Translate this page into:
Intractable Air Sickness in Trained Fighter Aircrew: Dilemma in Aeromedical Decision Making
Abstract
Background:
Air sickness (AS) in trained aircrew is unusual, whereas it is a well-known phenomenon amongst the neophyte pilots during their early days of flying training. Subjective assessment for AS and it’s desensitisation for aeromedical disposition in a trained aircrew might not always be rewarding.
Case Report:
A young trained fighter aircrew with active flying career of 06 years and total flying experience of about 350 hours was referred to the Aeromedical Boarding Centre for the evaluation and desensitization for AS. History revealed that the aircrew was experiencing recurrent episodes of AS since his training days, which was never reported to the concerned authority neither by aircrew himself nor by his supervisor. The problem evolved significantly when he recommenced flying after a long break due to certain other medical and psychological issues. A thorough medical and psychological evaluation was carried out at the Boarding Centre and he was subjected to desensitization therapy which could not be completed successfully.
Discussion:
A number of aeromedical issues surface with regard to this particular case report which has been brought out and discussed in this paper. Lack of objective assessment modalities and possibility of easy feigning the symptoms of air sickness in a trained experienced fighter aircrew with psychological accompaniment poses a big challenge to the Aerospace Medicine fraternity to conclude for an apt aeromedical disposition. The main concern is not only losing a trained aircrew but also the uprightness of aerospace safety.
Conclusion:
Air sickness is a perennial aeromedical problem. Objective modalities need to be further emphasized for realistic assessment of AS cases. In genuine cases, a psychotherapeutic element should reassure the individual that AS is not a manifestation of personal weakness or lack of moral fibre.
Keywords
Air sickness
desensitization
training
flying
Introduction
Air sickness (AS) is a debilitating condition that adversely affects the performance of an aircrew which leads not only to distraction but also interferes with his ability to accomplish the task assigned. AS is a well-known phenomenon amongst the neophyte pilots during early days of flying training. Symptoms like vomiting interfere directly with the student’s ability to control the aircraft and can culminate into aborting a sortie. When AS is not overt, the student may suffer in silence and it could be at the cost of compromising aerospace safety [1].
Institute of Aerospace Medicine (IAM), Indian Air Force (IAF) offers Motion Sickness Desensitization Therapy (MSDT) programme for the management of such cases. The programme comprises of graduated exposure of the aircrew to the rigorous motion stimuli over a period of time in the simulator, accompanied by Physical Exercise Training (PET), Progressive Muscle Relaxation (PMR) and Yogic exercises under supervision. The success of this programme is determined by the individual’s ability to tolerate the progressively increasing motion stimuli from 5 to 25 rpm without any symptom. This program has a success rate of 79.41 %, which is similar to that of the other programmes being followed by other countries across the world [2].
AS occasionally occurs in an experienced aircrew as they switch aircraft types, particularly in higher physical stress aircraft (heat, low level, limited visibility, etc.). AS may also occur when a previously adapted individual returns to duty after an extended period of non-flying. Severe AS in a trained aviator is unusual, even in a provocative flight environment [1]. In this paper, a rare case of Intractable Air sickness in a trained aircrew has been discussed, who could not be desensitized with the existing MSD protocol and was recommended permanently Unfit for flying duties.
Case Report
A 29 year old apparently healthy trained fighter aircrew with active flying career of six years and a flying currency of approximately 350 hours was referred to the Aeromedical Boarding Centre for the evaluation of Airsickness. A detailed history revealed that, the aircrew, during his initial flying training had experienced nausea and even vomited in the aircraft during the aerobatic training. These incidents were neither recorded in his performance book nor brought to the notice of the concerned medical authorities. However, he could endure the ab-initio training until successfully completed. The officer also states that, he had puked in the aircraft and had to abort several planned sorties during the subsequent stages of advanced flying training in two other aircraft as a part of the training schedule for fighter aircrew. The aircrew continued to have similar symptoms in flight throughout all instructional as well as aerobatic phases but denies of being symptomatic while flying simulators and solo sorties. The aircrew reports that, these were not recorded in the performance book and he was not referred for any treatment.
After the successful (?) fighter flying training of two years the aircrew got commissioned and was posted to a fighter squadron. Even while flying in the frontline fighter aircraft, he had similar symptoms involving a dual cockpit because of which the sorties were aborted on two different occasions. However, he remained asymptomatic in the solo sorties. At this juncture, he remained off flying for a period of approximately 04 years, as he suffered from Bell’s palsy followed by marital discord. Once he recovered from the disability and his domestic issues were settled, the aircrew returned back to flying.
After a few sorties, he became symptomatic again and at that time he was brought to the notice of Aerospace Medicine Specialist at the Squadron and was observed on ground for a while. The aircrew complained of AS on multiple occasions during the sorties flown to obtain an Executive Report on flying for recommencement of his flying duties. The symptoms were mainly observed during the aerobatic manoeuvres while he was not on the active control of the aircraft. His Executive Report also brought out that his performance was inconsistent and following which he was recommended to undergo aero-medical evaluation for AS before resuming his flying duties [3].
Aeromedical Evaluation
At the Aeromedical Boarding Centre, the aircrew was subjected to a complete haematological and biochemical assessment. Thereafter, a comprehensive evaluation by the Medical & ENT Specialists was carried out to rule out any organic cause for his AS. The differential diagnosis of AS is presented in Figure 1 [4].
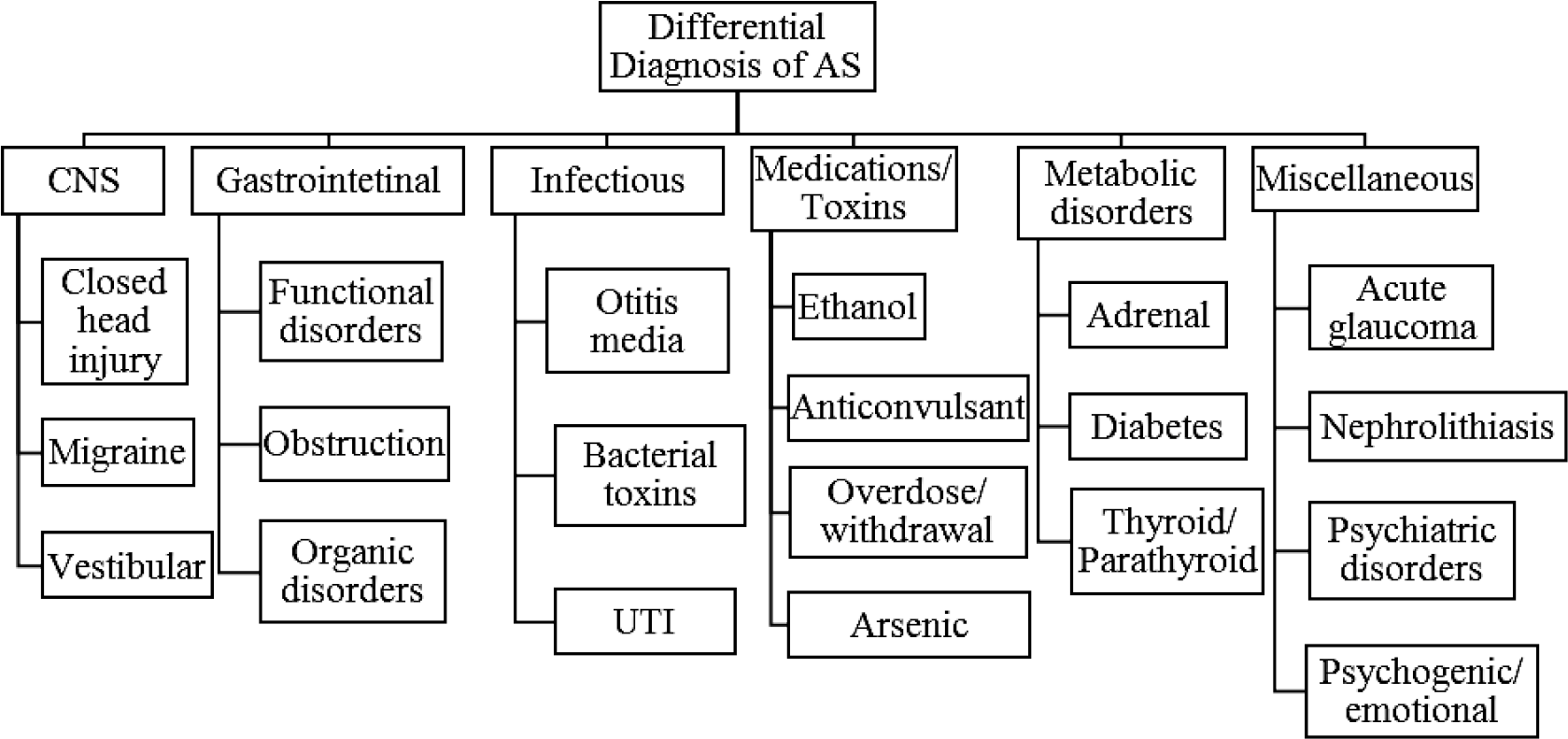
- Differential Diagnosis of Airsickness
The Aviation Psychologist also carried out an in-depth psychological evaluation to identify any psychopathology, maladaptive coping, vulnerability types (Gastrointestinal, Central, Peripheral and Sopite) and for overall motion sickness assessment. The aircrew was not reviewed by any Psychiatrist as the psychological evaluation was conclusive. Subsequently, the standard protocol of Motion Sickness Desensitisation Therapy (MSDT) of IAM was initiated using AIRFOX-DISO (ground based disorientation simulator) [5]. The Aircrew failed to complete the Desensitisation protocol because of which he was made unfit for flying duties.
Desensitization Protocol
With a prior assumption that the vestibular adaptation would improve [5,6,7], the aircrew was subjected to the combination of the following in the MSDT protocol as shown in Figure 2.
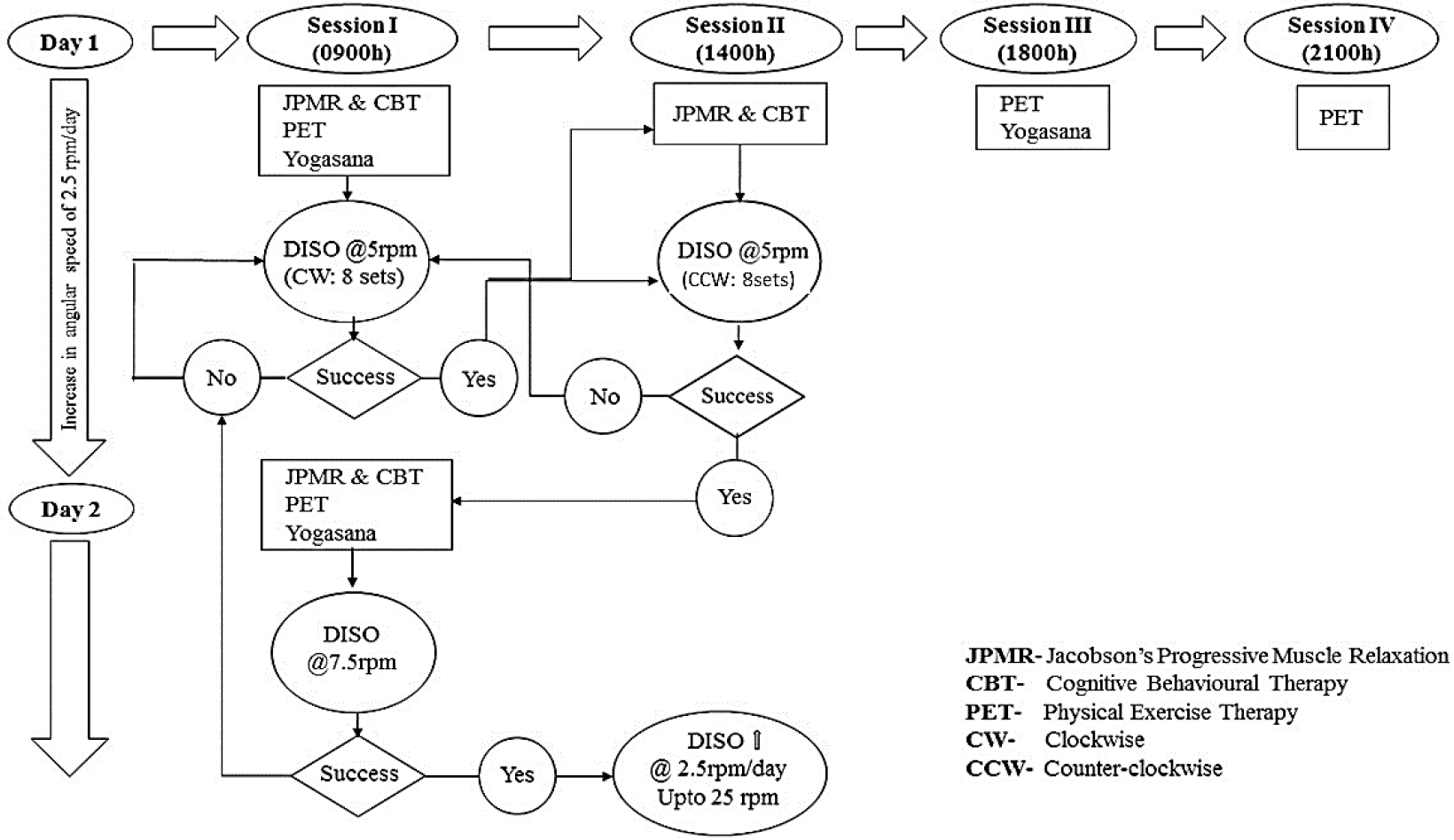
- IAM MSDT Protocol overview
Prior to the commencement of actual MSDT protocol, the aircrew was familiarized and was subjected to AIRFOXDISO simulator runs wherein, he could sustain well in a free flight run involving aerobatic manoeuvres in DISO simulator both in active and passive mode.
Exposure to graded increments of rotation (clockwise and counter-clockwise direction) was simulated with head movements in four planes to induce coriolis sensation on the AIRFOX-DISO simulator in the Coriolis Barany Chair mode. The desensitization in the DISO simulator was initiated at an angular speed of 5 rpm (30 degree/sec) as per standard protocol. It was gradually incremented by 2.5 rpm (15 deg/sec) per day. Failure to tolerate the complete protocol in a particular rpm reverted him back to the previous rpm in the subsequent session. The PET, PMR and Yogic exercises were conducted under supervision.
Throughout the therapy period the aircrew was suggested to practise a healthy diet, good night’s sleep, not to consume alcohol and not to smoke. During the MSDT protocol, the Coriolois Time Interval (CTI) and a Motion Sickness Rating Scale (MSRS) were recorded in each DISO run. MSRS is a 07 point Likert scale where a rating of 01 indicates no symptoms; and 07 indicates moderate symptoms and wants to stop [8].
MSDT Outcome
The aircrew could only reach a maximum of 7.5 rpm (45 deg/sec) by the 6th day of the Desensitization Therapy. The MSDT was suspended in view of persistence of symptoms of nausea and three episodes of emesis during this period. The results of coriolis simulation is shown in Table 1.
| Day | 0900h | 1400h | ||||
|---|---|---|---|---|---|---|
| rpm | MSRS | CW Rotation | rpm | MSRS | CCW Rotation | |
| 1 | 5 | 2 | Completed | 5 | 6 | Aborted |
| 2 | 5 | 2 | Completed | 5 | 3 | Completed |
| 3 | 7.5 | 4 | Aborted | 5 | 4 | Completed |
| 4 | 7.5 | 3 | Aborted | -- | -- | |
| 5 | 7.5 | 4 | Completed | 7.5 | 5 | Aborted |
| 6 | 7.5 | 6 | Aborted | -- | -- | |
Discussion
Air sickness or kinetosis is a perennial aeromedical problem. AS is caused by unfamiliar (unadapted) motion stimuli and particularly, by inter sensory perceptual incongruences among the visual, vestibular and somatosensory systems [9]. It is a complex clinical syndrome, characterized by various initial symptoms and signs, such as sweating, pallor, drowsiness, paraesthesia etc. which induce nausea or/and vomiting over sufficiently prolonged exposure to appropriate stimulation. In some cases, prodromal symptoms are missing, and the patient immediately experiences distress accompanied by retching and vomiting.
AS is incompatible with flying duties, hence such cases need to be desensitized before they return to their duty. Many authors have emphasized the critical importance of ‘successful’ desensitization and early reflighting of an air sick aviator. However, on detailed review of different MSD programmes, the lack of an acceptable definition of ‘success’ made it difficult to compare one programme with another. ‘Success’ can be defined as: completing the MSD protocol, returning to flying training, successfully completing basic flying training, or successful operational conversion onto a front-line aircraft [10].
The aim of these desensitisation programmes is to accomplish a complete and permanent resolution of AS symptoms in each subject. Unfortunately, this cannot always be achieved, due to factors related to individual characteristics and to the particular environment to which he/she is exposed. Besides the inter-individual variability of the clinical outcome, in any therapeutic approach (viz. MSDT), other factors may influence the final result of these programmes, such as prolonged absence from potentially nauseogenic motion stimuli, which paradoxically are the environmental situations that best prolong the benefits of rehabilitation, acting on retentivity.
A number of issues surface with regard to this particular case report which pose a challenge to the Aerospace Medicine fraternity, some of which are enumerated below:
Is the aircrew using this ‘easy to feign’ condition to quit flying?
Are the associated conditions (medical/personal) contributing to the aetiology as well as the prognosis of his air sickness?
Is there any fear / anxiety of being humiliated or disgraced within his community, which is stopping him from returning to flying?
Do we have an effective objective technique to prove, that the case is genuine?
Is there any valid method to screen such susceptible cases during the selection itself?
Is there any role of pharmacotherapy in treating such a chronically airsick aircrew?
Symptomatic in Dual sortie, but comfortable in Solo: Is it a consequence of Crew Resource Mismanagement?
Was the aerospace safety jeopardised all these years since the onset of his airsickness?
A few of these issues have been discussed in this paper to highlight the dilemma in aeromedical decision making in such cases.
1. Is the aircrew using this ‘easy to feign’ condition to quit flying?
Three situations point towards a possibility that the aircrew might have feigned. Firstly, the aircrew rated his most recent Airsickness experience to be very low on Motion Sickness Assessment Questionnaire during his last sortie indicating that he may not be prone to severe motion sickness [8]. Secondly, his psychological assessment indicated that he had low score on Disclosure Index and high score on Social desirability Index i.e. the officer portrays himself in the best possible way while being very reticent, guarded and secretive in his response. Thirdly, the officer was able to complete his entire flying training and has logged a total of 350 hrs of flying till date which includes aerobatics as well, even though he claims to have recurrent symptoms (?) of air sickness which were neither documented (unlikely…) nor he was referred to medical authorities inspite of emesis in cockpit (?).
2. Are the associated conditions (medical/personal) contributing to the aetiology as well as the prognosis of his air sickness?
The three factors: Receptivity, Adaptability and Retentivity represent the essential baselines for rehabilitation in AS. The aircrew in this case suffered from Bell’s palsy and marital discord, because of which he was off flying for approximately four years. Such a long break from flying might have negatively affected his adaptability and retentivity which was acquired during his regular flying sessions.
This non-flying period along with psychological stress of marital discord and other domestic issues could have aggravated his covert/suppressed symptoms. The psychological stressors are well known precipitators for AS and it is also possible that all these could have cumulatively resulted in Loss of Motivation for Flying.
Review of literature suggests that the rehabilitation programmes for AS are very tiring procedures which are based on inducing nausea through specific exercises and simulator runs and is, therefore, only recommended for highly motivated individuals [10]. The Low Motivation for flying and partial insight revealed in the psychometric assessment could have resulted in failure of MSDT in this case.
In addition, the role of other factors which result in high individual variability in susceptibility to air sickness viz age, sex etc. also cannot be disregarded.
3. Is there any fear of being humiliated or disgraced within his community, which is stopping him from return to flying?
The performance of the student pilot would be impaired in flight as a consequence of AS and this could be attributed as lack of fundamental flying skill by the flying instructor. In either of the circumstances, the student might feel humiliated, left behind in the peer group and disgraced in his own community, which could be construed as a personal weakness or constitutional defect. A continued introspection with increasing anxiety and loss of confidence can further impair progress and may strengthen even the instructor’s opinion about the student’s lack of aptitude. In addition, he could be a case of ‘Manifestation of Apprehension’ (MOA). MOA is a term used in US Armed Forces to describe a state of anxiety, apprehension and/ or physical impairment exhibited by students towards their training environment. It is a feeling of danger from within and in the absence of a dangerous situation the subject does not know exactly, of what and why he is afraid [11].
4. Do we have an effective objective technique to prove that the case is genuine?
AS is a normal physiological response of body to abnormal motion stimuli and unfortunately methods for clinical testing to accurately predict the sensitivity of each individual to AS are currently lacking. Furthermore, pharmacological prevention is contraindicated in aircrew whose cognitive tasks involve high level of vigilance. Therefore, applicability of some objective techniques such as Electrogastrogram, Videonystagmography, Vestibular Evoked Myogenic Potential (VEMP), Phasic skin conductance activity and Autogenic nervous system response monitoring etc. to identify those responses need to be explored [10, 12].
5. Is there any valid method to screen such susceptible cases during the selection itself?
Incidence of Air sickness amongst trainee pilots is a major problem at any Basic Flying Training Establishment. Attempts at pre-selection weeding out by questionnaire and past history are not successful largely due to gross under reporting [13]. An air sick trainee may have poor learning due to performance decrement; and if not treated it may lead to possible suspension from flying training. Any disqualification of a pre-solo trainee is a huge economic burden [14]. Heretofore, there exists no functional guide that can serve as a screening tool for individual susceptibility to AS. Thus, it is understood that reliable methods of preliminary investigation and selection of individuals are currently lacking.
6. Is there any role of pharmacotherapy in treating such a chronically air sick aircrew?
From a practical point of view, a more realistic method is to allow each individual to become adapted to the specific nauseogenic environment, and to treat only those few cases (slow adaptors) who have not adapted after an adequate exposure time. While some anti-motion sickness medications provide reasonable efficacy, adverse neuro-cognitive effects limit their use in military personnel engaged in safety critical operational roles such as flying.
In neophyte aviators, pharmacological intervention may accelerate this adaptation. One of the most effective medications is Scopadex (25 mg of Scopolamine hydrobromide with 5 mg of Dexamphetamine). Another effective medication is Promethazine (25 mg) with Ephedrine (25 mg). Pharmacological intervention is a temporizing measure and a positive effect should be seen within three to five doses, and should be used in conjunction with continued flight training to be maximally effective. Therefore, in a slow-adapting aircrew, rehabilitation techniques are preferred [15].
7. Symptomatic in Dual sortie, but comfortable in Solo: Is it a consequence of Crew Resource Mismanagement?
Crew pairing in a dual seat cockpit is an important factor in aviation, more so in military aviation, when it concerns both ab-initio and continuity training. Personality of the instructor pilot can at times overwhelm the responses of the pupil pilot and therefore disrupt cockpit resource management, so crucial in safe flying. This may lead to decrement of both situational awareness and airmanship not only during an emergency situation but also in routine sorties. Therefore, the possible role of crew resource mismanagement in the present case also cannot be simply overlooked [16].
8. Was the aerospace safety jeopardised all these years since the onset of his air sickness?
Any pilot considering a fitness for duty should be able to rely on the medical authority for legal and ethical handling of his or her situation with confidentiality, dignity and respect; to expect compatibility with the aerospace safety; and to find maximum employment benefits. This includes assurance at the outset that if a treatable medical condition is discovered the pilot’s medical status will be protected.
Fear of being medically downgraded, might have played a role throughout the training period which prevented him from disclosing to the medical authority and so he continued flying with symptoms of AS. The effects of AS can range from distraction to near incapacitation. The corresponding degradation of Situational Awareness and performance is incompatible with flying duties. If an aircrew continues to fly in such a condition, then aerospace safety is definitely violated.
Aeromedical Disposition
The aeromedical decision making (ADM) on a particular medical disability in an aviator is broadly based on following issues:
Determine the likelihood of a clinically significant event from the health condition.
Determine the likelihood of an undesirable aviation event from the health condition.
Determine the acceptability of the combined risks (1 and 2).
Determine the risk level after clinical intervention for the health condition
Determine the risk level after operational restrictions for the health condition
These issues are affected by several factors such as uncertainty, difficulty in generalization, power and “fit” of the therapy, etc [17]. In IAF, the current guidelines for Aerospace Medicine specialist state that, on failure to complete MSDT protocol the aviator has to be made unfit for flying duties, once all other causes of AS has been thoroughly ruled out. The disposal hence, for such an aircrew is left with the administrative authority without downgrading the medical fitness category.
Lessons Learnt
The evaluation for AS needs to be comprehensive. It would be really unfair to the aviator if the medical fraternity does not look at all aspects of AS. This is because, if something is missed, then the aircrew faces a circumstance where he either returns to flying and performs poorly or he is not allowed to return to flying even if he had a potentially treatable medical condition.
The scope of research with available objective methods in combination with the subjective scoring (MSRS) for true validation of AS needs to be emphasized. The critical importance of assessing the correspondence between physiological responses and symptoms cannot be overemphasized. Clearly, the use of both, symptom reporting and physiological recording during desensitization would add greatly to our accuracy to assess both Airsickness and countermeasures. This will also ensure not only the uprightness of aerospace safety but also preserving an experienced aircrew.
In genuine cases, a psychotherapeutic element should also reassure the individual that AS is not a manifestation of personal weakness or lack of moral fibre.
Acknowledgement
The authors gratefully acknowledge the inspiration, permission and guidance extended by the Commandant, Chief Research Officer and Head of Department of Acceleration Physiology and Spatial Orientation, IAM to bring out the case study.
Disclaimer
The opinions expressed in this article are those of the authors and do not reflect the official views of the Indian Society of Aerospace Medicine.
References
- Motion Sickness In: Rainford DJ, Gradwell DP, eds. Ernsting’s Aviation Medicine (4th ed). New York: Edward Arnold Ltd; 2006. p. :137-158.
- [Google Scholar]
- Air sickness in trainee aircrew of Indian Air Force: Our experience with desensitisation. Ind J Aerospace Med. 2005;49(2):33-40.
- [Google Scholar]
- Yogic exercise as a prophylaxis to reduce airsickness and morbidity in ab-initio pilot trainees. Ind J Aerospace Med. 1996;40(2):17-21.
- [Google Scholar]
- Airsickness desensitization based on physical exercise therapy: Indian Air Force programme 1983-1993. Ind J Aerospace Med. 1995;39(1):11-14.
- [Google Scholar]
- A questionnaire for the assessment of the multiple dimensions of motion sickness. Aviat Space Environ Med. 2001;72:115-119.
- [Google Scholar]
- Vestibular functions in motion sickness susceptible individuals. Eur Arch Otorhinolaryngol. 2009;266:1365-1371.
- [Google Scholar]
- Increasing Accuracy in the Assessment of Motion Sickness: A Construct Methodology: NASA. 1993. Report No: TM-108797
- [Google Scholar]
- Phasic skin conductance activity and motion sickness. Aviat Space Environ Med. 1992;63(3):165-171.
- [Google Scholar]
- Air sickness in trainee aircrew of Indian Air Force. Ind J Aerospace Med. 1995;39(2):1-9.
- [Google Scholar]
- Motion sickness medications for aircrew: Impact on psychomotor performance. Aviat Space Environ Med. 2005;76:560-5.
- [Google Scholar]
- Trans-Cockpit Authority Gradient in Flying Training: A Case Report. Ind J Aerospace Med. 2004;48(1):41-46.
- [Google Scholar]
- Aeromedical decision making: From principles to practice. Aviat Space Environ Med. 2014;85(5):576-80.
- [Google Scholar]






