Translate this page into:
A rare case of “coronary slow-flow phenomena” in an aviator: An approach to aeromedical disposition – A case report

*Corresponding author:Dr N Manu, MBBS, Resident in Aerospace Medicine, Institute of Aerospace Medicine IAF, Bengaluru - 560017, Karnataka, India. dr.manu.n@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Manu N, Tripathy NK, Divya N. A rare case of “coronary slow-flow phenomena” in an aviator: An approach to aeromedical disposition – A case report. Indian J Aerosp Med 2020;64(1):46-9.
Abstract
Introduction:
Coronary slow-flow phenomenon (CSFP) is a frequent angiographic finding with obscure pathophysiology. Although recognized for decades, the incidence of such a clinical entity is rare in aviation environment and poses unique aeromedical challenges in disposition of the aircrew.
Case Details:
A 53-year-old asymptomatic pilot from a helicopter stream was detected to have ECG abnormality during a routine medical examination. His treadmill test was borderline positive for inducible myocardial ischemia, whereas angiography revealed proximal ectasia with a slow flow. He was diagnosed as a case of “Coronary Slow-Flow Phenomenon,” started on antiplatelets and was observed on ground for 36 weeks. A comprehensive cardiological evaluation following that revealed an asymptomatic status, controlled modifiable risk factors and no progression of ECG changes. Echocardiography, 24 h Holter, and stress MPI were essentially normal. Based on an evidence-based approach, the aircrew were reflighted back to flying in a multicrew aircraft.
Discussion:
This case study discusses our approach to aeromedical evaluation and disposition of a helicopter pilot with CSFP, which is unique, yet rarely encountered disability among aircrew.
Keywords
Coronary slow-flow phenomena
Coronary artery disease
Stress MPI
INTRODUCTION
Coronary slow-flow phenomenon (CSFP), sometimes referred to as coronary syndrome Y,[1] is an independent clinical entity identified in 1972,[2] in which angiography shows a delayed distal opacification of the coronary artery in the absence of any significant coronary artery disease (CAD). As similar phenomenon can also occur following the percutaneous coronary intervention, it is important to differentiate CSFP from the slow flow resulting from percutaneous coronary intervention. The presentation of CSFP with its clinical symptomatology differs from syndrome X. It is also different from coronary slow flow secondary to structural abnormalities such as coronary spasm, valvular heart disease, connective tissue disorders, and functional abnormalities like ventricular dysfunction.[3]
The CSFP needs to be differentiated from the CAD. This is because CAD accounts for 17 million deaths per year making it one of the leading causes of death globally and has been estimated to increase to more than 23 million by 2030.[4] In aviation environment, CAD is also the leading cause for grounding of aircrew both in civil and military flying. CAD in India is a virtual epidemic with 8–10% of the urban population being affected by the disease. The presentation is more diffuse, often manifesting as sudden unheralded death.[5] The rates of cardiac events and the risk of sudden death are higher in non-obstructive CAD and overall atheroma burden.[6] Thus, risk assessment of aircrew, who are young and are undertaking routine high hazard activities in which incapacitation or distraction may prove catastrophic becomes extremely important.[7] On the other hand, CSFP is potentially benign.
The CSFP is an angiographic observation characterized by angiographically normal or near-normal coronary arteries with delayed opacification of the distal coronary vasculature. Although the coronary microvascular disease is observed in myocardial biopsies in some patients exhibiting coronary slow flow,[8,9] the phenomenon has not been extensively studied. There has been limited investigation of the clinical features of patients with this angiographic phenomenon. The paucity of detailed research makes it unclear whether most cases of coronary slow flow represent an angiographic manifestation of a pathological condition affecting the coronary circulation, or whether it is a benign clinical condition without any implications. This paper discusses the approach to aeromedical evaluation and disposition of such a unique, yet rare case of CSFP in a helicopter aircrew.
CASE REPORT
A 53-year-old helicopter pilot was detected to have ECG abnormalities with T inversion in lead I, aVL, and V6 during routine medical examination [Figure 1]. The pilot was asymptomatic and all his ECGs carried out during the previous Annual Medical Examinations were normal. His 2D Echo revealed no regional wall motion abnormality, normal left ventricular function with an ejection fraction (EF) of 60%. Treadmill test (TMT) revealed T inversion in lateral leads, which was considered borderline positive for inducible ischemia. Coronary angiography (CAG) revealed proximal ectasia with slow flow in the left anterior descending (LAD) artery [Figure 2]. The aircrew were started on antiplatelets, statins, and nicorandil 5 mg BD. He was managed conservatively and placed in a non-flying category for 24 weeks.
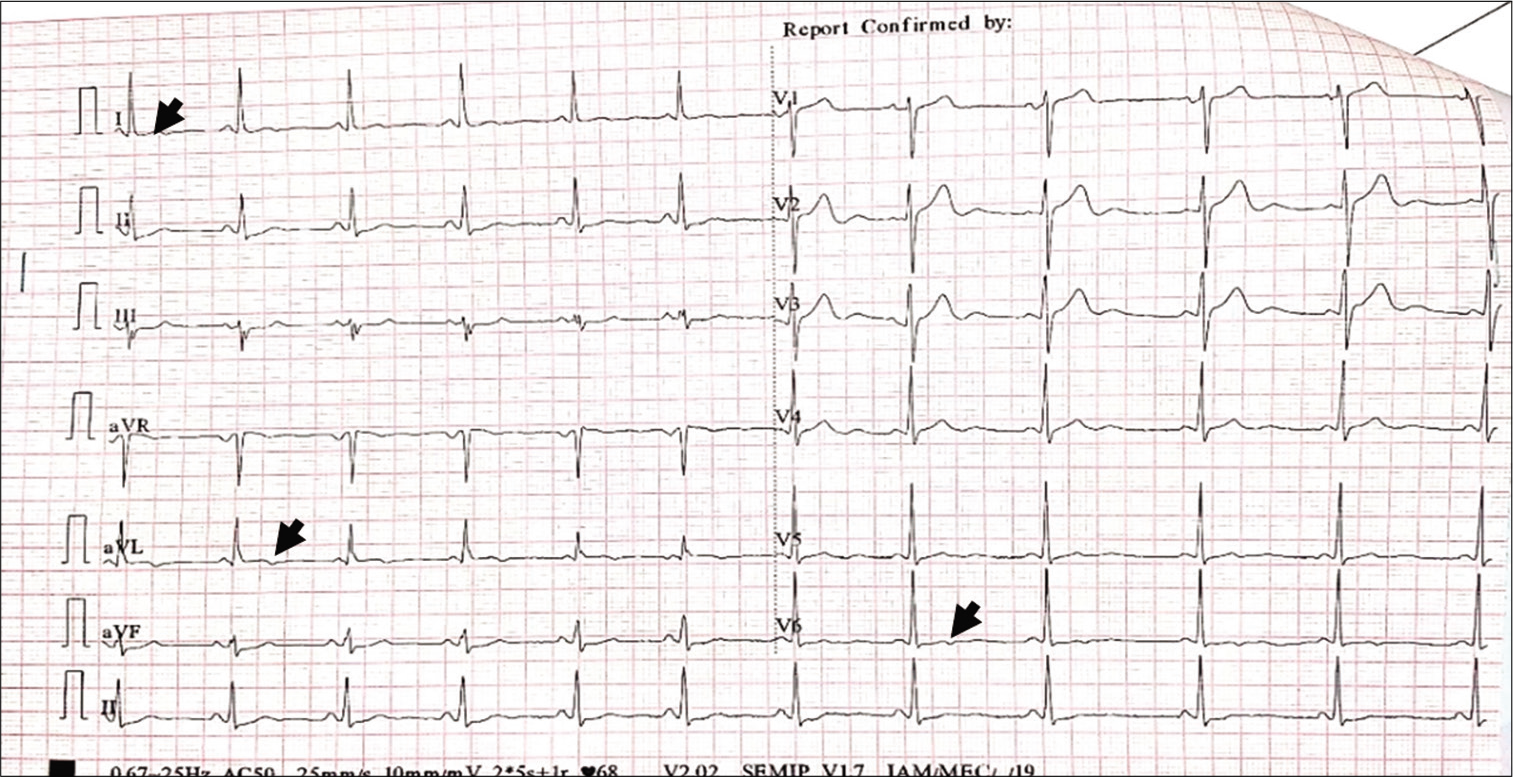
- ECG with T inversion in lead I, aVL, and V6.
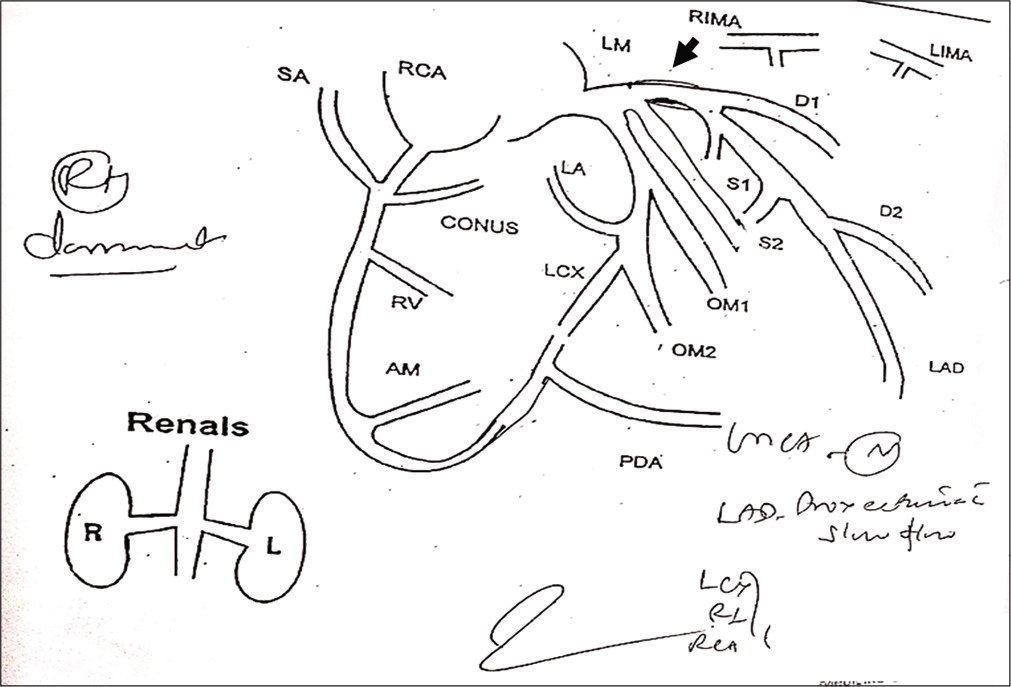
- Coronary angiography showing proximal ectasia.
Review after 24 weeks of observation on ground revealed that the aircrew continued to be asymptomatic with no progression in ECG findings. His 2D Echo remained within normal limits. He was recommended to continue in ground category for further observation for a period of 12 weeks.
The aircrew was reviewed at the Medical Evaluation Centre at the Institute of Aerospace Medicine (IAM) after 36 weeks of ground observation. During the review at IAM, the aircrew remained completely asymptomatic with fairly controlled modifiable risk factors. There was no progression of ECG changes. 2D Echo did not reveal any regional wall abnormality with an EF of 60%. Twenty-four-hour Holter study was within normal limits. Stress MPI was normal with no evidence of reversible or fixed perfusion defect. The cardiologist opined him fit for flying duties. Taking into consideration the objective clinical findings and possible aeromedical implications, the aircrew was reflighted back to helicopter flying. He was recommended follow-up with TMT once in 2 years and stress MPI once in every 5 years.
DISCUSSION
Our case was asymptomatic and was detected to have ECG abnormality during routine Annual Medical Examination. Asymptomatic ECG abnormality is not an uncommon finding in clinical practice. The incidence is approximately 32% in general population[10] and 3.59% among IAF personnel.[11]
All cases of asymptomatic ECG abnormality need to be comprehensively evaluated to rule out obstructive and conductive cardiac disorders. Accordingly, the aircrew was evaluated with TMT and 2D Echo, which were essentially normal. In addition to these investigations, the aircrew also underwent CAG under the provision of existing guidelines.[12] This becomes important in aircrew, wherein all possibilities of underlying disabilities need to be ruled out, in view of the risky operational environment. The possibility of acute incapacitation on flight safety is not acceptable.
The CAG study, in our case, revealed a unique finding. There was no obstruction of any coronaries, but slow flow was observed in the segment distal to an ectatic proximal LAD, a finding, consistent with CSFP. The condition is often referred as coronary syndrome Y,[1] due to the possible role of neuropeptide Y. In angiography, such a phenomenon is typically seen as a slow progression of angiographic contrast in the coronary arteries in the absence of stenosis in the epicardial vessels.[13] Diver et al. have observed the presence of CSFP in approximately one-hundredth of the patients undergoing CAG for acute coronary syndrome (usually unstable angina). An infarction (TIMI)-IIIA study states that 4% of patients presenting as unstable angina with normal or insignificant epicardial arterial blood vessel disease show impaired angiographic filling implicative of CSFP.[14]
Possible etiological factors of CSFP in our case may be arterial blood vessel ectasia (coronary artery ectasia), arterial blood vessel spasm, myocardial dysfunction, valvular cardiopathy, or certain tissue disorders involving coronary microvasculature.[15,16] Our case was detected to have an ectatic proximal LAD. Slow flow has been characteristically seen in ectatic coronary arteries with proportionate impairment of blood flow in these vessels with increasing coronary artery diameters.[17] Hagen–Poiseuille’s equation states that resistance to flow within a tube depends on the dimensions of the tube and the viscosity of the fluid in it.[18] The phenomenon of slow flow distal to the ectasia is in accordance with this rule. The reduced resistance in the ectatic area causes a delayed propagation of dye distal to the ectasia. On diagnosis, the aircrew was grounded for follow-up to observe the clinical behavior of the disability. He was started on statins and nicorandil. Lifestyle modification measures were advised to control modifiable risk factors. The case was observed for another 12 weeks on ground and then referred to Medical Evaluation Centre, IAM for review.
At IAM, the aircrew underwent a repeat ECG, 2D Echo, Holter, stress MPI, and a cardiologist opinion. The aircrew was reflighted back to flying after a comprehensive evaluation. Possible etiological factor, clinical course of the disease, investigation findings, compatibility with prescribed medications, likely aeromedical concerns, and need for follow-up formed the basis of aeromedical decision-making in the instant case. Even though patients with CSFP more often present with rest pains,[19,20] our case was completely asymptomatic with normal effort tolerance in NYHA-1 functional status since beginning and throughout the period of observation. The possible cause of CSFP in our case was ectasia of LAD, likely congenital in origin. Hence, the finding was considered incidental, who has never become symptomatic in his life. Although CSFP with remitting and relapsing anginal episodes resulting in impairment in quality of life has been documented in the literature, the clinical course of the disability is considered benign.[21] In our case, none of the cardiological investigations showed significant abnormalities. The Echo study revealed a normal left ventricular function with no motion abnormality. Holter study did not show any episodes of significant cardiac arrhythmias. Myocardial perfusion studies did not reveal any reversible or fixed perfusion defects or regional motion abnormalities. Further, all his modifiable risk factors were well controlled. In addition to all these factors, possibility of an in-flight incapacitation was considered. The same was assessed as “remote and unlikely,” and flight safety issues due to in-flight incapacitation in a multicrew cockpit were ruled out. Taking all these factors into consideration, the aircrew was reflighted back. However, since the literature reveals recurrence of chest pain in few cases,[17] the instant case was kept under follow-up with annual review with resting ECG, stress TMT once in 2 years, and stress MPI once in 5 years.
CONCLUSION
CSFP is a unique disability, in which slow progression of angiographic contrast is observed in the coronary arteries in the absence of any obstructive pathology. The phenomenon has been rarely reported among aircrew. The case study discussed in the paper brings out our evidence-based approach in reflighting a helicopter aircrew with CSFP. This can be used as a reference case in aeromedical disposition of aircrew for similar disabilities, wherein the literature is scanty.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
NK Tripathy is the editor of this journal. He does not have any competing interest.
References
- Coronary slow flow phenomenon or syndrome Y; a microvascular angina awaiting recognition. J Am Coll Cardiol. 2010;56:239-40.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary slow flow phenomenon. E J Eur Soc Cardiol Counc Cardiol Pract. 2013;11:25.
- [Google Scholar]
- Angina pectoris and slow flow velocity of dye in coronary arteries-a new angiographic finding. Am Heart J. 1972;84:66-71.
- [CrossRef] [Google Scholar]
- Executive summary: Heart disease and stroke statistics-2015 update: A report from the American heart association. Circulation. 2015;131:434-41.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing aeromedical risk: A three-dimensional risk matrix approach. Heart. 2019;105(Suppl 1):s9-16.
- [CrossRef] [PubMed] [Google Scholar]
- The risk continuum of atherosclerosis and its implications for defining CHD by coronary angiography. J Am Coll Cardiol. 2016;68:2467-78.
- [CrossRef] [PubMed] [Google Scholar]
- An introduction to aviation cardiology. Heart. 2019;105(Suppl 1):S3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Histologic evidence for small-vessel coronary artery disease in patients with angina pectoris and patent large coronary arteries. Circulation. 1986;74:964-72.
- [CrossRef] [PubMed] [Google Scholar]
- Slow coronary flow: Clinical and histopathological features in patients with otherwise normal epicardial coronary arteries. Cathet Cardiovasc Diagn. 1996;37:375-81.
- [CrossRef] [Google Scholar]
- Registry report of the prevalence of ECG abnormalities and their relation to patient characteristics in an asymptomatic population. QJM. 2018;111:875-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of asymptomatic ECG abnormalities in ground duty personnel in a forward air force base. Indian J Aerospace Med. 2012;56:2.
- [Google Scholar]
- Manual of Medical Examinations and Medical Boards. IAP 4303 (3rd ed). New Delhi: Indian Air Force; 2003.
- [Google Scholar]
- Diverse spectrum of presentation of coronary slow flow phenomenon: A concise review of the literature. Cardiol Res Pract. 2012;2012:383181.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and arteriographic characterization of patients with unstable angina without critical coronary arterial narrowing (from the TIMI-IIIA trial) Am J Cardiol. 1994;74:531-7.
- [CrossRef] [Google Scholar]
- The coronary slow flow phenomenon-a new coronary microvascular disorder. Cardiology. 2002;97:197-202.
- [CrossRef] [PubMed] [Google Scholar]
- Increased TIMI frame counts in cocaine users: A case for increased microvascular resistance in the absence of epicardial coronary disease or spasm. Clin Cardiol. 2003;26:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary hemodynamic and metabolic studies of the coronary slow flow phenomenon. Am Heart J. 2003;146:84-90.
- [CrossRef] [Google Scholar]
- Decrease in coronary blood flow reserve during hyperlipidemia is secondary to an increase in blood viscosity. Circulation. 2001;104:2704-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dipyridamole myocardial perfusion single photon emission computed tomography in patients with slow coronary flow. Coron Artery Dis. 2002;13:223-9.
- [CrossRef] [PubMed] [Google Scholar]
- Slow coronary run-off in patients with angina pectoris: Clinical significance and thallium-201 scintigraphic study. Braz J Med Biol Res. 1996;29:605-13.
- [Google Scholar]
- Long-term clinical course of patients with angina and angiographically normal coronary arteries. Clin Cardiol. 1991;14:307-13.
- [CrossRef] [PubMed] [Google Scholar]






