Translate this page into:
Study of Haemoglobinopathies in Aviators: Need of Haemoglobin Electrophoresis during Initial Medical Evaluation
Abstract
Background:
The inherited disorders of haemoglobin, particularly the β-thalassaemias and their interaction with haemoglobin E (HbE) and haemoglobin S (HbS) are a considerable health problem in India. Thalassaemias produce a low grade anaemia that can cause problems at altitude. Splenic enlargement and worsening of the anaemia can occur under conditions of stress. Therefore, it is important to screen and detect this condition so that the aviator may take adequate care to maintain the minimum required haemoglobin levels.
Methods:
All aircrew and candidates (both military and civil, males and females) coming to MEC, IAM for medicals over the period of 24 months (Jan 2011 -Dec 2012) were analyzed in the study. Subset of cases with normal Hb levels - the males with Hb <13.5gm% and females with Hb <12 gm% were screened by electrophoresis to detect the presence of haemoglobinopathies in individuals with borderline normal Hb levels.
Results:
A total of 3027 cases were evaluated during the 24 month period. 24 out of 56 screened cases were found positive for Haemoglobinopathies which includes 23 cases of β-thalassaemia trait and 01 case of Hb S/D/G, accounting for 42.86% of the screened cases.
Conclusion:
Incorporation of Hb electrophoresis for screening of low normal Hb during initial medical would be helpful in detecting such cases at the earliest.
Keywords
Haemoglobinopathy
Thalassaemia
Haemoglobin electrophoresis
Introduction
Anaemia reduces tissue oxygenation and can be associated with widespread organ dysfunction, particularly when haemoglobin concentration falls below 10 g/dl or hematocrit is less than 30%. Work capacity and compensations in conditions of hypoxia are also reduced in anaemia. Therefore, detection of anaemia in aviators is of great significance and needs to be investigated so as to find the cause. Nutritional anaemia should be diagnosed and appropriately corrected and prevented with correct balanced diet. Other causes like thalassaemias and haemoglobinopathies also need to be diagnosed so that the aviator may take adequate care to maintain the minimum required haemoglobin levels.
The inherited disorders of haemoglobin, particularly the β-thalassaemias and their interaction with haemoglobin E (HbE) and haemoglobin S (HbS) are a considerable health problem in India. Earlier studies have shown that the overall prevalence of β-thalassaemia in India is 3-4 % with an estimate of around 8,000 to 10,000 new births with major disease each year [1,2]. There is a variation in the prevalence of haemoglobinopathies in different regions and population groups in the country. The frequency of beta- thalassaemia trait (βTT) has variously been reported from <1% to 17% and an overall of 3.3% is stated for India (3). Studies have shown that certain communities like the Sindhis, Kutchhi Bhanushalis and Punjabis from Western and Northern India have a high prevalence of β-thalassaemia (5-15%) [4,5,6] and some population groups from the north eastern regions have a high prevalence of Hb E (5-50 %) [7,8]. A high frequency of Hb D has been reported from the North in the Punjabi population, Hb E in the eastern region of India and Hb S mainly reported from populations of tribal origin from different parts of the country [9]. There have been no large studies to see the prevalence of this in our aviators (civil and military).
In general, anemia could also result in lowered cardiovascular reserve which may not manifest during the routine day to day activities of the individual. Anemia, however, may reduce tolerance to Aviation stresses like hypoxia, G stresses and increased physical demand due to fatigue and interference with diurnal rhythm. It is important to diagnose the etiology of anemia in an aviator to differentiate the largely treatable condition of Iron deficiency anemia from the innocuous but untreatable Thalassemia Trait from one of the more sinister causes of anemia such as an abnormal hemoglobin [10]. The aeromedical concern in thalassaemias is that it produces a low grade anaemia that can cause problems at altitude. Splenic enlargement and worsening of the anaemia can occur under conditions of stress. Splenectomy results in a greater risk of overwhelming infection and of severe malaria, which can affect an aviator’s fitness to fly. Hypochromia and microcytosis due to reduced amount of haemoglobin characterize all forms of Beta thalassaemia. In heterozygote’s (Beta thalassaemia trait) this is the only abnormality seen. Most patients with thalassaemia trait have no symptoms, live normal life spans and do not require any treatment. Homozygous Beta thalassaemia or deletions in more than two of the Alfa chains are almost always severely symptomatic or anemic, and as such rarely make it into the military. Also, in these cases clinical severity precludes flying [11]. Therefore, it is important to screen and detect this condition, so that the aviator may take adequate care to maintain the minimum required haemoglobin levels.
Also, since all ethnic populations are well represented in our armed forces and civil aviation, there are many cases of thalassaemia traits and other haemoglobinopathies. Many of these cases clear the initial medicals at entry level as their haemoglobin levels are just within the minimum required standards. Subsequently, they get detected when the Hb levels fall. At present, Haemoglobin electrophoresis is not done at initial medicals if minimum criteria of haemoglobin concentration (13 gm% in male & 11.5gm% in females) are met with. Our study was carried out to study the prevalence of thalassaemias and haemoglobinopathies in aircrew and to evaluate the need for incorporation of Hb electrophoresis for screening of low normal Hb during initial medical.
Material and Methods
All aircrew (both military and civil, males and females) coming to MEC, I AM for medicals over the period of 24 months were analyzed in the study. The aircrew/candidates coming for initial issue were also taken as a separate group. Anaemia was diagnosed in males with Hb level <13gm% and in females with Hb <11.5gm%. Subset of cases with normal Hb levels - the males with Hb <13.5gm% and females with 12 gm% were screened for haemoglobinopathies by electrophoresis to see the detection of haemoglobinopathies in cases of borderline normal Hb levels. In both the groups nutritional causes were ruled out by PBS picture and RBC indices. Cases of microcytic hypochromic and normocytic anaemia were further investigated by Hb electrophoresis and serum ferritin levels to rule out iron deficiency.
The Hb electrophoresis was done on the semiautomated electrophoresis system from Alere (Helena Biosciences, Europe). Hemolysate of the sample was prepared and the Hb of the hemolysate was adjusted to a Hb between 2-3 gm/dl. Very small quantity (35 μl) of samples of hemolysate prepared from whole blood is applied to sample tray, by the applicator, which automatically applies the samples to the ready to use Alkaline Hb Gel (Agarose in a Tris/EDTA/Glycine buffer with sodium azide). The haemoglobins in the sample were separated by electrophoresis (200 volts, 30 minutes) using an alkaline buffer (pH 8.2-8.6), and were stained with Acid Blue Stain. The patterns were scanned on a scanning densitometer and the relative percent of each band was determined and interpreted as per the manufactures instructions.
The representative electrophoresis gels of normal & each type of haemoglobinopathies and their interpretation are depicted in figures as Figure 1 (A to D). All the results of Hb electrophoresis done over the last 24 months were analysed in this study.
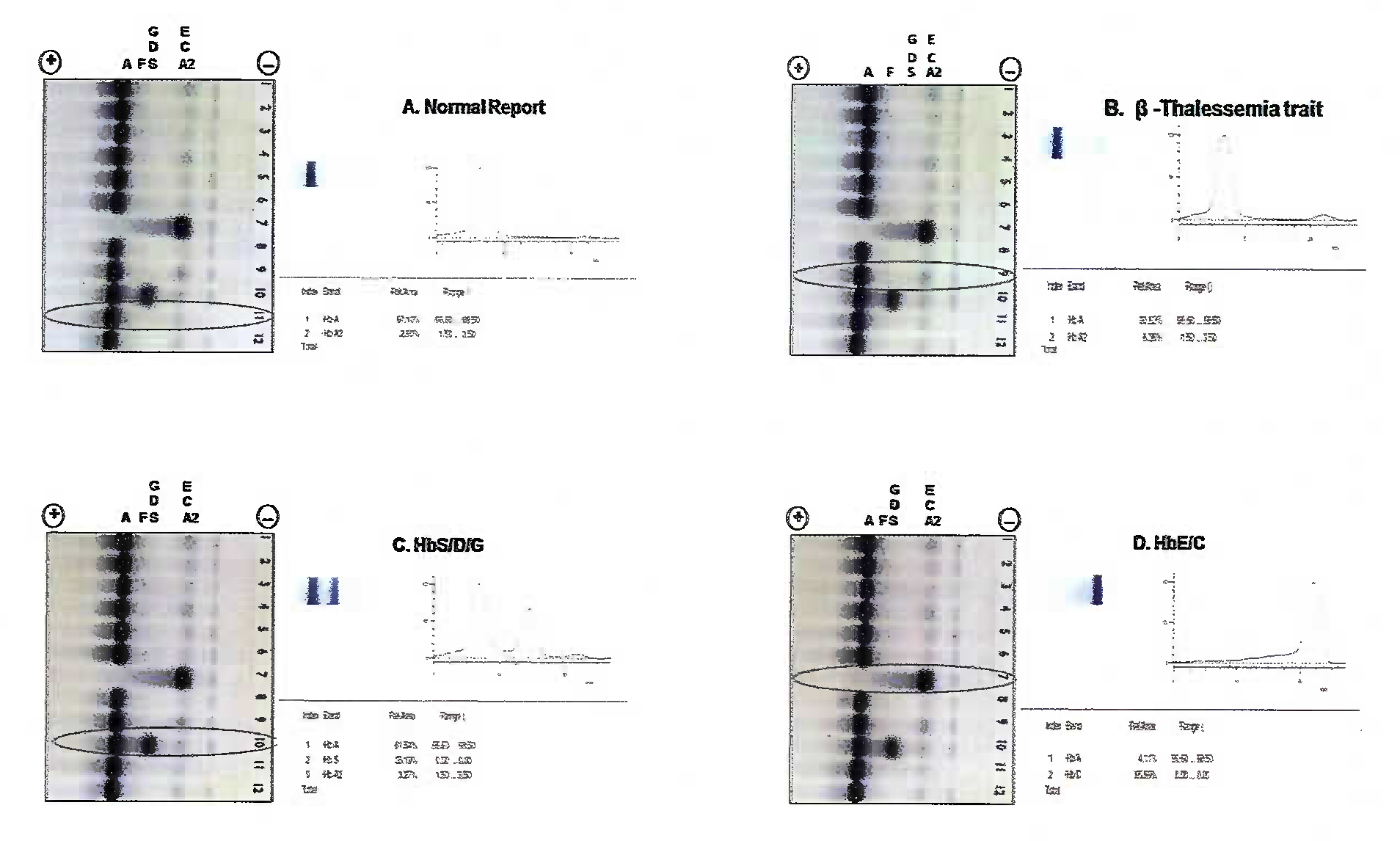
- Depicts the representative electrophoresis gels of normal & each type of haemoglobinopathies and their interpretation (A to D).
Results
A total of 3027 cases (both civil and service) were screened during the 24 month period. Of these, 56 cases fitted into our inclusion criteria of borderline Hb levels. 24 out of 56 cases were found positive for Haemoglobinopathies (Fig. 2) which includes 23 cases of β-thalassaemia trait and 01 case of Hb S/D/G.
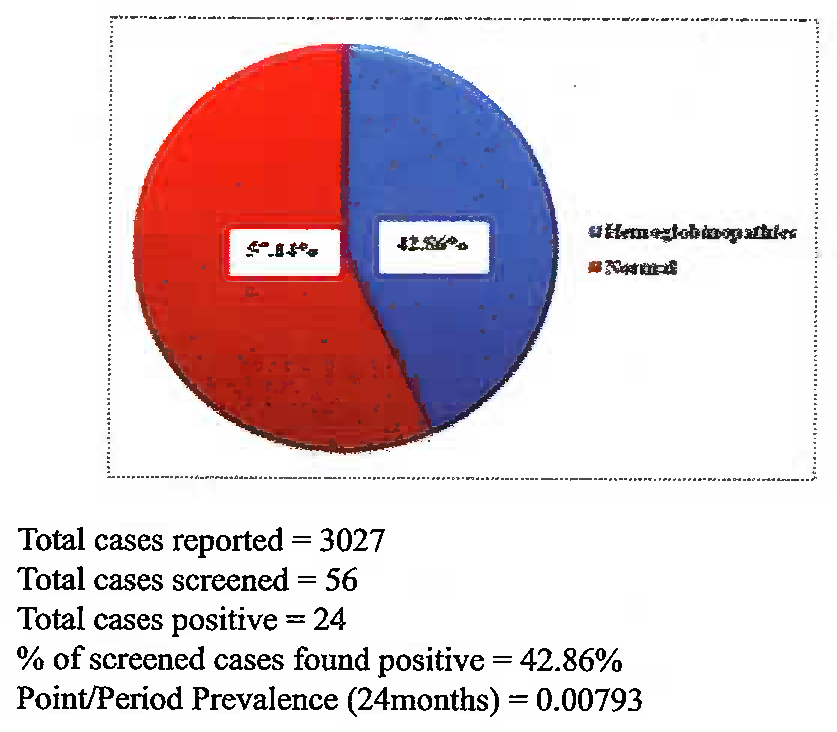
- Percentages of screened cases detected with Haemoglobinopathies (represented in blue) and Normal (represented in red)
All the 24 cases screened, the Hb was low normal - the males with Hb <13.5gm% and females with Hb<12 gm% .These cases would have otherwise cleared the medicals as the Hb was in the normal range.
An analysis of blood sample of 823 NDA cadets/direct recruitment from civil for flying branch was done. Of these 25 cases were screened and 6 were positive (Fig. 3). Of the 06 positive cases 01 case of Hb S/D/G and 05 β-thalassaemias traits were picked up even though the Hb levels were above normal values.
All the 24 cases screened, the Hb was low normal - the males with Hb <13.5gm% and females with Hb<12 gm% .These cases would have otherwise cleared the medicals as the Hb was in the normal range.
An analysis of blood sample of 823 NDA cadets/direct recruitment from civil for flying branch was done. Of these 25 cases were screened and 6 were positive (Fig. 3). Of the 06 positive cases 01 case of Hb S/D/G and 05 β-thalassaemia traits were picked up even though the Hb levels were above normal values. 164 initial civil candidate reported (male+female), none came under our inclusion criteria and so no cases were screened. However 1726 cases of civil pilots (male and female) came for medicals. In 19 cases, the Hb values were in the low normal range and were screened. 8 cases were positive for β-thalassaemia trait (Fig. 5)
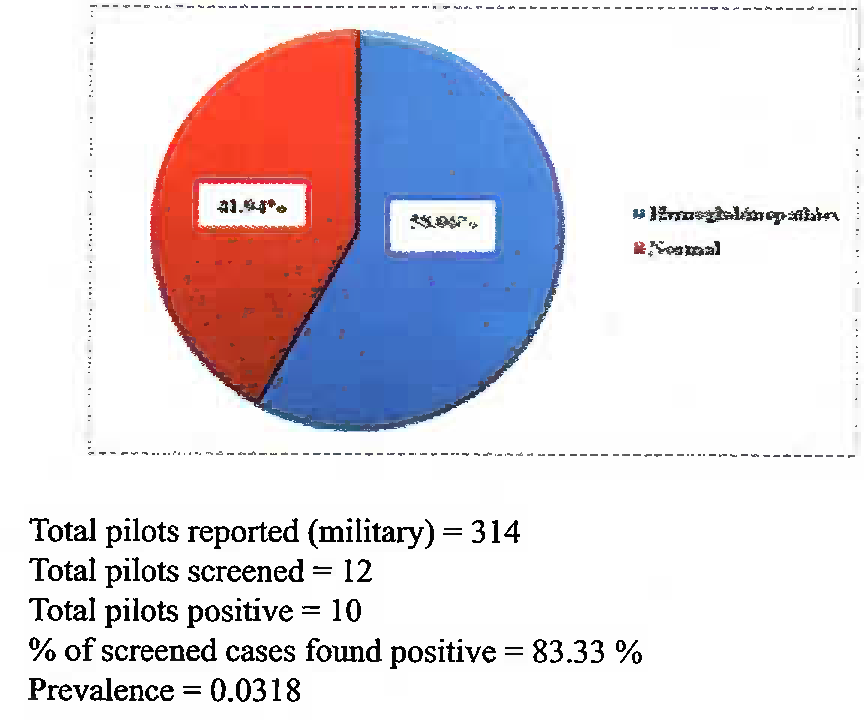
- Percentages of screened existing pilots (Military + Civil) detected with Haemoglobinopathies (represented in blue) and Normal (represented in red)
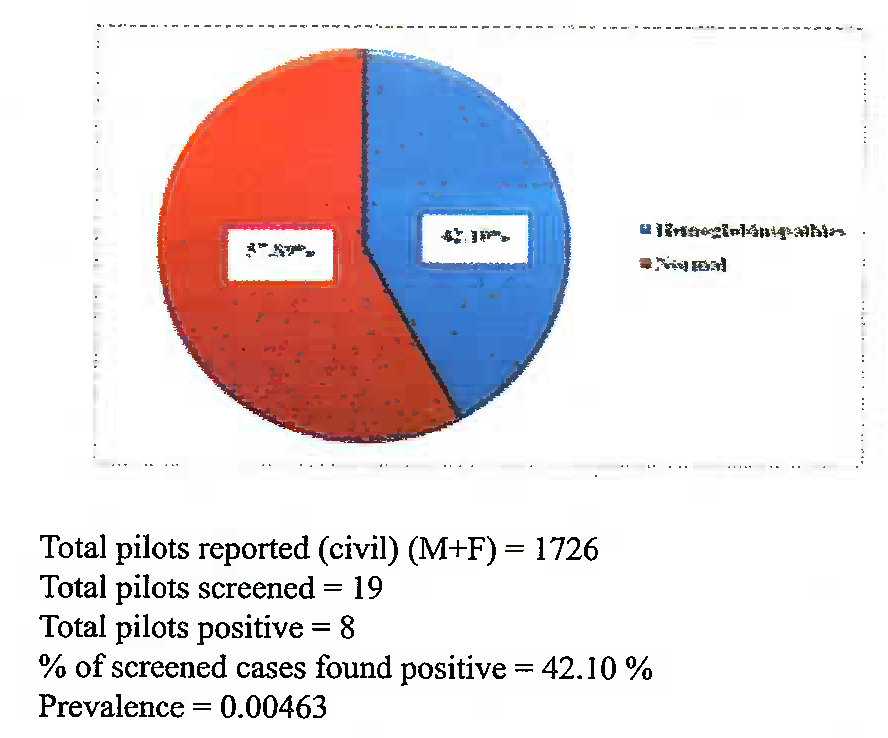
- Percentages of screened civil pilots (Male + Female) detected with Haemoglobinopathies (represented in blue) and Normal (represented in red)
Discussion
During the period of Jan 2011 to Dec 2012, a total of 3027 samples were analyzed for the estimation of haemoglobin concentration. Of these, 56 samples were found to satisfy the inclusion criteria. On conduction of Hb electrophoresis, 24 samples i.e. 42.86% of the samples screened were found to be positive for Haemoglobinopathies. The prevalence being 0.70 in the flying population (both civil and military). This is much lower than the national data of 2-3 %, mainly as only screened healthy population comes for evaluation. The most common haemogobinopathy detected was β-thalassaemia trait in 23 cases.
A total of 987 cadets reported for their initial medical evaluation, 823 of military and 164 of civil. Of them, 863 were males and 124 were females. On screening of 25 cadets with Hb levels as per the inclusion criteria, 06 were found to be positive for Haemoglobinopathies, accounting for 24% of the cases screened. This group included all those individuals detected with low normal Hb levels during the selection and the underlying Haemoglobinopathies would have remained undetected, had they not undergone Hb electrophoresis.
A total of 2040 pilots reported for their review medicals, 314 of military and 1726 of civil. Of them, 1973 were males and 67 were females. 31 pilots were screened, 18 were found to be positive for Haemoglobinopathies, accounting for 58.06% of the cases. All cases had low normal Hb levels and were screened, and of which all were detected with β-thallasemia traits.
A multicentre study conducted by Mohanty et al had revealed that the prevalence of β-thalassaemia trait was 2.78% and varied 1.48 to 3.64% in different states of India [12].
Introduction of Hb electrophoresis for screening cases of low normal Hb has resulted in detection of 24 cases (23 β-thallasemia traits & 01 Hb S/D/G) in our study. All these cases were detected in individuals with low normal Hb, who would have escaped detection under normal circumstances. The prevalence of 0.6% in the initial medicals (civil & military) and 0.88% in the existing pilots (civil & military) further substantiates the fact that the pilot population is composed of individuals healthier as compared to the general population. Absence of screening methods such as Hb electrophoresis at the initial medical stage results in many of them not detected during initial medicals and subsequently manifest later on.
In β thalassaemia trait, elevated levels of Hb A2 or F (the beta chains being decreased, the alpha chains combine with gamma and delta chains to make Hb F and A2) are usually helpful in confirming the diagnosis. A2 levels however may decrease in iron deficiency anaemia and increased levels may be seen in megaloblastic anaemia. However, in α thalassemia, the Hb electrophoresis results are usually normal; in this case, and in cases in which iron study results are also non-diagnostic, nonspecific tests may help to differentiate iron deficiency anaemia or anaemia of chronic inflammation from thalassaemia. Free erythrocyte protoporphyrin (FEP) levels are usually elevated in patients with iron deficiency or anaemia of chronic inflammation but not with thallassemia. The soluble transferrin receptors (sT fR) levels are high in patients with iron deficiency but not in those with anaemia of chronic infection or thalassaemia. Globin chain electrophoresis and DNA analysis is confirmatory [13].
As most individuals may never have any symptoms during their life span, treatment is usually not required for this benign hematological disorder. Medical waivers for pilots with minor form of the disorder can be considered favorably as long as the anaemia is minimal and the patient is symptom free [14]. These individuals have Hb levels slightly higher than the lowest cut off limits for their gender and hence are not suspected to have any underlying haemoglobinopathies. However, on exposure to high altitudes, this may lead to worsening of anaemia and make them prone for hypoxia. In addition, splenic enlargement and worsening of anaemia can occur in conditions of stress, leading to in-flight incapacitation. US Navy Aeromedical Reference and Waiver Guide also allows flying provided there are no other haemoglobinopathies present and the acceptable values for hematocrit of 40-52% in males and 37-47% in females are maintained. However, patients who have required splenectomy because of their thalassaemia are permanently disqualified from military flying [15]. However, as per Indian Air Force Publications 4303 4th edition, all candidates with evidence of hereditary haemolytic anaemias (due to red cell membrane defects or due to red cell enzyme deficiencies) and haemoglobinopathies (Sickle cell disease, Beta-thalassaemia: Major, intermedia, minor, trait, and Alpha thalassaemia etc) are to be considered unfit for service [16]. In our centre, cellulose acetate electrophoresis was done for screening. We could not distinguish between Hb S/D/G due to unavailability of citrate agar kits at our centre which would be able to distinguish the above, However, HPLC being the gold standard for confirmation of all types of haemoglobinopathies is to be used along with electrophoresis as screening in all centers where medicals are carried out.
Conclusion
The present study points towards the presence of haemoglobinopathies in aviators with even low normal levels of haemoglobin concentration. Incorporation of Hb electrophoresis for screening of low normal Hb during initial medical along with confirmation preferably by a gold standard method like HPLC would be helpful in detecting such cases at the earliest and is recommended in centres where medicals are carried out. Such screening will prevent the manifestation of many cases in later stages.
| Reported | Screened | Haemoglobino pathy type | Normal | Haemoglobino- pathy% | Normal% | Prevalence | |
|---|---|---|---|---|---|---|---|
| Total cases | 3027 | 56 | 24 (23 β-thal traits &01 Hb S/D/G) | 32 | 42.86 | 57.14 | 0.00793 |
| Total initial medicals (Civ+Mil) | 987 | 25 | 06 (05 β-thal traits & 1 Hb S/D/G) | 19 | 24 | 76 | 0.0060 |
| Military initial medicals | 823 | 25 | 06 (05 β-thal traits & 01 Hb S/D/G) | 19 | 24 | 76 | 0.0073 |
| Civil initial medicals | 164 | 0 | 0 | - | - | - | - |
| Total pilots (Civ+Mil) | 2040 | 31 | 18 (β- thal traits) | 13 | 58.06 | 41.94 | 0.0088 |
| Civil pilots | 1726 | 19 | 08 (β- thal traits) | 11 | 42.10 | 57.89 | 0.0046 |
| Military pilots | 314 | 12 | 10 (β-thal traits) | 02 | 83.33 | 16.67 | 0.0318 |
Disclaimer
The opinions expressed in this article are those of the author & do not reflect the official views of the Indian Air Force or the Indian Society of Aerospace Medicine
References
- Frequency of β-thalassaemia trait and other haemoglobinopathies in northern and western India. Indian J Hum Genet. 2010;16(l):16-25.
- [Google Scholar]
- Genetic epidemiology of the three predominant abnormal haemoglobins in India. J 7. Assoc Physicians India. 44:25-8.
- [Google Scholar]
- The problem of haemoglo-binopathics in India. Indian J haemoglobinopa-8 thies in India. Indian J Haematol 1983:1-5.
- [Google Scholar]
- Haemoglobin Q 9 India (alpha 64(E13) aspartic acid histidine) associated with beta-thalassaemia observed in three Sindhi families. J Med Genet. 1972;9(4):436-42.
- [Google Scholar]
- Study of hematological and genetical characteristics of Cutchhi Bhanushali community. Indian J Med Res. 1972;60(2):305.
- [Google Scholar]
- Spectrum of haemoglobinopathies in the state of Orissa, India: a ten years cohort study. J Assoc Physicians India. 2005;53:1021-6.
- [Google Scholar]
- Haemoglobin E disorders in the north east India. J Assoc Physicians India. 2000;48(ll):1082-4.
- [Google Scholar]
- The distribution of abnormal haemoglobins in the Indian population. Proceedings of the First Conference of the Indian Society of Human Genetics In: Human Population Genetics in India. Vol Vol 1. Mumbai: Brient Longman; 1973. p. :91-111.
- [Google Scholar]
- Beta thalassaemia trait-fitness for fighter flying: Two case reports. IJASM. 2002;46(1):75-82.
- [Google Scholar]
- Prevalence of β-thalassaemia and other haemoglobinopathies in six cities in India: a multicentre study. J Community Genet. 2013;4:33-42.
- [Google Scholar]
- U.S. Navy Aeromcdical Reference and Waiver Guide para 8.1 and 8.5. revised Jun 2000
- [Google Scholar]
- The Manual of Medical Examinations and Medical Boards. IAP 4303. (4th ed). Section 6.16
- [Google Scholar]






