Translate this page into:
HBOT in Frostbite: Less Explored Modality with Excellent Outcome
Abstract
Background:
Extreme cold weather along with certain risk factors, is known to cause ‘Frostbite’ that may lead to potentially serious tissue damage and necrosis.
Case Details:
A 38 year old non-smoker mountaineer with no known comorbidities and with history of expedition to Antarctica presented with sensory loss over great toe, second, third toe of the left foot and great toe, second toe of the right foot with progressive pain after a Himalayan Expedition at 6,200m altitude. Subsequently, he noticed dark discoloration on the plantar surface of left great toe. He was recommended tablet Pentoxyphyline. Symptoms worsened with numbness, pain and deep seated dark discoloration. After ruling out other possibilities with relevant investigations, he was managed conservatively with Pentoxyphyline, NSAID, Clopidogrel and multivitamins. Due to inadequate treatment response, he was recommended to undergo HBOT. On 12th day after summit, 1st session of HBOT was administered. He underwent 11 sessions of HBOT and was closely monitored and assessed with Galer Jensen Neuropathic Pain Scale (NPS). From the sixth session onwards, there was a significant clinical improvement as documented in the serial NPS.
Discussion:
Well established, definitive treatment modality for frostbite is still undefined. Neither Undersea and Hyperbaric Medical society (UHMS) nor European Society of Hyperbaric Medicine guidelines recommend HBOT as a treatment modality for frostbite. However, case studies have recommended that HBOT can be used effectively to treat frostbite. This case study supports available literature on possible benefit of HBOT in frostbite. Appropriate and timely administration of HBOT is immensely important to salvage reversibly injured tissues.
Keywords
Frostbite
HBOT
Galer Jensen Neuropathic Pain Scale
UHMS guideline
Introduction
From the arena of high altitude mountain warfare to various high altitude civilian activities, Freezing Cold Injuries (FCI) have taken a toll not only with significant morbidities but mortalities also. Frostbite, the most common type of freezing injury, is defined as ‘the freezing and crystalizing of fluids in interstitial and cellular spaces as a consequence of prolonged exposure to freezing temperature’ [1]. It happens due to acute freezing of the skin and tissues and usually develops following exposures to temperature below -2oC for more than one hour without proper clothing [2, 3]. Pathophysiology of frostbite is multifactorial.
Age of the patient, history of smoking, previous exposure to cold injury, altitude exposure, duration of exposure, tissue wetness, vascular insufficiency and any underlying pathology – all are critical attributes in the pathophysiology of frostbite [4]. It has been studied that ‘Thromboxanes’ and ‘Prostaglandins’ play an important role in the pathogenesis of this specific entity [5].
The classification of frostbite depends on the depth of tissue involved. Superficial frostbite includes 1st and 2nd degrees and deep frostbite includes 3rd and 4th degrees [6]. Superficial frostbite affects the skin and subcutaneous tissues whereas deep frostbite affects deeper structures viz. bones, joints and tendons [7]. Well established, definite treatment modality is still under consideration. Adjunctive therapies viz. Anti-prostaglandin agents, vasodilators, thrombolysis, sympathectomy and improved rewarming techniques are the available treatment options that are being used in the early phases of frostbite [6].
Hyperbaric oxygen is a form of therapy that has been used worldwide with exponential growth in acceptance for the treatment of wide array of diseases, ranging from decompression sickness to diabetic foot. It is performed by means of breathing 100% oxygen using an endotracheal tube, mask or hood in a completely isolated compression chamber by raising the ambient pressure to higher than 1 absolute atmosphere (ATA) [8]. Neither UHMS guideline nor European Society of Hyperbaric and Underwater Medicine guideline recommend HBOT as treatment modality for frostbite [9, 10]. Although available literature is sparse, quite a few case studies have come up with the fact that HBOT can be used effectively to treat frostbite cases.
Case details
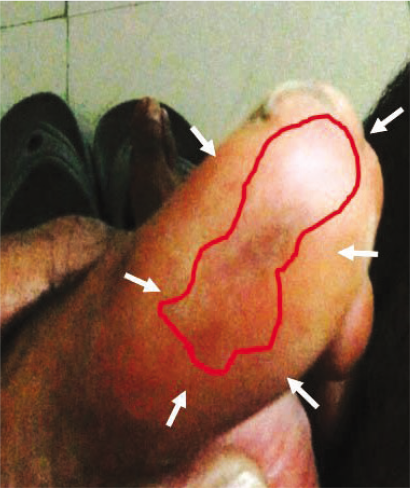
A 38 year old nonsmoker, teetotaler, experienced mountaineer with no known comorbidities felt sensory loss and dragging pain over great toe, second, third toe of the left foot and great toe, second toe of the right foot while on expedition to Mount Saifee (altitude 6,200m). The expedition included a trek of about 100km over a month. On the summit day, wind velocity was 25-30 nautical miles/ hr and ambient temperature was approximately -20˚C. He had a quarter pack of noodles and around 1.5 liter of water in the preceding 24 hrs. However, he ignored the numbness and dragging pain in his feet. Subsequently, within next two days, he noticed dark discoloration on the plantar surface of the left great toe (Fig 1) and sharp pain in both feet at the affected regions. He was treated with Tab Pentoxyphyline 400 mg twice daily. Within next couple of days his symptoms worsened with numbness, sharp pain and deep seated dark discoloration of the affected parts despite taking prescribed medications and warming of the limbs. After returning from the expedition, on the 9th day, he was evaluated by Reconstructive surgeon and Rheumatologist. Since there were no established guidelines regarding applicability of HBOT in vasculitis cases (except few case reports) [11], he underwent blood tests for vasculitis markers to rule out that possible aspect. His routine blood investigations, RFT, LFT, ESR, CRP, ANA, cANCA, Anticardiolipin antibody tests were within normal limits. Colour Doppler study of both lower limbs suggested decreased vascularity in the affected area and was considered as supportive evidence for confirmation of the diagnosis. After ruling out the possible diagnosis of vasculitis, he was managed conservatively as a case of superficial frostbite with Pentoxyphyline, NSAID, Clopidogrel and multivitamins in optimum dosage. Due to inadequate treatment response, he was recommended to undergo HBOT. With adequate precautions and mandatory evaluations, first session of HBOT was started on 12th day after summit. HBOT was administered every day with 2.5 ATA pressure for 90 min (five days a week). He underwent 11 sessions of HBOT uneventfully with break in treatment for four days on two different occasions and was closely monitored before, during and after each session. He was assessed with ‘Galer Jensen Neuropathic Pain Scale’ after each session. From the sixth session onwards objective assessment (Fig 2) and clinical profile suggested significant subjective improvement which was documented in the serial neuropathic pain scale.
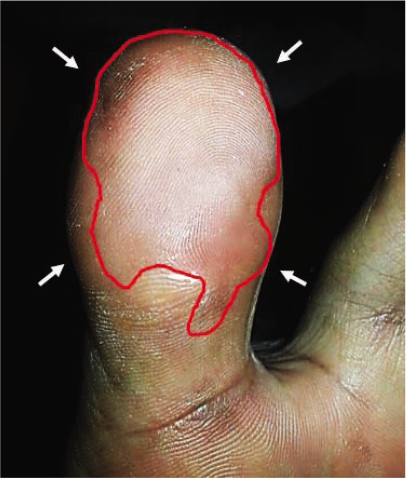
- Before HBOT (Black discolouration)
- After 6th session (Partial response)
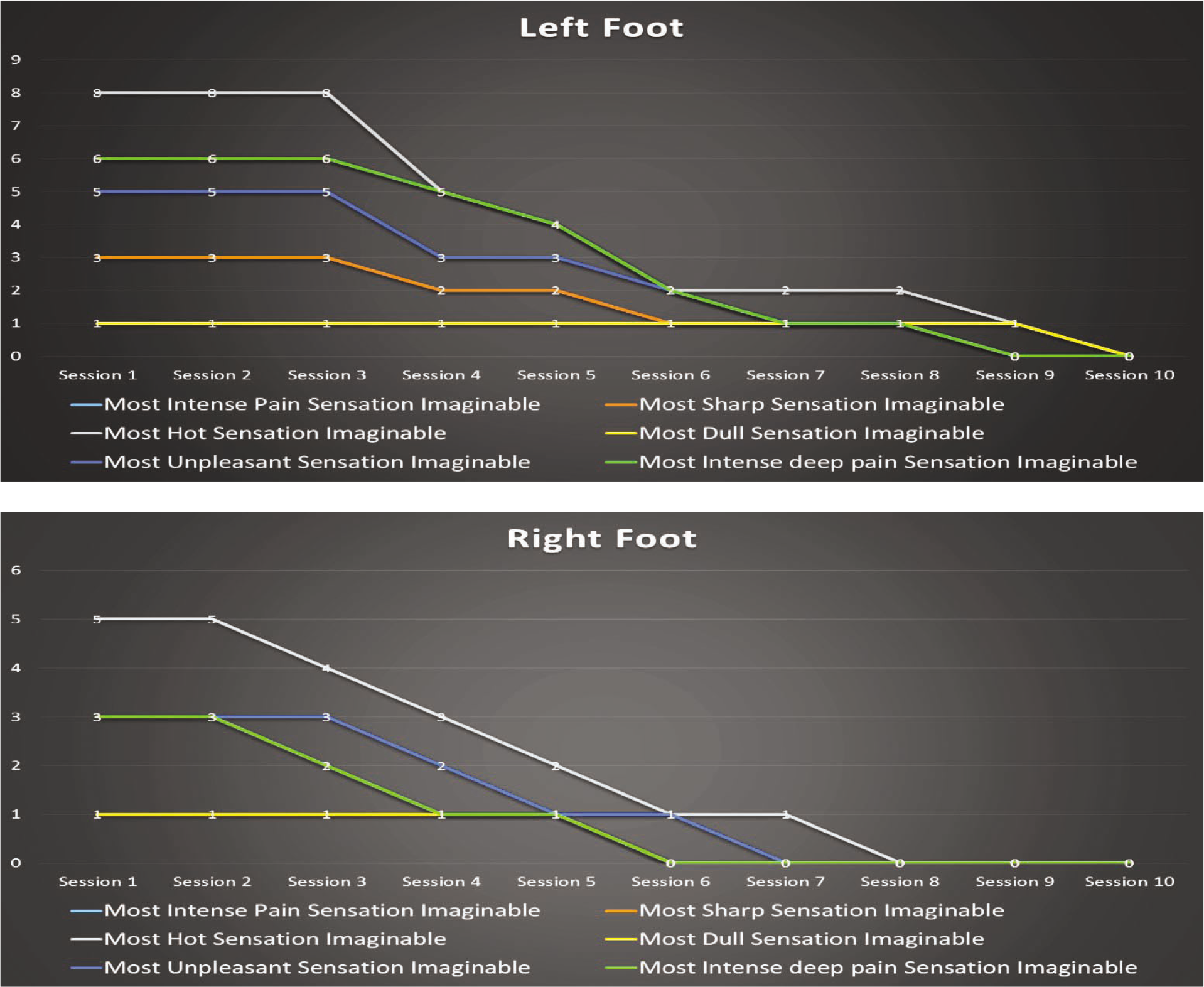
By the time of discharge, he became asymptomatic as documented in Galer Jensen neuropathic pain scale with resolution of dark discoloration in the lower limb as well (Fig 3). There was no tissue loss and all the affected toes regained their sensitivity. Full clinical recovery was achieved at the end of the 11th session of HBOT. Regular follow up was complementary to his asymptomatic clinical status.

- After 10th session (Significant response)
Discussion
Most common anatomical sites susceptible to frostbite are the extremities and to be more specific - 19% upper extremity, 47% lower extremity and 31% percent combined upper and lower extremities [11]. Other susceptible sites are the ears, nose, cheeks and penis. Multiple studies from public domain have come up with the fact that adults aged between 30 and 49 are most commonly affected with frostbite when compared to elderly and adolescents. This could be due to more participation in mountaineering by this group who are ultimately exposed to the freezing environment. Immediate treatment of frostbite consists of rewarming of the affected site with warm water (40-42˚C) over 15-30 min with antiseptic solution [5, 12]. The affected extremity must be elevated and splinted immediately to reduce oedema and promote tissue perfusion [7]. Tetanus prophylaxis and analgesics (Ibuprofen, Morphine) have to be provided and the affected areas should be protected from further exposure to cold environment [12]. Although the supporting evidence is limited, existing literature suggests the use of tissue Plasminogen activator (tPA), Heparin, Ilioprost, Low molecular weight dextran and Buflomedil (Alpha blocker) in frostbite cases [12].
Tissue damage in freezing occurs by two means: cellular damage and vascular insufficiency [7]. Slow freezing leads to the emergence of more ice crystals in the extracellular space than in the intracellular space [5]. Extracellular ice crystals cause dehydration of cells, which leads to protein denaturation, inhibition of DNA synthesis, loss of cell membrane integrity and finally cellular death. Cold causes increased blood viscosity and vasoconstriction leading to thromboembolism [7]. Inflammatory leukocyte infiltration, liberation of free oxygen radicals, prostaglandins and thromboxane also play significant role in the pathogenesis of frostbite [5, 6]
Available literature concerning the use of HBOT in human frostbite cases is sparse [13, 14, 15, 16, 17, 18]. Although randomized controlled trials are lacking on this aspect of treatment, all the existing studies and reported cases have been suggestive of a positive outcome. From a review of 21 cases of frostbite, it was reported that though the initiation of the therapy was delayed ranging from days to weeks, HBOT helped in hastening the formation of line of demarcation, helped in complete healing of wound in all the cases and neurological symptoms disappeared after 10-23 sessions of treatment [19]. Standard HBOT protocol followed at IAM is 90 mins of each session which includes 40 mins of therapy with 2.5 ATA pressure and 2 ft/ min ascent/ descent rate for 25 mins each (Fig 6).
- Session wise graphical representation of Galer Jensen Neuropathic Pain Score
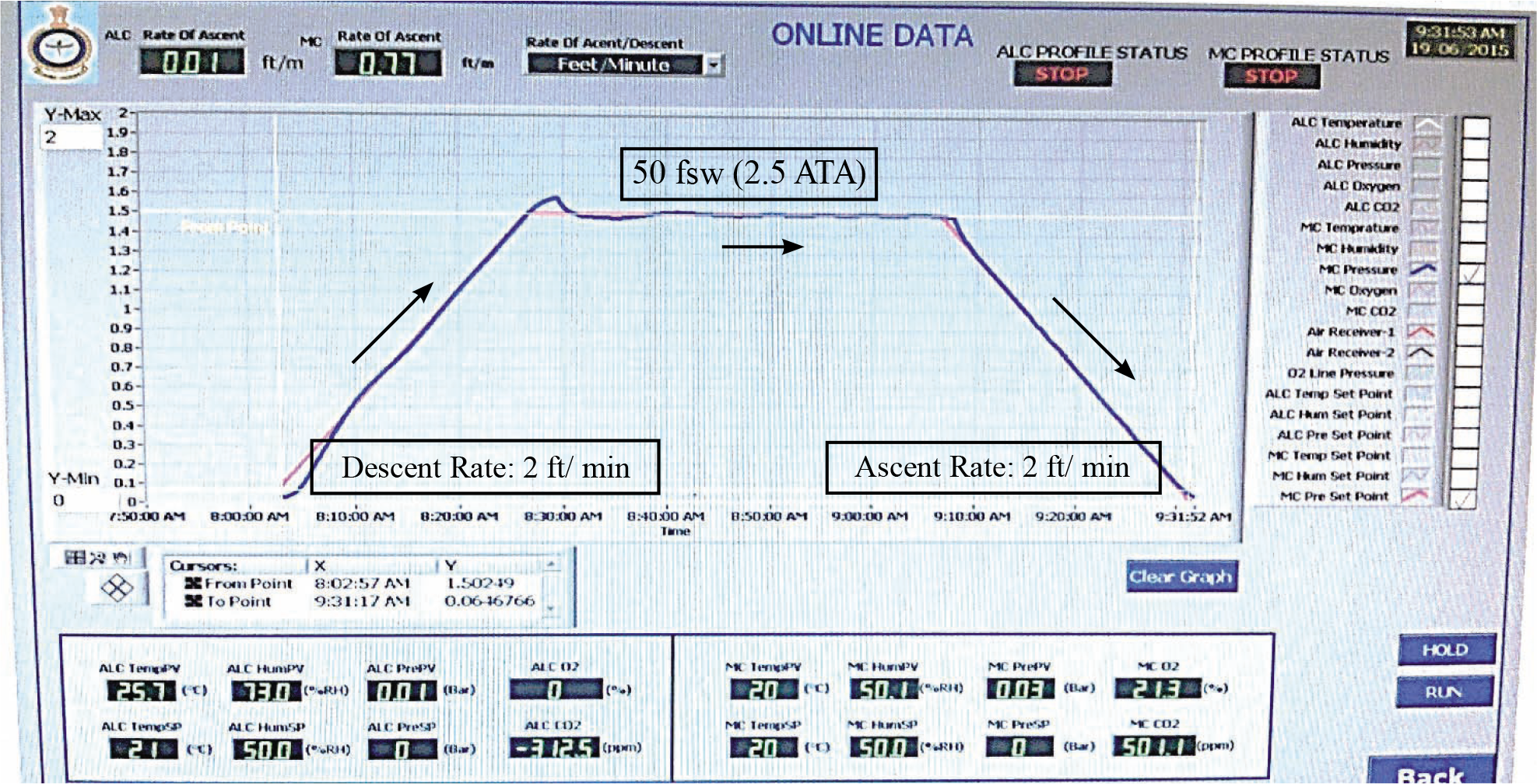
- HBOT profile
Compromised local blood supply in the background of raised metabolic demand results in hypoxic and acidotic wound environment with high lactate levels. The underlying pathophysiology is the sum of three factors - decreased O2 supply due to vascular damage with coagulation, increased metabolic demand due to heightened cellular response (anaerobic glycolysis) and aerobic glycolysis by inflammatory cells. Moreover, susceptibility to infection gets increased leading to compromised healing. Optimal function of neutrophils (primary cell responsible for non-specific immunity) depends on high partial pressure of oxygen. It is due to Reactive Oxygen Species (ROS) which are the major component of bactericidal defense. HBOT increases angiogenesis by virtue of vascular endothelial growth factor (VEGF) production. The capillary endothelial response to angiogenic factors viz. migration into wound, tubule formation, connecting to sources of blood flow is proportional to partial pressure of O2 in the artery along with blood perfusion. The matrix for neovascularization is produced by fibroblast. Although replication and migration of fibroblast depends on growth factors and chemo-attractants, production of mature collagen requires O2. Post-translational modification by prolyl and lysyl hydroxylases helps collagen peptides to aggregate into triple helices which is responsible for tissue strength. The activity of hydroxylases is critically dependent on tissue O2 tension. Hyperbaric oxygen induced soluble Nitric oxide radical is believed to be an important factor in healing [20]. Neovascularization happens by virtue of increased oxygen gradient between the wound and surrounding tissue, increased fibronectin and enhanced collagen deposition. Studies from public domain have correlated the effect of hyperbaric oxygen with increased elasticity of RBC, leukocyte bactericidal activity, resistance to infection, growth of new capillaries, collagen synthesis as well as storage in wound healing [21, 22] by increasing the normal level of tissue oxygen pressure to 10-15 times. Simultaneously, it regulates microcirculation and reduces oedema by causing vasoconstriction without occurrence of hypoxia [8].
In this case, the individual had a number of contributory risk factors for the development of frost bite.
Susceptible age of the individual
Extreme fatigue
Prolonged exposure to subzero temperature (Although the individual had proper trekking gear, the average ambient temperature was approx. -20˚c)
Inadequate hydration (Only 1-1.5 L water intake in the preceding 24 hrs)
Possible sweating inside the shoes
Possible tight shoes and cramped position
Moreover, the individual ignored the symptoms initially and hence proper rewarming and avoidance of the contributory factors could not be ensured at the initial stage.
Haemorrheologic agent, antiplatelet drugs, NSAID and vitamin supplements failed to yield optimal clinical outcome. But when HBOT was added as an adjunct therapy, the result was obvious from sixth session onwards with an impressive clinical recovery as depicted in serial Galer Jensen neuropathic pain scale. However, three different aspects of pain viz. ‘most cold, itchy and sensitive sensation’ were absent in both the limbs since the onset of the disease. After 11th session of HBOT, the individual attained full clinical recovery without any neurovascular deficit. The scores from the scale, measuring different aspects of pain have been depicted in the Fig 4 and Fig 5. Session wise time quality of pain has been described in Table 1.
| Session No. | Feeling of background pain ‘all the time’ & occasional Flare ups ‘some of the time’ | Feeling of single type of pain ‘all the time’ | Feeling of single type of pain ‘sometimes’; ‘Othertimes’- Painfree |
|---|---|---|---|
| 1 | - | Burning with foreign body sensation | - |
| 2 | - | Burning | - |
| 3 | - | Burning | - |
| 4 | - | Mild burning | - |
| 5 | - | Mild burning | - |
| 6 | - | Mild burning | Burning (No pain - Rt toe) |
| 7 | - | - | Burning (No pain at all) |
| 8 | - | - | Burning (No pain at all) |
| 9 | - | - | Mild burning (No pain at all) |
| 10 | - | - | No pain at all |
After resolution, the individual continues to be asymptomatic for last 14 months without any medication and has completed another mountaineering expedition without any discomfort.
Conclusion
In frostbite a certain number of cells are injured irreversibly but a large number of cells are injured reversibly. The reversibly injured cells may recover and survive with appropriate treatment [23]. In the early stages of freezing, hyperbaric oxygen can assist in salvaging a greater amount of tissue by increasing the viability of reversibly damaged cells neighboring the necrotic tissues by preventing tissue hypoxia and reducing tissue oedema. In the late stages, it can shorten the duration of hospitalization and can reduce the development of secondary infection by accelerating wound healing.
Galer Jensen Neuropathic pain scale which has been used to quantify pain and perform objective assessment of recovery, can be used in similar cases to assess and monitor treatment response. Though standard HBOT guidelines are mute regarding applicability of HBOT as definite or adjunct therapy in frost bite cases, many recent case studies have demonstrated the beneficial effect with excellent outcome. It supports the evidence based approach regarding the applicability of HBOT in such cases. Since Indian Armed Forces are hugely involved in high altitude mountain warfare including operations at glaciers, the soldiers are inevitably exposed to high risk environmental factors. From Indian perspective, it is strongly recommended to formulate our own HBOT guideline which can include ‘not so well established’ indications as well as can encourage the use of available single or multiplace chambers for potential benefits of the patients. Appropriate use of HBOT in lowest possible time for frostbite cases irrespective of the severity of injuries is immensely important to salvage the reversibly injured viable tissues.
References
- New horizons in management of hypothermia and frost bite injury. Surg Clin North Am. 1991;71:345-370.
- [Google Scholar]
- Effectiveness of resistive compared to passive warming in treating hypothermia associated with minor trauma: A randomized controlled trial. Mayo Clin Proc. 2001;76:369-375.
- [Google Scholar]
- Cold induced injury: Frostbite In: Herndon DN, ed. Total burn care. London: WB Saunders; 1996. p. :408-414.
- [Google Scholar]
- The physiologic effects of hyperbaric oxygenation In: Kindwall EP, Whelan HT, eds. Hyperbaric medicine practice (2nd revised.ed). USA: Best Publishing Com; 2002. p. :37-69.
- [Google Scholar]
- Accessed on 05 Jul 16http://www.uhms.org/resources/hbo-indications.html
- The guidelines of the European Society of Hyperbaric Medicine, the Society of Underwater and Hyperbaric Medicine and the National Health Fund Polish Republic on a hyperbaric oxygen therapy (HBOT) in 2013. Journal of Heath Sciences. 2013;3(9):125-134.
- [Google Scholar]
- Hyperbaric oxygen therapy for nonhealing vasculitic ulcers. Clin Exp Dermatol. 2007;32(1):12-17.
- [Google Scholar]
- An algorithm for early agressive treatment of frostbite with limb salvage directed by triple-phase scanning. Plast Reconstr Surg. 1998;102:1069-1074.
- [Google Scholar]
- Some clinical and experimental applications of high pressure oxygen. Proc Roy Soc Med. 1963;56:999-1002.
- [Google Scholar]
- Hyperbaric oxygen treatment in deep frostbite of both hands in a boy. Burns. 2001;27:404-408.
- [Google Scholar]
- Frostbite: General observations and report of cases treated by hyperbaric oxygen. Proc Roy Soc Med. 1968;61:787-789.
- [Google Scholar]
- The treatment of deep frostbite with hyperbaric oxygen. Injury Extra. 2005;36:499-502.
- [Google Scholar]
- Hyperbaric oxygen treatment in deep frostbite of both hands in a boy. Burns. 2001;27(4):404-408.
- [Google Scholar]
- Use of Hyperbaric oxygen therapy in Frost Bite-A review of cases. Ind J Aerospace Med. 1988;32(1):33-40.
- [Google Scholar]
- Oxygen and the basic mechanism of wound healing In: Tom SN, Stephen R, Thom, eds. Physiology and medicine of hyperbaric oxygen therapy (1st ed). 2008. p. :205-211.
- [Google Scholar]
- Successful treatment of frostbite with hyperbaric oxygen treatment. IJOEM. 2015;19:121-122.
- [Google Scholar]
- Enhancement of healing in selected problem wounds In: Feldmeier JJ, ed. Hyperbaric oxygen 2003 Indications and results: The Hyperbaric Oxygen Committee Report. Kensington: Undersea and Hyperbaric Medical Society; 2003.
- [Google Scholar]






