Translate this page into:
Abnormal ECG patterns and significance in a group of mountaineers
Abstract
In the present study twenty four trained and otherwise fit mountaineers of the Indian Air Force, selected for Mount Everest expedition underwent routine evaluation for medical fitness prior to the expedition at Air Force Central Medical Establishment, New Delhi. Unexpectedly, a high percentage (29.16 %) of individuals were observed to have non specific ECG abnormalities. A small but important subgroup of mountaineers showed ECG abnormalities suggestive of cardiovascular disease and were subjected to detailed cardiovascular evaluation with exercise stress test, echocardiography and stress myocardial perfusion scan studies. The prevalence, clinical significance and determinants of abnormal ECG patterns in mountaineers have not been documented so far in the literature, although they are well documented in athletes, especially those involved in high endurance sports activities. The clinical significance of the abnormal ECG patterns in mountaineers is discussed.
Keywords
Mountaineers
12-lead ECG
athletic heart syndrome
The 12-lead ECG shows a broad range of abnormal patterns in people involved in high endurance sports, particularly increased QRS voltages, which are suggestive of left ventricular (LV) hypertrophy, and repolarization abnormalities [1-7]. These alterations have been attributed to the physiological cardiac adaptations that occur as a consequence of physical training [8]. Moreover, ECG patterns in such individuals may mimic structural heart diseases such as hypertrophic cardiomyopathy (HCM) or arrhythmogenic right ventricular cardiomyopathy (ARVC), which can be responsible for sudden death during physical exertion [9,10].
No study has yet documented ECG abnormalities among mountaineers. The aim of the present study was to elaborate the ECG abnormalities that were detected during medical examination of a group of twenty four mountaineers for Mount Everest expedition from the Indian Air Force (IAF).
Material and Methods
The study group consisted of 24 IAF personnel all of whom were healthy males, trained as mountaineers, in the age group 27 - 45 years. None of them had any significant past medical history.
The study was carried out at Air Force Central Medical Establishment, New Delhi.
A detailed history was taken and a thorough physical examination was conducted for all individuals. Haematological and biochemical parameters tested included blood glucose, total cholesterol, triglycerides, high density lipoprotein cholesterol, urea, uric acid and a complete haemogram.
Standard 12-lead ECGs were recorded with the subject in supine position at 25 mm/s. All ECG patterns were evaluated according to commonly adopted clinical criteria.
Two-dimensional, M-mode and Doppler echocardiographie studies were performed by a cardiologist at a tertiary care service hospital. Images were obtained in multiple cross-sectional planes using standard transducer positions. End-diastolic and end-systolic LV cavity dimensions and anterior ventricular septal and posterior free wall thicknesses were obtained from the M-mode echocardiogram. Parameters of LV filling were obtained with pulsed Doppler Echocardiography. Cardiac dimensions were judged to exceed normal limits when they were >95% of the predicted limits derived from populations of similar age, height and body surface area.
Exercise stress test and exercise myocardial perfusion imaging was done in select cases where there was a need to rule out coronary artery disease. The need to do these specialized investigations was left to the discretion of the cardiologist.
Results
Seventeen individuals (71%) did not reveal any abnormality on clinical examination and routine investigations. Seven individuals (29%) were noted to have abnormal resting ECGs (Fig 1). Three individuals had non-specific intraventricular conduction defects (IVCD) recorded in resting ECG (slurring of S wave in precordial leads with mild increase in QRS duration). Incomplete RBBB was seen in two individuals. Two individuals showed diffuse, symmetric, and marked T wave inversion associated with greatly increased precordial R or S wave voltages and/or deep Q waves, which is strongly suggestive of HCM (Fig 2).
Echocardiographie study showed that cardiac dimensions were normal in 22 of the 24 mountaineers. This included those with IVCD and incomplete RBBB. In two mountaineers in whom there was suspicion of HCM based on ECG, concentric left ventricular hypertrophy was noted. These individuals however did not have other findings to suggest HCM. No structural heart disease was noted in any individual.
Exercise stress test (TMT) was done in all individuals noted to have ECG abnormality. It was negative in all except one individual where significant ST depression was noted. This 40 year old individual with positive TMT underwent stress myocardial perfusion scan that was normal.
All the mountaineers were considered fit following detailed cardiovascular evaluation as described above.
Discussion
ECG abnormalities in mountaineers per se have not been described so far in literature. Mountaineering is comparable to other high endurance isometric athletic activities. Such ECG abnormalities in healthy Air Force personnel, who undergo periodic medical check up, were therefore not expected. There was a dilemma in certifying medical fitness with ECG abnormalities for an activity requiring the highest levels of medical fitness.
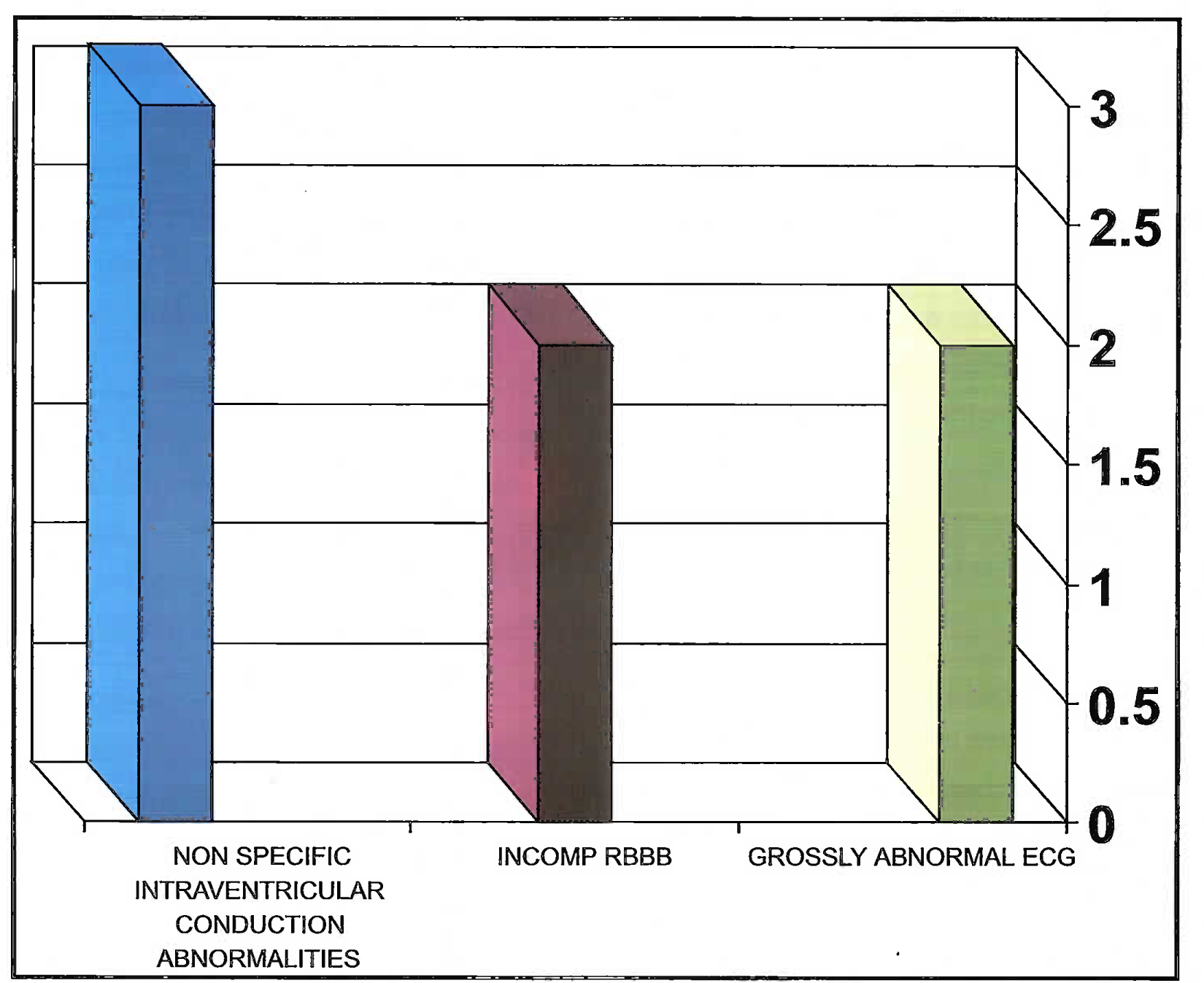
- Distribution off ECG abnormalities
- 12-lead ECG from a 36 year-old mile showed marked and diffuse T wave inversion (up to 7 mm to depth) in lateral precordial (V4 to V6) and irferior leads (II, III and aVF), increased R wave voltage >30 mm (V4-Vs).
Several reports in the past have described a variety of ECG alterations in trained athletes that have been attributed to cardiac adaptations to systematic athletic conditioning (increased vagal tone and diminished sympathetic drive) [1], ECG findings in high endurance athletes come under the diagnosis of “Athletic heart syndrome”[4, 7, 8]. The “Athletic heart syndrome” represents a constellation of clinical, electrocardiographic and echocardiographic alterations in trained athletes that have been attributed to cardiac adaptations to systematic athletic conditioning [7,8,12,13,14,15].
In sharp contrast to the low prevalence of abnormal ECG patterns reported in other surveys, [4,8,11,13,15] our data showed that 29% of the athletes had ECGs that raised clinical suspicion of cardiovascular disease. This apparent discrepancy may be the consequence of our definition of abnormality; we considered ECGs as abnormal even if they showed a prolonged PR interval, incomplete RBBB or early repolarization. In most of the other studies these have been regarded as normal and part of athletic heart syndrome.
The present study offers some insight into the clinical significance of ECG patterns because it directly compares ECG patterns with echocardiographic assessments of cardiac morphology. Structural cardiovascular diseases were not responsible for the abnormal ECG patterns. The low prevalence of cardiac disease in spite of abnormal ECG patterns was expected given that all the individuals have been examined and investigated several times before as part of periodic routine health evaluation in the Air Force.
In the absence of pathological conditions, the major determinant of altered ECG patterns was the morphological cardiac remodeling induced by physical training. Indeed, those mountaineers with the most marked ECG abnormalities showed increase in wall thickness and mass. Conversely, athletes with normal or mildly abnormal ECGs had normal cardiac dimensions. Similar correlation has been noted in other studies [13,15].
It is essential to perform echocardiography in athletes with abnormal ECGs for similar patterns have been noted in patients with HCM [9] or ARVC [14]. However, we found no familial, clinical, or echocardiographic evidence of these diseases to explain the ECG abnormalities.
The 12-lead ECG has been suggested as a relatively simple and inexpensive test to strengthen the limited diagnostic efficacy of the medical history and physical examination. Our findings in a small group of individuals participating in high endurance sports show a significant number having ECG abnormality. The strength of ECG testing as part of pre-participation cardiovascular screening in individuals participating in high endurance sports can be ascertained only after screening a large number of individuals. It is however recommended that all individuals participating in high endurance sports be screened so as to detect any underlying structural heart disease which might predispose them to sudden death.
References
- Recommendations for competitive sports participation in athletes with cardiovascular disease: A consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur. Heart J. 2005;26(14):1422-45.
- [Google Scholar]
- ECG variants and cardiac arrhythmias in athletes: clinical relevance and prognostic importance. Am Heart!. 1990;119:1378-91.
- [Google Scholar]
- Task Force 1: Preparticipation screening and diagnosis of cardiovascular disease in athletes. J Am Coll Cardiol. 2005;45(8):1322-26.
- [Google Scholar]
- Electrocardiogram of the athlete: alterations simulating those of organic heart disease. Arch Intern Med. 1973;132:763-70.
- [Google Scholar]
- Noninvasive evaluation of ventricular hypertrophy in professional athletes. Circulation. 1976;53:286-92.
- [Google Scholar]
- T wave abnormalities in top ranking athletes: effects of isoproterenol, atropine, and physical exercise. Am Heart J. 1980;100:213-22.
- [Google Scholar]
- Significance of abnormal electrocardiograms in highly trained athletes. Am J Cardiol. 1982;50:985-89.
- [Google Scholar]
- Identifying athletes at risk for sudden death. J Am Coll Cardiol. 2003;42(11):1964-66.
- [Google Scholar]
- Electrocardiographic diagnosis of exercise-induced left ventricular hypertrophy. Am Heart J. 1988;116:784-790.
- [Google Scholar]
- ECG variants and cardiac arrhythmias in athletes: clinical relevance and prognostic importance. Am Heart J. 1990;119:1378-91.
- [Google Scholar]
- Preparticipation screening for the detection of cardiovascular abnormalities that may cause sudden death in competitive athletes. Br J Sports Med. 2003;37(1):4-5.
- [Google Scholar]
- Arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2001;38(7):1773-81.
- [Google Scholar]
- Clinical Significance of Abnormal Electrocardiographic Patterns in Trained Athletes. Circulation. 2000;102:278-83.
- [Google Scholar]






