Translate this page into:
Myocardial Bridge: Forgotten Cause of Acute Coronary Syndrome A Case Report
Introduction
Myocardial Bridge is often termed as 'A forgotten cause of Acute Coronary Syndrome (ACS)’. It is a congenital coronary abnormality. It's defined as a segment of a major epicardial coronary artery –'the tunneled artery' that goes intramurally through the myocardium beneath the muscle bridge instead of resting on top of it [1,2]. It is generally found in mid left anterior descending coronary (LAD) artery [3,4]. The main angiographic finding is the systolic compression of the involved epicardial coronary artery. Quantitative coronary angiography [5], Intracoronary Doppler study and Intravascular ultrasonography [6,7,8,9] have documented a characteristic flow disturbance during systole that may have chance to exert significant inducible ischemia during exertion. The degree of obstruction depends on factors such as - location, thickness, length of the bridge, degree of cardiac contractility. In an autopsy series, the estimated frequency is as high as 80% [10,11]. Though it is considered as a benign condition, complications such as Ischemia, ACS, Coronary spasm, ventricular septum rupture, fatal arrhythmias, exercise induced AV block, transient ventricular dysfunction, early death after cardiac transplant and sudden cardiac death have been reported.
Case Report
A 40 year old helicopter pilot with 3670 hrs of flying experience was incidentally found to be positive for inducible ischemia on Treadmill Test (TMT) during his annual medical evaluation. The aviator was a known smoker for past 20 years with 06-08 cigarettes/day and history of occasional alcohol consumption. He used to lead a physically active lifestyle with regular running sessions and exercise. ECG, Radiological evaluations and blood investigations were essentially normal. He underwent Coronary Angiography that eventually revealed the specific clinical entity–'Mid myocardial bridge in LAD and mild plaque in Mid Right Coronary Artery (RCA)'. Subsequently, he was grounded and managed with optimum dosage of medications - Nonsteroidal anti-inflammatory drug (Aspirin), lipid lowering drug (Atorvastatin) and Calcium channel blocker (Diltiazem SR) with an advice for behavioral and lifestyle modifications. During his subsequent medical evaluation, he underwent 2D Echocardiography and 99 m Tc Tetrofosmin early gated single photon emission computed tomography-Myocardial perfusion imaging (SPECT MPI). The tests revealed normal cardiac status both structurally and functionally. The aircrew was upgraded to restricted flying category with waiver. Following uneventful 06 months period, he was awarded a restricted flying category for an additional 06 months. During the evaluation following the detection of his disability, he was recommended for flying in permanent medical category after 2D ECHO (Normal), Stress MPI (Normal) and TMT (+ve), with restriction for instructional duties.
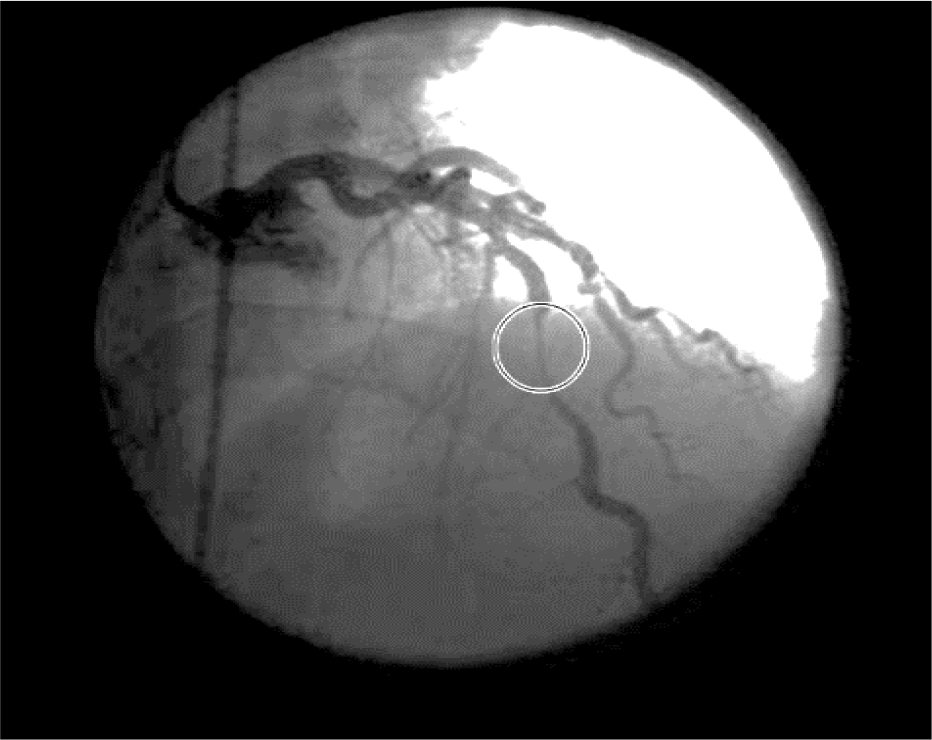
- CAG showing mid myocardial bridge in LAD
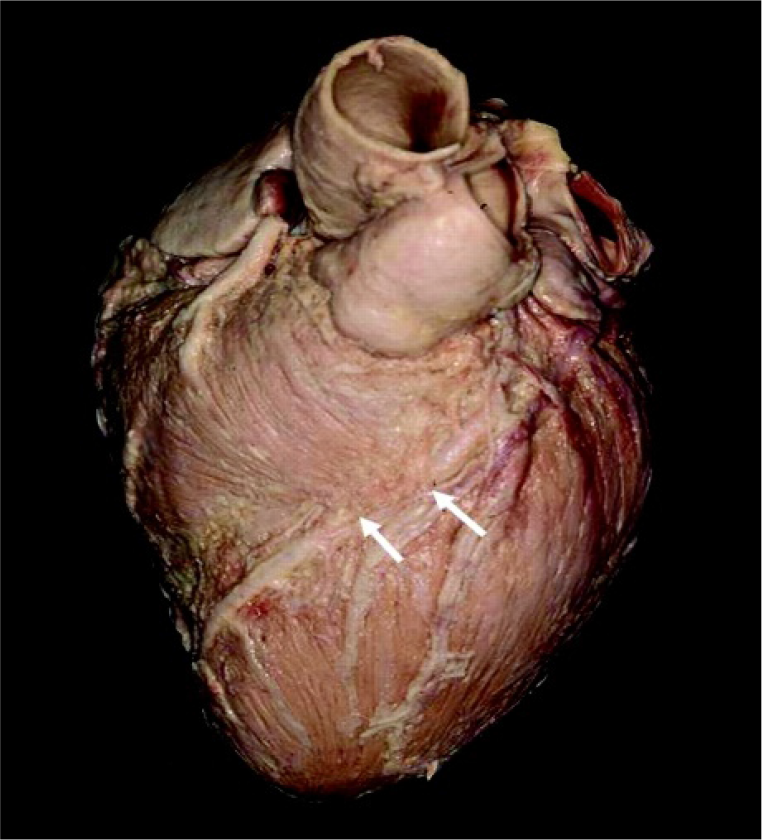
- Representational view-myocardial bridge in LAD
Discussion and Aeromedical Disposal Dilemma
With the advent of sophisticated investigative modalities 'Myocardial bridge' has come into light more frequently than was earlier known. When assessed by coronary angiography, the incidence varied from 1.5-16% where as it reached to much higher percentage (80%) when estimated by autopsy [10,11]. The entity has been generally known to be confined to the mid left anterior descending artery [12], with occasional presentations documented in right coronary artery. Earlier, Myocardial Bridge was often considered as a normal variant of coronary arteries. However, reports have suggested that it may be potentially hazardous with clinical relevance [12,13]. It has also been known to have higher propensity to develop atherosclerosis in coronary arteries. The typical angiographic findings demonstrate systolic narrowing of an epicardial artery that's fully resolved during diastolic phase. During the systolic phase of the cardiac cycle, because of the extrinsic compression of the tunneled artery, anterograde flow is significantly hampered and retrograde flow at the proximal segment of the myocardial bridge is observed. It may acquire significant relevance clinically, in particular conditions viz, extreme stressful activity and tachycardia. In tachycardia, diastolic phase is shortened and maximal coronary circulation happens during diastole. Hence, as heart rate increases, there is increased importance of systolic coronary flow (Normally 15% coronary circulation happens during systolic phase). Keeping these three facts into consideration, due to myocardial bridging, the tunneled coronary artery is likely to be more compressed during systolic phase, eventually leading to increased chance of sudden ischemia of that specific region of coronary circulation.
In this case of helicopter pilot, his TMT was positive using Bruce protocol. His coronary angiography showed 'Mid Myocardial Bridge' in LAD and mild plaque in mid RCA.
As per existing aeromedical disposal guidelines, the aircrew was be considered at par with a case of significant coronary artery disease (SCAD - owing to involvement of LAD); moreover, he was to be grounded till definitive management in form of surgery/ Percutaneous intervention (PCI) was performed. Having said this, in this aviator 2D ECHO showed adequate left ventricular ejection fraction (LVEF) without evidence of residual wall motion abnormality (RWMA); Stress MPI confirmed the findings by depiction of no structural anomaly. During his 2nd medical review after detection of the disability, the following facts were taken into consideration for waiver by the concerned authority to upgrade him in restricted flying category-
While TMT was positive for inducible ischaemia, the pilot remained asymptomatic carrying out his normal daily activities without any symptoms suggestive of compromised cardiac function.
His cardiac status was NYHA-I
The Coronary angiography showed 20-30% stenosis of LAD, the plaque in mid RCA was deemed unlikely to increase the total outcome.
2D Echo showed adequate LVEF without RWMA and a normal study.
Normal stress MPI (During cardiac evaluation with 99m TC Tetrofosmin Early gated SPECT Myocardial Perfusion Imaging, using stress-rest same day protocol, the pilot exercised upto a workload of 13.5 METS (Metabolic equivalents)and remained asymptomatic with target heart rate achieved; Stress and rest images were essentially normal with normal Myocardial perfusion, No RWMA, LV cavity normal; Resting MPI - Normal in all LV myocardial walls; RWM - Good systolic thickening seen in all resting images, LV cavity - Normal, Extent of LV wall defect - 0%, LVEF 66%)
Cardiologist assessed and opined him as a case of minimal CAD and recommended up-gradation to flying category.
The aircrew abstained from smoking and alcohol after initial diagnosis.
He adopted strict life style modification and dietary regime (Evident by weight loss).
While there is documentation in literature of propensity in such cases to develop myocardial ischemia due to sudden tachycardia during piloting an aircraft in various highly demanding and emergency situations, an already pathological heart may be seriously compromised by the possibility of myocardial ischemia and further enhance possibility of inflight incapacitation. The extant literature suggests surgical intervention, though the same was not deemed necessary for the aircrew in view of his stable and asymptomatic status [14]. Surgical approach is extremely delicate in these cases due to possibility of potentially fatal complications, including right and left ventricular perforation. Keeping the fact in mind that the individual was maintaining physically active life style that included regular physical exercise and total abstinence from smoking as well as alcohol, medical management and continued life style modification were considered a fair option without any apparent consideration of surgical intervention. Moreover, the aircrew was a dual cockpit rotary wing aircraft pilot where risk of sudden inflight incapacitation was anticipated to be minimal with proper precaution and medical management. Periodic medical checkups at his base were considered adequate to anticipate a cardiac event in case of stenotic lesions do increase in size/ number. The rationale behind restricting him from instructional duty was to take a preventive stance where he would be operating the aircraft with a trainee pilot.
As far as aeromedical decision making is concerned, standard techniques of exercise stress testing and follow-up (if indicated) with myocardial perfusion imaging and coronary angiography should continue to guide aeromedical certification decision processes [15]. Moreover, literature says myocardial bridge is the common cause of abnormal ECG in pilots and usually manifested as a superficial type which does not affect cardiovascular function and flying. Pilots with clinical symptoms should be assessed individually according to their treatment outcome and the types of airplane they fly. Since superficial myocardial bridge doesn't affect cardiovascular function, pilots can be declared qualified to fly a double-seat airplane while whether those flying a single-seat airplane should be assessed individually [16].
After up-gradation to flying category, the aircrew continues to be asymptomatic without any medication and flying comfortably for almost 02 years.
Conclusion
Extant literature indicates Myocardial Bridges to be a benign condition, but several recent studies have demonstrated that their clinical sequel may be catastrophic and may cause sudden cardiac death [17]. Aeromedical disposal of such case needs comprehensive physical, radiological and biochemical evaluation along with rational consideration of flight safety. Although he was TMT +ve, his Stress MPI result was essentially normal with normal myocardial perfusion, there was no RWMA, LV cavity was normal with adequate LVEF. MPI was demonstrated to have overall accuracy 83%, sensitivity 85% and specificity 72% [18] and is comparable (or better than) other non-invasive tests for ischemic heart diseases. Risk factors were satisfactory mitigated with normal stress MPI findings as well as structural and functional cardiac status. In this case, the aircrew was recommended to be observed in flying category with waiver after observation of 18 months with recommendation for periodic follow up. Appropriate timely usage of advanced radiological technique for suspected cases along with rational consideration regarding flight safety are of immense importance for disposal of such cases.
References
- Coronary anomalies: incidence, pathophysiology, and clinical relevance. Circulation. 2002;105:2449-54.
- [Google Scholar]
- Symptomatic myocardial bridging of coronary artery. Am J Cardiology. 1978;41:1305-10.
- [Google Scholar]
- Functional, angiographic and intracoronary Doppler flow characteristics in symptomatic patients with myocardial bridging: Effect of short-term intravenous beta-blocker medication. J Am Coll Cardiol. 1996;27:1637-45.
- [Google Scholar]
- Comparison of intravascular ultrasound and angiography in the assessment of myocardial bridging. Circulation. 1994;89:1725-32.
- [Google Scholar]
- Disturbed intracoronary hemodynamics in myocardial bridging: Early normalization by intracoronary stent placement. Circulation. 1997;96:2905-13.
- [Google Scholar]
- New approach to the diagnosis of myocardial bridging by intracoronary ultrasound and Doppler. Eur Heart J. 1999;20:1687-88.
- [Google Scholar]
- A case of myocardial bridging: Evaluation using intracoronary ultrasound, Doppler flow measurement and quantitative coronary angiography. Heart. 1996;76:374-76.
- [Google Scholar]
- Coronary anomalies: Incidence, pathophysiology, and clinicalrelevance. Circulation. 2002;105:2449-54.
- [Google Scholar]
- Coronary revascul-arization in patients with stable or asymptomatic CAD: Areview of courage trial. JCOM. 2008;15(7):349-53.
- [Google Scholar]
- A bridgetoofar? - Aeromedical certification decisions in aircrew with myocardial bridging. https://www.iaasm.org/documents/Abstracts_Vienna.pdf Accessed on 23 Sep 16
- [Google Scholar]
- Medical assessment of coronary artery myocardial bridge in 15 pilots. Journal of Chinese PLA Postgraduate Medical School. 2012;12
- [Google Scholar]
- Myocardial bridging in a young patient with sudden death. Clin Cardiol. 1997;20:581-3.
- [Google Scholar]
- Dobutamine stress myocardial perfusion imaging in coronaryartery disease. Journal of Nuclear Med. 2002;43(12):1634-46.
- [Google Scholar]





