Translate this page into:
Unconjugated hyperbilirubinemia in commercial pilot: A clinical dilemma
-
Received: ,
Accepted: ,
Abstract
This paper discusses the case of a commercial pilot who was detected to have unconjugated hyperbilirubinemia during Class- I Medical Assessment and subsequently was referred to Institute of Aerospace Medicine for further evaluation and disposition. Cases presenting with mixed picture of benign disorder like Gilbert’s Syndrome along with evidence of hemolytic disorder and liver function test abnormalities can complicate the situation and pose diagnostic dilemma. A systematic approach would then be required for evaluation which subsequently will affect aeromedical disposition. This case is presented with aim of discussing approach and aeromedical implications in aviators.
Keywords
Unconjugated hyperbilirubinemia
Gilbert’s syndrome
Introduction
Unconjugated hyperbilirubinemia is a disorder of bilirubin metabolism consisting of overproduction, defective uptake or defective conjugation. Recognition of this condition is important in distinguishing it from hepatic and post hepatic causes of hyperbilirubinemia. Diagnostic dilemmas can arise in asymptomatic cases with lab investigations suggesting benign disorder like Gilbert’s Syndrome along with evidence of hemolytic disorder and liver function test abnormalities. Disabilities like hemolytic anemias, leading to a hemolytic episode can reduce tolerance to aviation stresses compromising flight safety. On the other hand, benign disorders like Gilbert’s syndrome pose little threat. Correct diagnosis, differentiating serious from benign causes is essential for appropriate disposition and briefing of aircrew. In aviation scenario undiagnosed cases with serious disorders or unawareness regarding precautions to be taken may lead to a catastrophic event.
Case Details
A 34 year old commercial pilot with 1500 hrs of flying experience reported to the company doctor for renewal medical of Commercial Pilot Licence (CPL) with Liver Function Test (LFT) report. His LFT report showed raised total and indirect bilirubin. The pilot was aware of his jaundice and had done LFT on his own initiative. History revealed that he had an episode of Jaundice in 2004, which subsided on its own after a gap of one month. Barring LFT, no other investigation was carried out during past episode and no conclusive diagnosis was made. Pilot did not give any history of repeated episodes of Jaundice. In 2007, at the time of reporting he was asymptomatic, had no history suggestive of infections, active hepatic disease, medication or excessive alcohol intake. General and systemic examination was unremarkable except for icterus. There were no signs of chronic liver disease. He was thoroughly investigated for identifying the cause. Hemogram, PBS, urine examination and lipid profile revealed no abnormality. LFT revealed elevated S. Bilirubin levels (4.4 mg/dl), Indirect bilirubin (3.4 mg/dl) and ALT (73 U/L). Pilot tested negative for viral markers. USG abdomen showed grade–I fatty liver. Glucose 6 Phophate Dehydrogenase (G6PD) quantitative assay revealed decreased values of 4 units/gmHb (normal range – 4.6-13.5). Direct and Indirect Coomb’s tests were negative. Because of asymptomatic transaminitis and negative direct Coomb’s test which may be associated with Wilson’s disease, he was investigated on the lines of Wilson’s disease also. Initially serum ceruloplasmin levels at two occasions showed lower values and raised suspicion for Wilson’s disease but subsequent levels (after one week), S.copper and 24 hr urinary copper excretion were within normal limits without any evidence of Kayer-Fleischer rings in eyes.
Gastroenterologist and hematologist reported Gilbert’s syndrome as the primary cause and G6PD deficiency as the associated cause of asymptomatic unconjugated hyperbilirubinemia. Transaminitis was accounted for by NAFLD. He was grounded with effect from 18 Jul 07 and recommended evaluation at IAM.
During his evaluation at IAM, it was decided to follow up the individual periodically, for transaminitis to settle down with lifestyle modification, to conclusively rule out the possibility of Wilson’s disease and to ensure patient’s compliance with restrictions imposed for G6PD deficiency. He was recommended fit to fly as PIC along with an experienced qualified pilot. He was recommended monthly reviews by company doctor with LFT report. Raised ALT values subsided within two months. Subsequent investigations and reviews at IAM revealed persistent mild hyperbilirubinemia and lowered values of G6PD without any evidence of hemolysis.
He remained asymptomatic throughout the observation period (Feb 08 to Mar 09) and logged around 1100 hrs of flying. Laboratory and biochemical parameters did not show any deterioration, considering which he was given full flying category.
Discussion
Our pilot initially showed evidence of Gilbert’s syndrome, G6PD deficiency and Wilson’s disease. Wilson’s disease was ruled out after a follow-up period as pilot showed no symptoms, signs or lab manifestations indicative of copper hepatotoxicity. Mild transaminitis was better accounted for by mild NAFLD. Both G6PD deficiency and Gilbert’s syndrome were suspected as a cause for hyperbilirubinemia. In the absence of any substantial history of intake of provocative agent, past history of hemolytic episode and laboratory confirmation of hemolysis, Gilbert’s syndrome was favored as most probable cause for persistent hyperbilirubinemia. It is important to rule out G6PD deficiency as a cause for elevation of S. bilirubin, as it could lead to severe episode of hemolysis on exposure to provocative agent. Our pilot though aware of his raised bilirubin levels, was not adequately briefed about the probable cause and precipitating factors, which in an adverse circumstances would have led to an undesirable event.
Gilbert’s syndrome is the most common congenital hyperbilirubinemia syndrome, occurring in about 5% of population [1]. It is transmitted through an autosomal recessive gene. Its pathogenesis is related to a partial deficiency (10-30%) in hepatic UDP glucuronoyl transferase, the enzyme responsible for the glucuronidation of bilirubin. In addition, some patients have reduced bilirubin uptake by hepatocytes [1,2]. Other abnormalities that have been reported include mild and fully compensated state of hemolysis with increased haem turnover [3]. The syndrome is usually detected in adolescents and young adults, most commonly in males. Most of the cases are asymptomatic. Scleral icterus may be present and fluctuating, but the physical examination is otherwise normal. Liver tests and hemogram (to exclude hemolysis) are normal except for unconjugated serum bilirubin, which is elevated between 2 to 6 mg/dl, usually less than 3 mg/dl [1]. Bilirubin levels fluctuate and may be precipitated by dehydration, fasting, fatigue or stress, such as an intercurrent illness or vigorous exercise. Diagnosis is made by exclusion of other conditions by conducting specific diagnostic tests (Table 1).
| Causes | Diagnostic tests |
|---|---|
| 1. Hemolytic disorders | Hemogram and blood film: evidence of hemolysis, S.bilirubin <5mg/dl-Coombs test for immune hemolytic anemia-Enzymatic assays-G6PD, pyruvate kinase |
| 2.. Ineffective erythropoiesis | Hemogram and blood film, Elevated levels of S.iron ferritin and plasma LDH, Bone marrow – cellularity |
| 3. Drugs-Rifampicin, Probenecid, Ribavirin | LFT deranged, Liver biopsy |
| 4. Inherited conditions-Gilbert’s syndrome, Crigler-Najjar types I and II | LFT, S. bilirubin : 3-6mg/dl-Liver biopsy-Enzymatic assay - Nicotinic acid test} rare |
Other diagnostic tests are available but usually not necessary: fasting for two days or intravenous administration of nicotinic acid significantly increases serum unconjugated bilirubin, while Phenobarbital administration (enzyme inducer) significantly decreases it. No treatment is warranted and prognosis is excellent [1,2,3]. Other congenital hyperbilirubinemia syndromes like Crigler-Najjar Syndrome Type I (hepatic bilirubin UGT activity is undetectable) and Type II (hepatic bilirubin UGT activity is reduced) are typically detected in infancy. In some cases of CN Type-II, hyperbilirubinemia may appear later in life. It is rare and distinguished from Gilbert’s Syndrome by higher levels of indirect bilirubin (6-25 mg/dl) [1,2].
The differential diagnosis of an isolated unconjugated hyperbilirubinemia is limited (Table 1). The critical determination is whether the patient is suffering from a hemolytic process or from impaired hepatic uptake/conjugation of bilirubin.
G6PD deficiency is a form of hemolytic anemia, inherited as a sex-linked condition and thus affects only males. G6PD enzyme is pivotal in the Hexose Monophosphate Shunt and produces NADPH to protect the red cell against oxidative stress. It deserves special mention because of the potential for development of acute and severe hemolytic episode in conditions when the erythrocytes are challenged by oxidative stress like medications and/or infections. Hemolysis has been clearly associated with exposure to certain drugs like Primaquine, Dapsone, certain antibiotics, analgesics and food like fava beans.
The severity of hemolysis depends on the variant type and extent of enzyme deficiency. G6PD can be classified into 4 grades of severity depending on residual enzyme activity [9]. As functional assessment of enzymatic activity was not done, severity is not commented upon with certainty. In general, most hemolytic episodes are mild with complete remission once the medication is stopped [5]. Although occasionally it is associated with persistent hemolytic anemia and mild jaundice, most patients maintain a normal hemoglobin level. There will usually be no abnormality noted on routine laboratory screening. There is no known treatment for the disorder other than to avoid the inciting agent [4,5].
Diagnostic approach for Unconjugated Hyperbilirubinemia
A diagnostic algorithm is presented in Fig. 1 for evaluation of unconjugated hyperbilirubinemia in an adult.
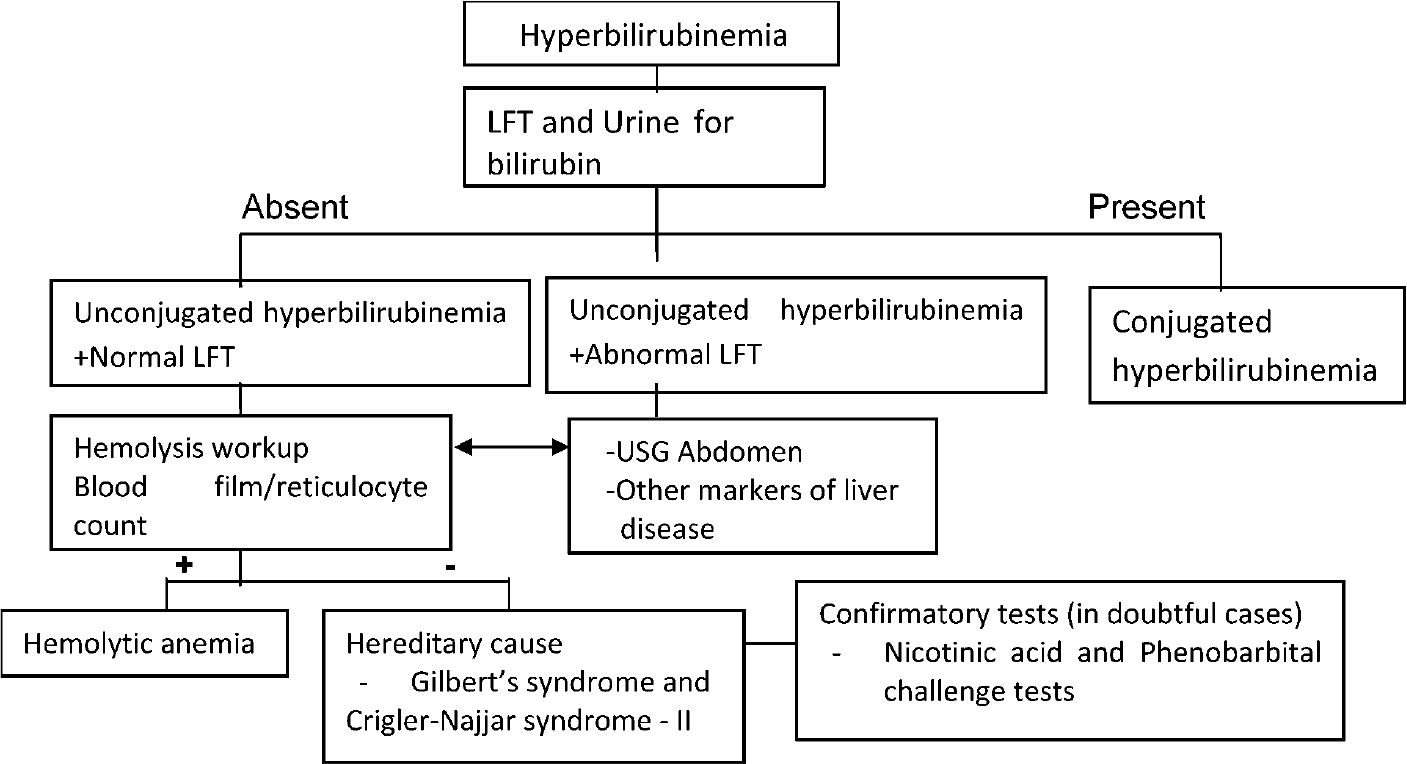
- Algorithm for evaluation of unconjugated hyperbilirubinemia
Aeromedical Concerns
Gilbert’s syndrome being a benign disorder will not pose any serious health risk, if precipitating factors are taken care of. There is neither a risk of sudden incapacitation in flight nor is any likelihood of pilot’s performance getting affected in long term. International Civil Aviation Organisation (ICAO) manual of civil aviation medicine [6] is silent on aeromedical disposition of pilots with this disability. Joint Aviation Authority (JAA) recommend certification for this condition without any restrictions [7]. Our patient was followed-up for 2 years in restricted flying category to conclusively rule out other causes before declaring him 'Fit Class-I Medical Assessment'. In view of the above, unrestricted flying category appears justified for civil pilots for cases of Gilbert’s disease, if other serious causes have been excluded beyond any doubt.
G6PD deficiency exhibit great clinical variability depending on the variant, extent of deficiency and compliance of patients in avoiding precipitant factors. It would not be efficacious to establish a rigid policy to apply to all cases. Each case will have to be judged individually, taking into consideration the severity, patient’s hemoglobin level and past history of hemolytic episodes. ICAO doesn’t bar certification, provided the hemoglobin level is stable and the pilot is well aware of what foods and medicine should be avoided [6]. He should disclose his disability whenever visiting physician before taking any drugs.
Question arises, what are the aeromedical implications in military aircrew, fighter aircrew in particular, with such disabilities. IAP 4303,3rd ed does not give clear-cut guidelines for such disabilities. US Tri-service waiver guide permits unrestricted flying in cases of isolated Gilbert’s syndrome, provided the pilot is totally asymptomatic [8]. Given the benign nature of the disease, it appears appropriate to give unrestricted flying category to military aircrew after thorough workup to rule out other serious disorders.
As far as G6PD deficiency is concerned, the issue is hemolytic episodes. Even milder episodes can have greater adverse effects on aircrew in terms of stresses of fighter flying. Literature survey did not reveal that how G6PD deficiency state would behave under aviation stresses like hypoxia and acceleration. But it can be hypothesised that due to destruction of red blood cells, oxygen carrying capacity of blood will be reduced which may lead to decreased tolerance to these stresses. Initially aircrew should be observed in non flying category for 12 to 24 weeks to ensure compliance with imposed restrictions. Asymptomatic cases without any signs of hemolysis can be allowed unrestricted flying, if there is reasonable assurance that precipitants will be avoided. In more serious forms, change of stream should be considered with multicrew cockpit restrictions.
The key to certification of aviators suffering from hyperbilirubinemia is to base policy on symptoms, cause, severity and compliance of patient with restrictions imposed. Need for regular follow-up, irrespective of the cause in this group of civil and military aircrew cannot be overlooked as they will always be at higher risk for developing hepatic abnormalities, which if ignored will lead to serious consequences. 3 to 6 monthly follow up with LFT reports will be required to rule out any development of hepatic dysfunction.
Conclusion
This case report is intended to create awareness about unconjugated hyperbilirubinemia, its diagnostic workup and aeromedical concerns. Though disabilities discussed here are essentially benign in nature, affected aircrew should be under strict observation, with periodic monitoring of markers of the disease. He will have to be adequately briefed, reminded time and again to avoid precipitants and aggravating factors. Flying category will depend upon clinical circumstances.
Conflict of interest: None
References
- Bilirubin Metabolism and hyperbilirubinemias In: Eugene B, ed. Harrison’s Principles of Internal Medicine (16th ed). 2005. p. :1928-30.
- [Google Scholar]
- Liver and biliary tract disease In Davidson’s principle and practice of medicine (20th Ed). 2007. p. :944-6.
- [Google Scholar]
- Clinical experience with isolated hyperbilirubinemia. Scand J Gastroenterol. 1989;24:617-22.
- [Google Scholar]
- Hemolytic anemias and acute blood loss. In Harrison’s principles of internal medicine Vol 681. (16th Ed). 2005.
- [Google Scholar]
- Glucose-6-Phosphate Dehydrogenase Deficiency. In: In Clinical Aviation Medicine (4th Ed). New York: Professional Publishing Group; 2006. p. :35-6.
- [Google Scholar]
- International Civil Aviation Organization. Haematology:III 5-2. Available from: http://www.icao.int.icaonet/dcs/8984 Accessed Oct 15 2009
- [Google Scholar]
- 2009 The digestive system. 4:1-6. Available from from: http://www.jaat.eu/licensing/manual_civil_aviation.html Accessed Oct 15, 2009
- [Google Scholar]
- In:Manual of Clinical Hematology. In: 4th Ed. Lippincott Williams & Wilkins; 2001. p. :101-2.
- [Google Scholar]






