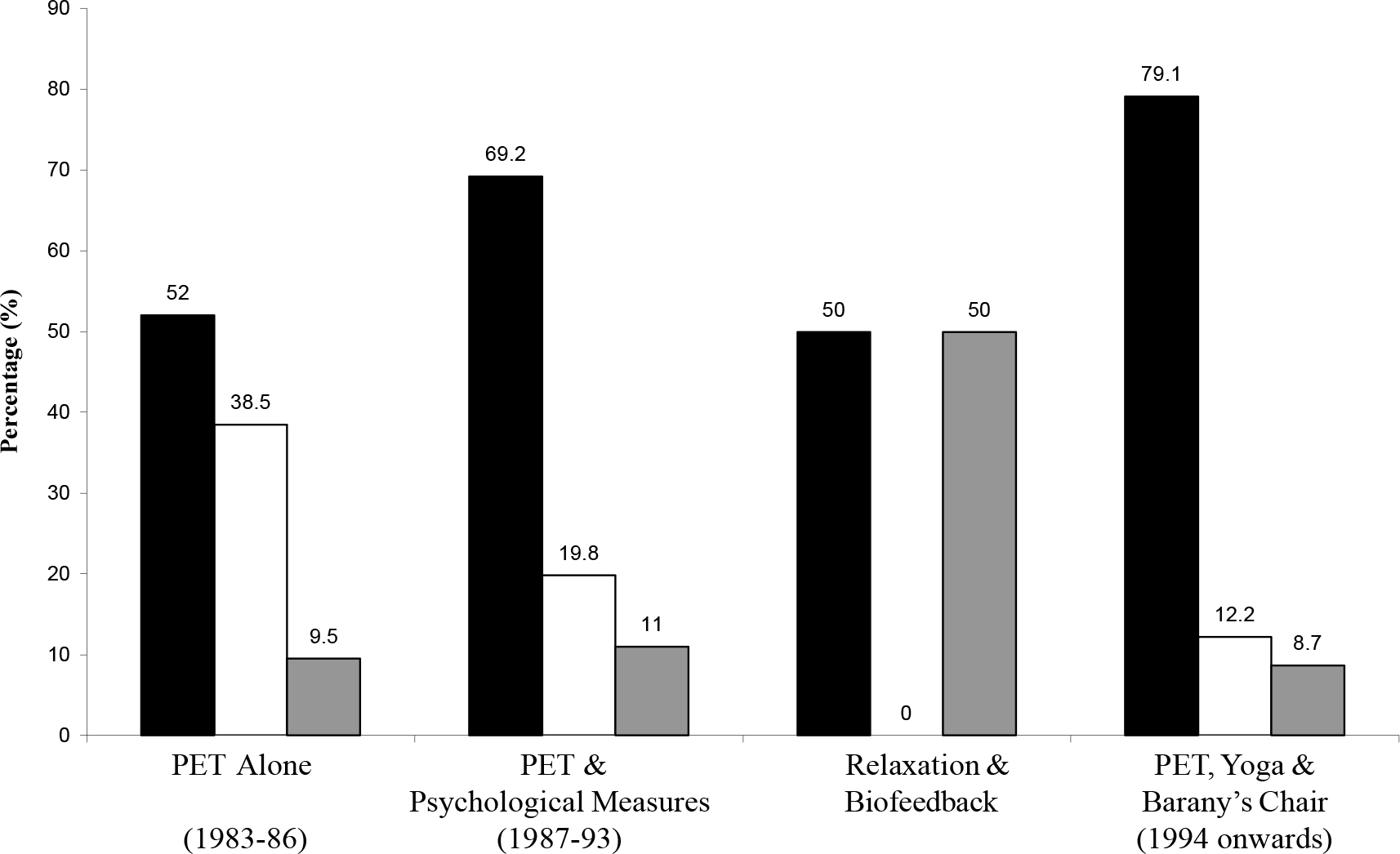
- Outcome of desensitisation therapy in IAF (1983-2003)
-
Legend : Black Rectangle: Successful; Blank Rectangle: Successful but did not learn flying; Grey Rectangle: Unsuccessful
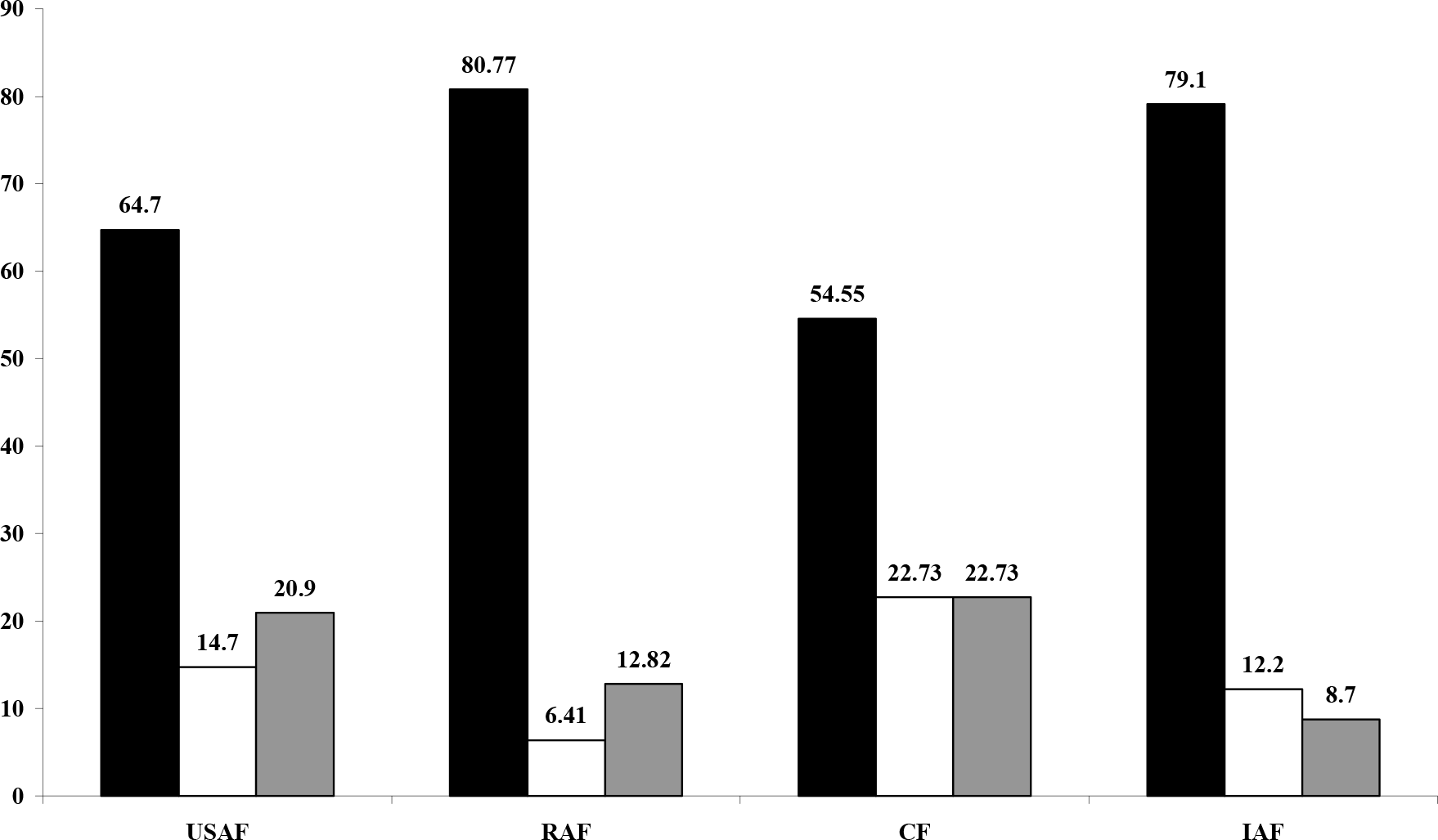
- Outcome of desensitisation therapy in various Air Forces (in percent)
-
Legend: Black Rectangle : Successful; Blank Rectangle : Successful but did not learn flying; Grey Rectangle : Unsuccessful; USAF : United States Air Force; RAF : Royal Air Force; CF : Canadian Forces; IAF : Indian Air Force
| Desensitisation | Total | Male | Female | |||
|---|---|---|---|---|---|---|
| Therapy | (n) | (%) | (n) | % | (n) | % |
| Successful | 91 | 79.1 | 83* | 79.41 | 8* | 88.8 |
| Unsuccessful | 24 | 20.9 | 23* | 21.6 | 1* | 11.2 |
| Total | 115 | 100 | 106 | 100 | 9 | 100 |
Discussion
Incidence of AS amongst trainee pilots is a major problem at any Basic Flying Training Establishment. Attempts at pre-selection weeding out by questionnaire and past history are not successful largely due to gross under reporting [16]. An airsick trainee may have poor learning due to performance decrement; and if not treated it may lead to possible suspension from flying training. Considering that any disqualification of a pre-solo trainee is estimated to cost around Rs. 900,000.00 [8], an overall incidence of 9.5% of AS in IAF remains an economic constraint on the exchequer. The higher incidence among female trainees as compared to males was statistically significant (p<0.001). This corroborates with findings of other workers [3, 17, 18, 19].
The successful outcome among 79.13% of AS trainees speaks highly about the DT at AMTC (Table 1). However the cause of persistent airsickness among 9.5% trainees in the past decade needs to be analysed. This may help lower the number of trainees removed from flying training due to persistent AS. Whether DT was inadequate for habituation or did motivation play a role to determine their willingness to cope up with their malady is a matter of debate. It is arguable that weeding out such trainees at the selection stage itself may help this percentage to reduce, although not completely [16].
The existing protocol has shown the best results so far (Figure 2). However, the criteria of success during evolution of DT have been different. For example, one of the studies [12] included only those cases as successful who not only became asymptomatic after DT but successfully went on to complete flying training to be commissioned as pilots. In comparison, the present study is limited to the outcome of DT till basic flying training stage only. Despite the above, the comparison still holds good as during the period of present study, there was no reported case of termination of flying training in subsequent flying stages due to AS till commissioning. Interestingly, rates of unsuccessful cases are comparable and not significantly different. Wadhawan and Kapur utilized yogic exercises and biofeedback system, respectively with varied results [8, 20]. Kapur had to deal with cases of resistant AS, who failed to respond to DT at AMTC [8]. Hence, the failure rate of 50% did not reflect ineffectiveness of biofeedback but a persistence of AS not amenable to non-pharmacological methods. This was considered incompatible with safe piloting.
Kumar and Sengupta utilised an ancient but now well known yogic concept for exercise [21]. Yogic exercises are known to allay anxiety, modulate autonomic system and allow self-initiation of a relaxation response to extraneous motion stimuli. This helps a trainee focus and concentrate on the task at hand. A few of those yogic exercises for vestibular habituation and reduction of susceptibility to MS by optimisation of arousal state are adapted for DT. This includes, firstly the ‘Surya Namaskar’ with recitation of the chant of ‘Om’ or ‘Gayatri Mantra’. Secondly, practice of ‘Pranayama’ to help develop an ability to control breathing. This helps decrease the state of anxiety. Both exercises help vibrate the body at a resonant frequency of 3-4 Hz, thus modulating the autonomic nervous system [9]. Thirdly ‘Sarvangasana’ simulates mild negative G effects with shifting of diaphragm and abdominal viscera, as experienced during descent from altitude. This is known to act as an AS provoking stimulus [11, 12]. Lastly, ‘Shavasana’ is a technique for physical and mental relaxation, which controls autonomic function, akin to Jacobson’s progressive muscle relaxation exercises [4, 15].
Besides the yogic exercise, PET and cross-coupled angular accelerations with head rotation on Barany’s chair, the protocol is designed to reproduce features of neural mismatch that are generated in the flight environment and allow the subject to be exposed to them in a controlled and incremental manner [1,4,14,15]. Tolerance acquired during exposure to cross-coupled stimulation by ground based desensitisation methods gets positively transferred resulting in decrease in susceptibility and increase in adaptability to provocative motion [22]. Evidently though, there is no single system of desensitisation for effective control of AS.
Various Air Forces have adopted a combination of methods for DT for AS (Table 2). These include two vital components: firstly, psychotherapy to alleviate the patient’s anxieties about flying and his future career; and secondly an adaptation schedule involving graded exposure to cross-coupled angular accelerations produced by passive head movements aboard a rotating platform [1, 4, 7, 11-15, 22- 24]. It must be added that in the absence of any latest reported protocols of ASDT, this study depended on relatively older literature available, assuming that the basics of DT have not changed much. However, readers may use their discretion while evaluating the outcome reported in various studies as per the reported protocol (Table 2).
| Ground based desensitisation | In flight desensitisation | |
|---|---|---|
| RAF (14) | Cross- coupled coriolis stimulation on rotation chair two sessions for 3 weeks after initial assessment at IAM Farnborough | Initial & advanced phases of flying schedule of 10-15 hrs in Hunter T-7 with medical pilot who is a QFI |
| USAF (4) | Employs biofeedback & relaxation therapy with cross-coupled coriolis stimulation, 2 session per day for 20 sessions | Five reorientation flights |
| CF (15) | Deep muscle relaxation training for two days, cross-coupled coriolis stimulation on rotation chair, two sessions per day till 15- 30 sessions. | Six flights in CT-114 tutor jet trainer by pilot flight surgeon |
| IAF | Physical exercise therapy, yogic exercises & cross-coupled coriolis stimulation on rotation chair for 7 days | Two sorties without any provocative manoeuvres in HPT – 32 by QFI |
Legend : RAF : Royal Air Force USAF : United States Air Force CF : Canadian Forces IAF : Indian Air Force
The overall success rate of 79.13% amongst IAF trainees is better than most of the reported rates and is comparable to that of Royal Air Force [4, 14, 15]. Interestingly, in IAF DT employed shorter duration, inexpensive, easy-to-perform physical exercises and had minimal exposure to in-flight desensitisation. The emphasis was on the individual’s motivation and willin to practice yogic exercise and PET, after perfecting the technique under supervision. There has been no study on motivation in airsick trainees and hence it is not possible to comment on this aspect. However, the authors observed that the trainees continued with their therapy despite repeated episodes of vomiting during DT; and they also showed a positive outlook to return to their flying training. It is recommended that this aspect be studied in future.
Conclusion
DT has proven its usefulness amongst trainee pilots over the past two decades. The encouraging results of this study suggest that DT at AMTC is safe, useful, easy to practice and cost-effective. The benefits accrued from applying yogic concepts require scientific validity. Also, factors like personality and motivation levels in successful rehabilitation of a significant numbers of trainees need to be evaluated.
References
- Motion sickness In: Ernsting J, Nicholson AN, Rainford DJ, eds. Aviation Medicine (3rd edition). Oxford: Butterworth-Heinemann; 1999. p. :455-61.
- [Google Scholar]
- Effect of seating, vision and direction of horizontal oscillation on motion sickness. Aviat Space Environ Med. 2000;71:996-1002.
- [Google Scholar]
- Gender differences in the motion sickness history and susceptibility to optokinetic rotation-induced motion sickness. Aviat. Space Environ Med. 1999;70:1077-80.
- [Google Scholar]
- Self-control of psychophysiologic response to motion stress using biofeedback to treat airsickness. Aviat Space Environ Med. 1985;56:1152-7.
- [Google Scholar]
- Desensitisation programme for cases of air sickness among flight cadets and aircrew of IAF. IAM Dept Project No. 121/ 4/81.
- [Google Scholar]
- Desensitisation of air sickness in trainee pilots by physical exercise therapy. Aviation Medicine. 1987;31:16-22.
- [Google Scholar]
- Airsickness desensitisation based on physical exercise therapy. Ind J Aerospace Med. 1995;39(2):9-19.
- [Google Scholar]
- Development and establishment of microprocessor controlled rotation platform for vestibular desensitisation in cases of air sickness amongst trainee pilots at Air Force Academy In: AR& DB Project: 750/1999.
- [Google Scholar]
- The desensitisation of chronically motion sick aircrew in Royal Air Force. Aviat Space Environ Med. 1985;56:1144-51.
- [Google Scholar]
- The Canadian Forces air sickness rehabilitation program 1981-1991. Aviat Space Environ Med. 1992;63:1098-1101.
- [Google Scholar]
- Air sickness in trainee aircrew of Indian Air Force. Ind J Aerospace Med. 1995;39(2):1-9.
- [Google Scholar]
- Motion sickness susceptibility and related characteristics in men and women. Aviat Space Environ Med. 1977;48:316-22.
- [Google Scholar]
- Effects of pre-exposures to a rotating optokinetic drum on adaptation to motion sickness. Aviat Space Environ Med. 1991;62:53-6.
- [Google Scholar]
- Effects of gender of subjects and experimenter on susceptibility of MS. Aviat Space Environ Med. 1999;70:962-5.
- [Google Scholar]
- . 1984;28(2):171-7.
- [Google Scholar]
- Yogic exercise as a prophylaxis to reduce air sickness and morbidity in ab-initio pilot trainees. Ind J Aerospace Med. 1996;40:56-61.
- [Google Scholar]
- In: Clinical Aviation Medicine (3rd edition). New York: Castle Connolly; 2000. p. :305-6.
- [Google Scholar]
- Neuropsychiatry in Aerospace Medicine In: DeHart RL, ed. Fundamentals of Aerospace Medicine (2nd edition). Philadelphia: Lea & Febiger; 1985. p. :555.
- [Google Scholar]






