Translate this page into:
Superotemporal Quadrantanopia and Central Serous Chorio-Retinopathy: Aeromedical Disposition
Abstract
Background:
Optimal vision is crucial in aviation related tasks. In aircrew, the diagnostic work up for rare visual disabilities affecting vision has to be exhaustive. The need for using newer diagnostic modalities cannot be disregarded, when there is a massive implication on the correctness of diagnosis. Vision corrected with lenses can be accepted safely and effectively in aviation. However, there is a need to understand the future course of a particular visual defect for appropriate disposition.
Case Summary:
38 years old fighter aircrew of IAF with a flying experience of approximately 1350 hours was detected to have visual field defect- Right Supero-temporal quadrantanopia (B/E) while undergoing review for Ureteric Colic (Lt) in Feb 14. He was also found to have optic disc features suggestive of Glaucoma. In subsequent reviews the aircrew maintained normal visual acuity while in non-flying category. Later his diagnosis was changed from Rt Supero-temporal Quadrantanopia (B/E) to Central Scotoma (B/E)-Old CSCR. He has been observed adequately in non-flying medical category for a period exceeding one year and gradually upgraded to restricted flying category for another one year period of observation before considering him for awarding full flying category.
Discussion:
The guidelines for aeromedical disposition in Indian Air Force, IAP 4303 (4th Ed-Revised) is silent about the disposition of a case of CSCR. In case of any field loss detected in automated perimetry, aircrew is unfit for flying duties in fighter stream as per the same guidelines. The fact and figures about the visual conditions have been brought out in this paper after extensive literature review. The international consideration on various waiver and aeromedical certification also has been discussed for future reference on such cases.
Aeromedical disposition:
All possible associated conditions need to be diagnostically excluded; once satisfied, the benefit of doubt should definitely go to the aircrew after the recovery is complete. Once reflighted, a close and regular follow up to assess the disease progress is essential in such cases. If the actual aetiology is unknown, it becomes a challenge to predict the disease prognosis as well as chance of recurrence and the possibility of sudden incapacitation, thus the aeromedical decision.
Keywords
Quadrantanopia
Field loss
Vision
Reflighting
Introduction
Human civilization can be aptly said to be centred around vision. Good vision is an essential requirement to perform difficult and complex tasks, especially in aerospace scenario. Though the importance of other sensory systems which a pilot would require to perform complex tasks cannot be undermined, vision is by far the most important sensory modality sub-serving spatial orientation and is utilized to its fullest capacity during flying. The need of ensuring optimal vision is crucial in an aircrew suffering or after recovery from any visual disabilities. Therefore, the diagnostic work up for rare visual disabilities affecting vision has to be exhaustive. The need for using newer diagnostic modalities cannot be disregarded, when there is a massive implication on the correctness of diagnosis. Vision corrected with lenses can be accepted safely and effectively in aviation. However, there is a need to understand the future course of a particular visual defect for appropriate disposition. Else, the aerospace safety will be jeopardised. In this paper, the aeromedical decision making for a case of Supero-temporal Quadrantanopia transforming to Central Serous Chorio-retinopathy has been discussed.
Case Summary
38 years old fighter aircrew of IAF with a flying experience of approximately 1350 hours was detected to have visual field defect- Right Supero-temporal quadrantanopia (B/E) while undergoing review for Ureteric Colic (Lt) in Feb 14. He was also found to have optic disc features suggestive of Glaucoma.
On carrying out a thorough glaucoma diagnostic work up, he was found to have normal IOP (Intra Ocular Pressure), normal corneal thickness, normal OCT (Optical Coherence Tomography) and RNFL (Retinal Nerve Fibre Layer) thickness. Although the aircrew was completely asymptomatic, during perimetry the visual field defect which was documented initially was reproducible in all the occasion of subsequent reviews during the period of observation in non-flying category. Thereafter, the quadrantanopic field defect was reassessed as a central scotoma which was persistent throughout the further period of observation. The officer was maintaining normal visual acuity (6/6; both eye) with corrective glasses along with normal colour perception and contrast sensitivity. On review by the Vitreo-Retinal Surgeon, it was opined that the visual field defect (Central Scotoma) is probably a sequel of old healed CSCR (Central Serous Chorioretinopathy).
Subsequently, his diagnosis was changed from Rt Supero-temporal Quadrantanopia (B/E) to Central Scotoma (BE)-Old CSCR. He has been observed adequately in non-flying medical category for a period exceeding one year. He was gradually upgraded to temporary restricted flying category and was further observed for one more year before awarding him final disposition.
Based on the above mentioned status, as there were no further progression of the disease and deterioration of the vision, he was finally awarded A2 (P) status, recommended unfit for Fighter flying and fit for Transport/ Heptr only in accordance with IAP 4303 (4th Edition) [1].
Discussion
Superotemporal Quadrantanopia
Quadrantanopia, Quadrantanopsia or Quadrant anopia refers to an anopia affecting a quarter of the field of vision. It can be associated with a lesion of an optic radiation, temporal and parietal lobes. It is most commonly associated with lesions in the occipital lobe. An interesting aspect of quadrantanopia is that there exists a distinct and sharp border between the intact and damaged visual fields, due to an anatomical separation of the quadrants of the visual field. The prospects of recovering vision in the affected field are bleak. Occasionally, patients spontaneously recover vision in the affected field within the first three months [2].

- Rt Superotemporal Quadrantanopia (visual field loss)
There was no radiological work up to rule out possible causes. Extensive literature search does not reveal any useful guideline for aeromedical disposition of such cases. However, available guidelines do comment on the issues of aeromedical interest in an aircrew with visual field loss. Furthermore, the final diagnosis of the aircrew in this study was revised to Central Scotoma-Old CSCR (ambiguous).
Central Serous Chorioretinopathy (CSCR)
CSCR is a relatively common cause of visual impairment worldwide, and is characterized by the accumulation of subretinal fluid in the macula [3,4]. The disease classically affects men between the ages typically of 20 and 50. Patients can present with blurred or dim vision, relative central scotoma (our case), metamorphopsia, dyschromatopsia and micropsia [5,6] or the process may remain silent. CSCR is a major cause of vision threat among middle-aged male individuals. Most acute CSCR cases resolve spontaneously within 2-3 months. Multimodal imaging led to the description of a wide range of CSCR manifestations, and highlighted the contribution of the choroid and pigment epithelium in CSCR pathogenesis. However, the exact molecular mechanisms of CSCR have remained uncertain [7].
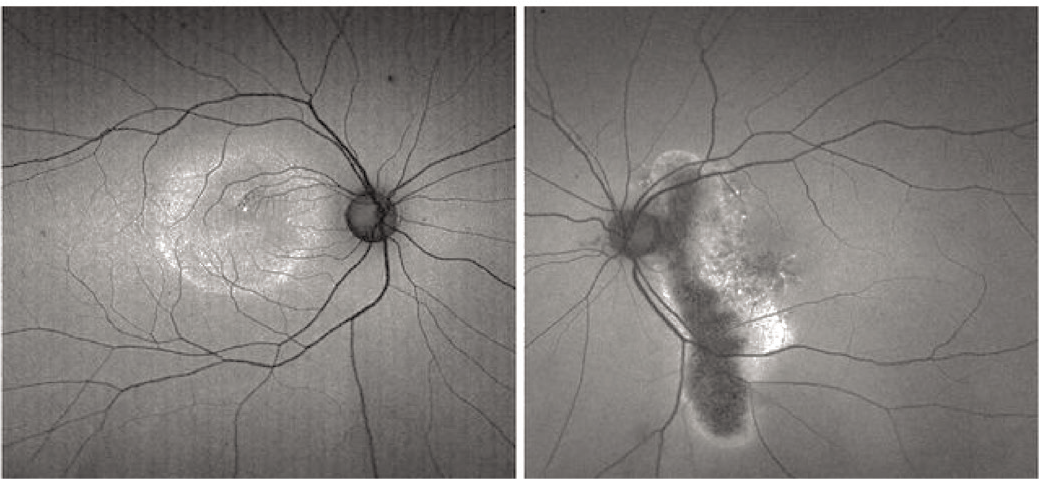
- Acute CSCR with visual field loss
Aeromedical concerns
This particular aircrew was initially diagnosed as a case of Right Superotemporal Quadrantanopia and after thorough investigation and observation was re-diagnosed as Central Scotoma (B/E) that too as Sequelae of CSCR. Therefore, aeromedical disposition should be based on the potential of any physiological or physical limitation occurring in flight or any interaction with the aviation stressors.
Supero-temporal Quadrantanopia transforming to Central Scotoma is rare. The later diagnosis was made based on assumption i.e. as a sequalae of Central serous Chorioretinopathy (CSR). CSR can adversely impact visual function with symptoms of metamorphopsia (distortion of vision), micropsia (smaller visual images), scotomata (areas of the visual field missing or blurred), blurred vision, colour desaturation (reduced brightness of colours), Reduced contrast sensitivity or sub-standard visual acuity. A 1988 Aeromedical Consultation Service (ACS) study that examined 47 rated airmen with 55 eyes affected by CSR found that all but one of the patients was returned to flying status. 51% of airmen had recurrent episodes, 86% had better than 20/20 visual acuity after resolution of the CSR, 87% had normal colour vision and 90% had normal stereopsis [8].
The effect of the aerospace environment on active CSR is currently unknown. The presence of subretinal fluid introduces new dynamics into the eye that are not present otherwise. The effect of applying G-forces or relative hypoxia upon the pathophysiologic process of CSR is unclear. Further, sub-retinal fluid indicates active disease, which introduces the possibility of fluctuating visual acuity and could have an adverse impact on flight safety. Because of the aeromedical implications of these variables, aircrew members will not be considered for return to flight status until complete resolution of the sub-retinal fluid occurs as demonstrated by ophthalmologic exam and ancillary studies.
For an aircrew who has a history of CSR, regular follow-up care and monitoring are critical for aerospace safety and continued ocular health.
International Considerations
Most of the relevant Aeromedical Disposition guidelines do not stress upon much on Quadrantanopia but adequate information available CSCR. All the available disposal guidelines have been depicted in Table 1.
| Reference | Aeromedical Disposition |
|---|---|
| US Air Force Waiver Guide | CSR is disqualifying for aviators and requires ACS evaluation for waiver consideration. After documented resolution of the CSR by a fundus exam and if possible optical coherence tomography (OCT), a waiver may be requested. Even if the airman’s vision returns to 20/20 or is correctable to 20/20, a local eye specialist must demonstrate that the sub-retinal fluid has resolved prior to waiver request submission. Waivers may be requested with best corrected vision less than 20/20 or residual visual symptoms (metamorphopsia, color vision deficits), however, the visual acuity and visual symptoms must be stable (not improving or worsening). |
| US Navy Waiver Guide | N/A |
| JAA | The clinical course of this disease is very unpredictable. Usually visual functions are almost fully restored, leaving only a slight reduction in contrast sensitivity. An assessmentmay be considered if visual functions are restored and retinal oedema cannot be demonstrated by clinical nor by angiographic examinations. |
| AsMA | N/A |
| Clinical Aviation Medicine 4th Ed (Russel B. Rayman) | Aviators with active CSC should be restricted from flying duty. Once remission occurs usually within several months and the patient has regained normal visual acuity and depth perception, a request for a medical waiver can be granted. However, because there is a significant recurrence rate, close follow up is recommended. |
| Ernsting’s Aviation Medicine 5th Ed (David J. Rainford & David P. Gradwell) | Aviators with CSC are often unfit aircrew duties while they have significant visual disturbances. They will often opt for laser treatment of the problem rather than wait for spontaneous resolution. |
| FAA | N/A |
| Fundamentals of Aerospace Medicine 4th Ed (Jeffrey R. Davis et al) | Central serous retinopathy, plays havoc with a pilot’s stereopsis/depth perception. Fortunately, 97% of these afflicted individuals recovered and were returned to full flight status as noted in a review of USAF aviators with this condition. Older flyers may develop macular degeneration that may eventually end their flying careers because presently no effective treatment exists for this condition. |
|
Principles and Practice of Aviation Medicine (Claus Curdt Christiansen) |
This disorder, which mostly affects active men in their middle years. If the macula is involved, patients usually complain of distortion of vision or micropsia (the perception of objects as being much smaller than they actually are). In many cases, the warping of the retina leads to hyperopia. This disorder has a good prognosis and spontaneous healing is common. In some cases, the source points can be visualized with fluorography and coagulated by laser. Often, this results in a minimal decrease in function and diminished contrast sensitivity. Medical certification may be considered when there is no further evidence of leakage as shown by fluorography. Persistent serous leaks can result in unpredictable vacillations in visual acuity. |
IAP 4303 (4th Ed-Revised) position
According to IAP 4303 (4th Ed-Revised), any field loss, detected on automated perimetry shall make aircrew unfit for flying duties in fighter stream. Change of stream, if feasible, can be considered if the ocular condition remains controlled. However, IAP is silent on disposal of cases of CSCR.
Aeromedical Disposition
In accordance with the IAP 4303 and as there were no further progression of the disease, the aircrew in this case was recommended to be placed in permanent A2 category. Although, the corrected vision was normal due to Central Scotoma he was recommended unfit for Fighter flying and fit for Transport/Heptr only. In this particular case due to the incidental detection of the disease, the onset and etiopathology of CSCR could not be commented upon.
Conclusions
The prognosis of CSCR is generally excellent [9]. Whilst immediate vision loss unlike the present case may be as poor as 20/200 in the affected eye, clinically over 90% of patients regain 20/30 vision or better within 6 months. Once the fluid leak is resolved, by itself (in this case, no history of active treatment) or through treatment visual acuity should continue to improve and distortion should reduce as the eye heals. However, some visual abnormalities can remain even if visual acuity is measured at 20/20, and lasting problems include decreased night vision, reduced colour discrimination, contrast sensitivity and localized distortion caused by scarring of the sub-retinal layers [10]. Complications include subretinal neovascularization and pigment epithelial detachment [11].
One important concern is, the disease can re-occur causing progressive vision loss. There is also a chronic form, titled as Type II Central Serous Chorioretinopathy, which occurs in approximately 5% of cases. This exhibits diffuse rather than focalized abnormality of the pigment epithelium, producing a persistent subretinal fluid. Prognosis for this condition is less favourable and continued clinical consultation is advised. In this particular case there is no further progression/deterioration in visual fields since his last review by the Ophthalmologist. However, the aircrew has to be periodically reviewed to rule out any further deterioration of the condition, any recurrence of CSCR and to decide airworthiness accordingly.
Acknowledgement
The author gratefully acknowledges the assiatance extended by CO, No 1 AMU, IAF. Author also expresses heartfelt thanks to an Ophthalmologist at AFCME and the team of researchers at Institute of Aerospace Medicine for the support to bring out this article.
Disclaimer
The opinions expressed in this article are those of the author and do not reflect the official views of the Indian Society of Aerospace Medicine or Indian Air force.
References
- Section VI- Assessment of trained serving personnel (Opthalmic systen) In: IAP 4303 (4th ed (revised)). New Delhi: Air head quarters; 2016. p. :352.
- [Google Scholar]
- The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980–2002. Ophthalmology. 2008;115:169-73.
- [Google Scholar]
- Pathogenesis of disciform detachment of the neuroepithelium. Am J Ophthalmol. 1967;63:1-139.
- [Google Scholar]
- Review and Update of Central Serous Chorioretinopathy. Curr Opin Ophthalmol. 2011;22:166-73.
- [Google Scholar]
- Central Serous Chorioretinopathy: recent findings and new physiopathology hypothises. Progress in Retinal and Eye Research. 2015;48:82-118.
- [Google Scholar]
- Central serous chorioretinopathy in US Air Force Aviators: A review. Aviat Space Environ Med. 1988;59(12):1170-75.
- [Google Scholar]
- (2005). Long-term macular function in eyes with central serous chorioretinopathy. Clinical and Experimental Ophthalmology. 2008;33(4):369-72.
- [Google Scholar]
- Long-term follow-up of central serous chorioretinopathy. Bulletin de la Societebelged’ophtalmologie;. ;284:39-44.
- [Google Scholar]






