Translate this page into:
Sympatho-adreno-cortical activity during head up tilt, lower body negative pressure & + Gz acceleration
Abstract
Three laboratory procedures are used to impose a haemodynamic stress in aerospace physiology, namely, head up tilt (HUT), Lower body negative pressure (LBNP) and acceleration (+Gz) stress in a centrifuge. It was felt that exposure to these stresses would induce a baroreceptors mediated reflex increase in heart rate (HR), and endocrine responses, albeit the quantum of these changes may be different. In this study, we compared the changes in urinary levels of Catecholamine (CA), Epinephrine (E), Norepinephrine (NE), Vanillyl Mandelic Acid (VMA) and 17-oxygenic steroids (17-OGS) in comparison to HR during HUT, LBNP and a simulated aerial combat manoeuvre (SACM) by subjecting healthy male volunteers to 20 minutes of 70° HUT without foot support (n=12), 25 minutes of LBNP in consecutive steps of 5 min at -20, - 30, - 40, - 50 and -60 mmHg (n=10) and + 4-8Gz SACM with anti-G suit (AGS) and anti-G straining manoeuvre (AGSM) until volitional fatigue (n=18). Changes in HR and urinary CA, E, NE, VMA and 17-OGS during these exposures were measured and compared. Increase in HR during HUT (25.4 + 8.7 bpm) and LBNP (25.2 ± 14.6bpm) were about the same while exposure to SACM resulted in a much higher increase (86.9 ± 32.1 bpm). However, the increase in CA. NE, NE/E ratio and 17-OGS was similar during SACM and HUT, VMA was significantly higher during SACM than during HUT. No such increase was noted during LBNP. Though LBNP and HUT showed a similar cardiovascular response, they differed significantly in their endocrine response. In contrast HUT and SACM, which had a markedly different HR response, had similar endocrine responses. This may be due to the difference in hydrostatic pressure gradients above the heart, which is not there during LBNP. A higher VMA excretion during SACM reflects enhanced CA synthesis due to associated fatigue while performing AGSM.
Keywords
HUT
LBNP
SACM
CA
E
NE
VMA
17-OGS
HR
SBP
DBP
High + Gz stress is an important reality of modern day flying. As the capabilities of aircraft are increasing, there is a need to simulate + Gz forces in the laboratory for research and training purposes. Usually this is done using a human centrifuge. The human centrifuge is, however, a very expensive tool. Researchers have been trying to find low cost surrogates for the human centrifuge, which could apply similar stress on the human body [1, 2, 3]. Head up. tilt (HUT) applies a hydrostatic pressure gradient of + 0.94 Gz, thus reducing the blood pressure at brain level by about 25 mmHg and increasing that at the legs by about 80 mmHg. This results in a venous pooling with transfer of about 600 ml of blood to the leg veins [4, 5]. A more exaggerated hydrostatic pressure is seen during exposure to +Gz. The expected pooling is about 12-50 ml/G in the first 25s followed by 60 ml/G in the next five min [6]. Lower body negative pressure (LBNP) done in supine position does not apply such a hydrostatic pressure gradient. The application of LBNP, however, causes elevation of vascular trans-mural pressure that results in pooling of blood in capacitance vessels and translocation of plasma filtrate into extra vascular spaces. It has been established that the amount of pooling depends upon the level of LBNP used. With -30 to - 50 mmHg, the pooling is of the order of 600 ml, which is equivalent to that seen during 70° HUT [7, 8,9]. LBNP of the order of - 40 mmHg has been equated to a +Gz stress of+2 Gz [7, 9].
All the three stressors mentioned above result in central hypovolaemia. This in turn triggers various physiological responses, namely, arterial baroreceptor reflex and peripheral vasoconstriction. The degree of such response depends upon the degree of stress and the adequacy of vagus, sympathetic nervous system (SNS) and adrenal gland function. It has been demonstrated, that the increased excretion of catecholamine (CA), epinephrine (E), nor-epinephrine (NE), Vanillyl Mandelic acid (VMA) and 17 oxygenic steroids (17 OGS) may quantify the magnitude of change in the activity of the sympatho-adreno-medullary axis and adrenal cortex [1, 10, 13]. These urinary hormones, when converted into timed excretion rates provide an integrated measure of stress and constitute a sensitive index for stress assessment [13, 14]. The various stress hormones indicate different type of stresses. We thus feel that comparing urinary stress hormone levels between the various stresses would give us an understanding of how well the HUT and LBNP could act as a surrogate for research and training of + Gz stress.
In the present study, we investigated changes in urinary CA, E, NE, VMA and 17-OGS in relation to baroreceptor mediated reflex increase in heart rate (HR) during exposure to HUT, LBNP and simulated air combat maneuvers (SACM) in the human centrifuge.
Material and Methods
The study was conducted after due approval by the Human Experimentation Committee of the Institute of Aerospace Medicine. Different volunteers (Table - 1) were subjected to HUT (n=12), LBNP (n=10) and SACM (n=18) stresses after due and informed consent. All subjects reported to the laboratory in the post absorptive state. They were placed in supine position for a period of 30 min to reach a resting state. Baseline pulse and blood pressure (BP) were recorded at the end of this period.
| Stress | Height (cm) | Weight (kg) | Age (years) |
|---|---|---|---|
| HIT | 166.9 ±5.62 | 65.7 ± 6.2 | 35.3 ± 3.2 |
| LBNP | 170.5 ±6.31 | 63.5 ± 3.2 | 29.2 ± 2.4 |
| SACM | 176.5 ±5.3 | 68.3 ± 6.3 | 25 ± 2.1 |
HUT 12 healthy male volunteers (Table - 1) were subjected to 70° HUT using a tilt table with a well-padded bicycle seat for support. The subject was tilted, within 5 s to 70° HUT and maintained in this position for 20 min. No foot support was provided.
HR »as recorded by counting the pulse rate manually and BP was recorded using a mercury yfryj—yimetiT These measurements were lnir-*~ r'TT- 2 mm during orthostasis. Recovery of OKfc«»?5«r_ir parameters were recorded 5 min jiHet im z. ~.
LBNP 10 healthy male volunteers (Table - 1) pBTacxiUiC :n this study. The LBNP apparatus in ■ ae e L\M -a as used. This apparatus has been jfcscnrei s. detail elsewhere [15]. Subjects were aw":^r-^ -A-.th the LBNP protocol one day prior ts ix experiment by subjecting them to a anmusnzsT-on protocol of LBNP, to - 30 mmHg. The Tss rrccrccv consisted of step-wise increase in LBV?. — increments of -10 mmHg, starting at -20 Fill “I Physiological parameters were recorded at ine n: c:” a stabilization period of 5 min. The pr«sac»k>r.-:al parameters recorded were HR, systolic ricoi pressure (SBP) and diastolic blood pressure DB? The experiment was terminated at -60mmHg, -•' ix subject reported discomfort or if pre-rocccal 5>Tnptoms developed. None of the rocrrnents had to be terminated due to subjective rsc-ocnfo-n or pre-syncopal symptoms.
SACM Eighteen healthy male fighter pilots (Table -". > »-.ih flying experience of 480-1300 h, belonging 😮 SfiG 21 and MiG -27 aircraft participated in the irjdy One pilot had flown 80 h in the Mirage 2000 and r*o had 10-15 h in the MIG-29 high performance aircraft. These aircrew were undergoing the Advanced Fighter Aeromedical Indoctrination Course (AFAIC) that has been described in detail by Gomez et al [16]. The subjects were tested in the microprocessor controlled human centrifuge with an arm length of 7.5 m and an effective radius of 5 m. The subjects were instrumented with a standard 3 lead
ECG and a Doppler probe to detect superficial temporal artery blood flow. They were seated on an upright (13° tilt-back) seat, with a standard 5 - bladder cutaway type anti - G suit. They were strapped to the seat using a standard four - point harness, adjustable headrest, adjustable rudder pedals. The SACM profile consisted of multiple peaks of 4 G-15 s/8 G-lOs. The end-point was volitional fatigue, peripheral light loss or G-LOC. SACM tolerance was taken as the total duration in seconds from the start of the run till its termination.
Collection of Urine Samples Timed and measured urine samples were collected before and after the experiment using “double voiding” technique. The sample pH was adjusted to 3 using HCI following which it was refrigerated.
Urinary CA, E and NE were analysed using fluorometric techniques and VMA and 17-OGS by spectrophotometry [12]. The concentration of each analysate was multiplied by volume divided by time and expressed as excretion rate [12, 14].
Statistical Analysis Paired Student's t-test was used to compare pre and post - experimental changes in urinary biochemical and physiological variables within and between various groups. The relationship between HR and CA, E, NE, NE/E ratio, VMA and 17-OGS during these three experimental conditions was established using Pearson's Product moment correlation coefficient test. Significance was accepted at 0.05 levels. Values were expressed as Means ± SD.
Results
Cardiovascular Changes The heart rate changed significantly during all three stresses. The mean heart rates before and during all three stresses are mentioned in Fig - 1. The difference in HR between LBNP and HUT was not significant. SACM was significantly different, in that, the increase in heart rate was 3.4 times greater than in either HUT or LBNP. Despite similar changes in HR during HUT and LBNP, the BP changes were significantly different. While HUT showed a rise in both SBP and DBP. LBNP showed a fall in SBP and a slight but significant rise in DBP. BP values could not be recorded inside the gondola during the SACM run due to logistic problems. Post SACM values were higher for both SBP and DBP (Table - 2 & 3).
| Stress | Pre Exposure | During Exposure | Post Exposure | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| HUT | 117 | 4.4 | 126 | 2.8 | 120 | 2.4 |
| LBNP | 117.9 | 2.09 | 112.2 | 2.66 | 124 | 26 |
| SACM | 114.0 | 1.4 | ND | ND | 122 | 1.87 |
ND = Not Determined
| Stress | Pre Exposure | During Exposure | Post Exposure | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| HIT | 77 | 1.9 | 96 | 2.5 | 82 | 2.3 |
| LBNP | 71.7 | 1.83 | 80.1 | 2.28 | 75 | 1.0 |
| SACM | 70.3 | 1.7 | ND | ND | 78.2 | 1.8 |
ND = Not Determined

- Indicates changes in HR during HUT, LBNP and Gz. Changes are significant to the pre exposure levels (P<0.001).
Urinary Hormonal Changes The changes in urinary hormone levels are reflected in Fig-2 & 3. Urinary hormones also behaved differently for HUT and LBNP. HUT showed significant increases in CA, NE, NE/E ratio and 17-OGS. Values of E and VMA did not change significantly. In sharp contrast. LBNP did not result in any change in any of the variables, except for a significant reduction in 17-OGS. Fig - 2 & 3 indicate that the changes in urinary hormones following SACM were similar to those following HUT, though SACM resulted in a significant increase in VMA unlike HUT. There was a strong correlation between HR and NE/E ratio for HUT and SACM (r=0.94 and 0.75 respectively) The correlation between HR and NE/ E ratio for LBNP was positive but less marked (r= 0.64).
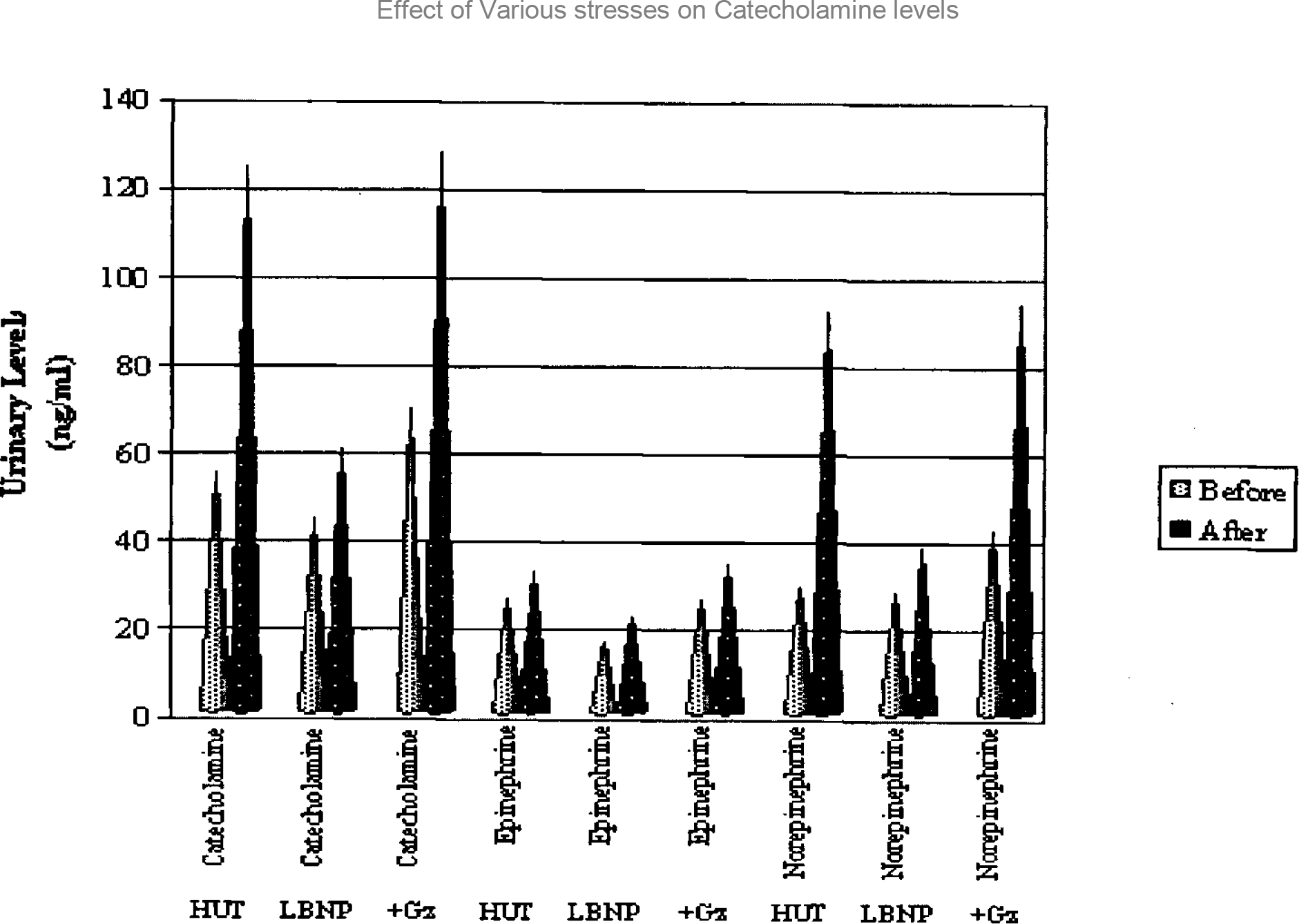
- Shows the effect of HUT, LBNP and SACM on urinary levels of CA, E and NE. Changes in E are insignificant in all stresses. Changes in CA and NE are significant for HUT and SACM only (p<0.05).
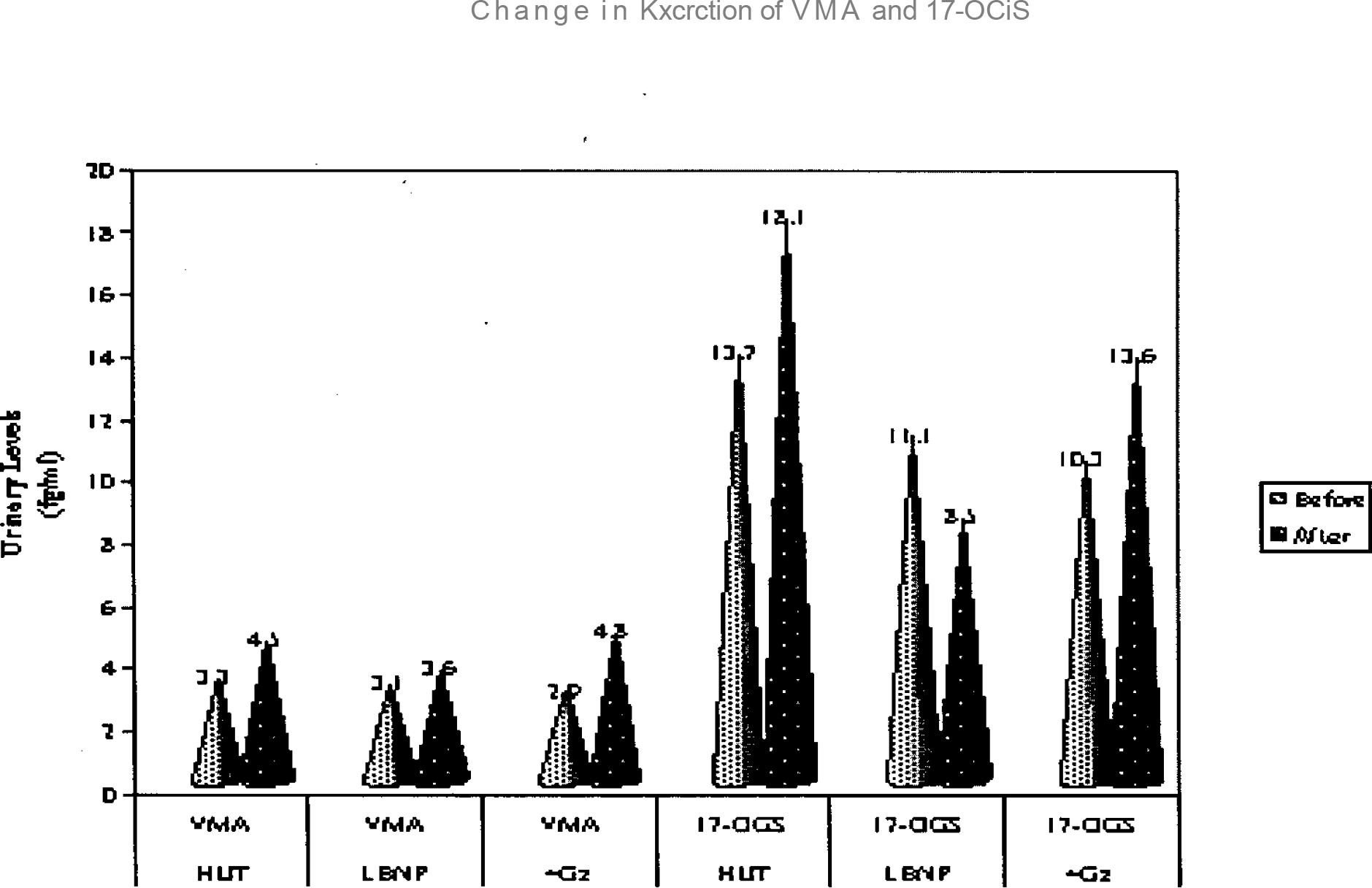
- Shows the effect of exposure to HUT, LBNP and SACM on urinary levels of VMA and 17-OGS. Changes are significant 17-OGS during all three stresses (p<0.05) Change in VMA is also significant post- SACM (p<0.05).
Discussion
To understand these results it is important to understand the significance of the above-mentioned test. All the parameters measured i.e., E, NE, NE/E ratio, CA, VMA and 17-OGS are indicative of stress. However, different hormones represent responses to different types of stress [6,18,19]. E secreted from the adrenal gland is more indicative of psychological stress than the other hormones [18]. NE on the other hand is secreted from the sympathetic nerve endings and is more indicative of physiological (haemodynamic) stress. Urinary levels of CA and VMA are both indicative of circulating levels of total catecholamine. Thus urinary CA and VMA levels demonstrate the total amount of stress that the individual is undergoing. Similarly, 17-OGS levels are indicative of the total adrenal cortical stimulation and give an idea of the total stress faced rather than whether the stress is physiological or psychological [18]. We feel that measuring urinary levels of these various hormones can give us a fair idea of the relative stress levels during HUT, LBNP and SACM. This would indicate the appropriateness of HUT and LBNP when used to simulate +Gz.
It is well known that exposure to HUT, LBNP and + Gz stress causes venous pooling in the foot ward direction temporarily reducing venous return and consequently cardiac output and arterial blood pressure. Stimulation of baroreceptor results in decreased parasympathetic inhibition of the heart and increases HR. Sympathetic stimulation of resistance and capacitance vessels further increases HR. In our study, the HR responses of HUT and LBNP were similar to each other and to those reported by other authors [5, 20]. They were, however, significantly different from SACM. AHR during SACM was 3.4 fold than that during HUT or LBNP. Does this mean that the two stresses are similar and radically different from +Gz? One would be led to believe so from the HR responses alone. However LBNP and HUT have significantly different BP responses. The lack of BP readings during SACM seriously limits the importance of as measurement.
HUT resulted in rise in NE, CA, NE/E ratio ar>d 1 “-OGS. The increase in CA, NE and NE/E rano »as almost three-fold. This indicates a significant haemodynamic stress. These results are similar to these reported by various authors in the paa [4. 5. 7. 8. 12, 20, 21]. Iwase et. al. [20] have ■ demonstrated a significant linear correlation between the sine of the angle of tilt and burst rate of rrnscle sympathetic nerve activity in normal subjects.
The response of these hormones to LBNP has. however, been variously reported by different ichors. Abboud [10] found no change in plasma CA associated with LBNP of -20 to -40 mmHg srplied t°r 20 min. Increase in renin, aldosterone and Cortisol have been reported during LBNP [7, *\ Suvorov and Beleda [9] have tried to divide subjects on the basis of LBNP tolerance and CA response, and found a positive correlation. To test ±is hypothesis, Baisch et. al. [7] measured CA and '. “OHCS in blood and urine and got inconsistent results. In our study, these hormones showed a rising trend, positively correlated with the HR, but ix change is insignificant. The LBNP levels of -60 mmHg to which our subjects were subjected is known to produce a pooling similar to that seen during 70° HUT. Why then, is the hormonal response lacking? LBNP does not provide a hydrostatic gradient between the carotid and aortic baroreceptors, unlike HUT. It would thus appear mat this gradient is important in bringing about the hormonal changes that accompany orthostatic stress.
+Gz on the other hand, imposes a much greater stress on the individual, which is a composite of psychological and physiological stresses [13, 22]. One is the psychological stress of centrifuge ride. This stress is known to reduce with successive exposures [13]. Since the pilots underwent SACM towards the end of the AFAIC, the psychological stress of Gz exposure was expected to have stabilized. This was reflected in the stable E levels pre and post centrifugation and the relatively high NE/E ratio. The other stress is haemodynamic. The haemodynamic stress was reflected in the increase in CA, NE, NE/E ratio as well as VMA and 17-OGS. Neal et al have reported a two-fold increase in VMA levels during sub-maximal exercise [23]. We found a similar increase during +4 Gz/ +8 Gz SACM to volitional fatigue. This correlated well with the rates of 157 ± 29 bpm during our study which are similar to those reported for sub-maximal exercise [23]. This also substantiates anecdotal reports from pilots that the end-point for requesting termination of the SACM was fatigue rather than +Gz stress.
To summarize, the HR responses to LBNP and HUT were similar and significantly different compared to SACM. Thus, neither of these stresses would appear to simulate +Gz stress haemodynamically. However, the stress hormone responses of HUT were very similar to those following SACM. Thus the haemodynamic stress applied by SACM appears to be effectively replicated by HUT. While this appears to be counter-intuitive, it could be explained in terms of exposure times. While an SACM run is of maximum duration of 5 min [16] the HUT lasted for 20 min, perhaps resulting in similar pooling and thus a similar haemodynamic challenge. LBNP, on the other hand, while producing a HR response similar to HUT, does not produce the same physiological stress and is thus not a close simulation of +Gz. LBNP in seated position, as recommended by Ludwig et al [1] may be a better simulation.
References
- Mediating effects of onset rate on the relationship between +Gz and LBNP tolerance and cardiovascular reflexes. Aviat Space Environ Med. 1998;69:630-8.
- [Google Scholar]
- Lower body negative pressure box for +Gz simulation in upright seated position. Aviat Space Environ Med. 1979;50:1182-4.
- [Google Scholar]
- Value of lower body negative pressure system for simulation +Gz-induced physiological strain. Aviat Space Environ Med. 1993;64:165-9.
- [Google Scholar]
- Cardiovascular and endocrine responses to head up tilt and vasopressin infusion in humans. Am J Physiol. 1986;251:335-41.
- [Google Scholar]
- Plasma nor-epinephrine, blood pressure and heart rate response to graded change in body position. Aviat Space Envicon Med. 1985;56:1166-71.
- [Google Scholar]
- Human endocrine responses to acceleration stress. Aviat Space Environ Med. 1982;53:537-40.
- [Google Scholar]
- Zero G simulation for ground based studies in human physiology with emphasis on cardiovascular and body fluid system. In : Chapter III Lower body negative pressure-A method for controlled circulation disorder. European Space Agency, 8-10, Rue-Mario-Nikis, 75738, Paris, Cedex-15 France 1982:43-78.
- [Google Scholar]
- Peripheral venous renin activity during 70° tilt and lower body negative pressure. Aerospace Med. 1972;43:713-5.
- [Google Scholar]
- Analysis of some mechanisms of man's tolerance to lower body decompression (English Abstract) Kosmicheskaia boil i med. 1972;6:56-9.
- [Google Scholar]
- Autonomic reflexes and vascular reactivity in experimental survey in man. J Clin Invest. 1970;49:298-307.
- [Google Scholar]
- Correlation of + Gz tolerance to urinary adrenaline and nor-adrenaline. Am J Physiol. 1956;18:601.
- [Google Scholar]
- Biogenic amine/metablic responses during in-flight emergencies. Aviat Space Environ Med. 1985;56:576-80.
- [Google Scholar]
- Urinary output of adrenaline, nor-adrenaline and 3-methoxy, 4-hydroxy Mandelic acid following centrifugation and anticipation of centrifugation. J Clin Invest. 1960;39:1533-8.
- [Google Scholar]
- Catecholamine excretion in T-37 flight training. Aviat Space Environ Med. 1977;48:405-8.
- [Google Scholar]
- Nystagmus induced by lower body suction. Procedings of the 42nd ICASM. Ind J Aerospace Med. 1994;38:57-60.
- [Google Scholar]
- Centrifuge training for fighter aircrew: The Indian experience. Procedings of the 42nd ICASM. Ind J Aerospace Med. 1994;38:84-8.
- [Google Scholar]
- Practical Clinical biochemistry - hormones, vitamins drugs and poisons Vol II. London: The White Friars Press Ltd; 1981. p. :67, 201-2
- [Google Scholar]
- Metabolic adrenergic changes during sub-maximal exercise and in recovery period in man. J Appl Physio. 1979;47:301-5.
- [Google Scholar]
- Effects of graded head up tilting on muscle sympathetic avtivity in man. Physiologist. 1987;30(Suppl):62-3.
- [Google Scholar]
- The effect of body posture on the urinary excretion of adrenaline and nor-adrenaline. Acta Med Scand. 1958;16(Suppl):336-59.
- [Google Scholar]
- "Salivary Cortisol". Good indicator for acceleration stress. Aviat Space Environ Med. 1987;58:573-5.
- [Google Scholar]
- 3-methoxy, 4-hydroxy Mandelic acid excretion during physical exercise. J Applied Physiol. 1968;24:619-21.
- [Google Scholar]






