Translate this page into:
Spirometry
Background
Spirometry or the Pulmonary Function Test (PFT) is a physiological test that measures how an individual inhales or exhales volumes of air as a function of time. It is one of the basic tools for evaluating a patient's respiratory status. It is often the first diagnostic work up for patients suspected with any pulmonary disease. The primary signal measured in spirometry may be volume or flow. Flow volume loops provide a graphical representation of the patient's respiratory efforts, where flow is plotted against volume and time. It can also evaluate reversibility of airways obstruction with the use of bronchodilators. After spirometry is completed, patient is given an inhaled bronchodilator and the test is repeated. The most important aspects of spirometry are the Forced Vital Capacity (FVC), which is the volume delivered during expiration made as forcefully and completely as possible starting from full inspiration and the Forced Expiratory Volume (FEV1) in one second, which is the volume delivered in the first second of an FVC maneuver. If the variability of the results can be diminished and the measurement accuracy can be improved, the range of normal values for populations can be narrowed and abnormalities more easily detected. The Snowbird workshop held in 1979 resulted in the first American Thoracic Society (ATS) statement on the standardisation of spirometry. This was updated in 1987 and again in 1994. A similar initiative was undertaken by the European Community for Steel and Coal, resulting in the first European standardisation document in 1983. This was then updated in 1993 as the official statement of the European Respiratory Society (ERS). There are generally only minor differences between the two most recent ATS and ERS statements, except that the ERS statement includes absolute lung volumes and the ATS does not.
Technique of Spirometry
The patient must be clinically stable, should sit straight, with head erect, nose clip in place and holding the mouth piece tightly between the lips. Initially, he or she should breathe in and out at the tidal volume, to record the tidal flow volume loop. Then, when the patient is ready, the technician instructs him/her to inhale maximally to TLC (Total Lung Capacity) and exhale as fast and as completely as possible to record the FVC (Forced Vital Capacity). The point at which no more air can be exhaled is the RV (Residual Volume). The patient is then instructed to inhale fully to TLC again, to record the IRV (Inspiratory Reserve Volume). The test is then repeated to ensure reproducibility to meet quality control criteria (American Thoracic Society or ATS Criteria).
Measured Lung Volumes and Capacities in Static and Dynamic Pulmonary Function Tests
Static Spirometry
Tidal Volume (TV): The volume of air inspired or expired during one breath (approx. 500ml).
Inspiratory Reserve Volume (IRV): Maximum inspiratory volume over and above Tidal Volume (approx. 2.5-3.0 L).
Inspiratory Capacity (IC): Maximum inspiration including Tidal Volume (approx. 3-3.5L).
Expiratory Reserve Volume (ERV): Maximum expiratory volume after expiration of Tidal Volume (approx. 1.3 L).
Vital Capacity (VC): The volume of air measured during maximum inspiration followed by maximum expiration (approx. 4.8L in males, 3.2 L in females).
Residual Volume (RV): The volume of air remaining in the lungs after maximal expiration (approx 1-1.2L).
Functional Residual Capacity (FRC): The volume of air remaining in the lungs after forceful expiration (approx. 1-1.2L)
Total Lung Capacity (TLC): The volume of air in the lungs after deepest possible inspiration (approx. 5.8-6L)
Dynamic Spirometry (Plotted with time)
Forced Vital Capacity (FVC): When the vital capacity is timed and split in the graph on the basis of seconds.(approx 4-5L)
Peak Expiratory Flow PEFx: Peak expiratory flow at x% of FVC. Can be PEF25, PEF50, or PEF75.
FEV1: Air expired at the end of first second of FVC.
Forced Expiratory Flow (FEF25-75): Maximum flow rate in the middle 50% of forced expiration.
Residual Volume and Functional Residual Capacity (Air after normal expiration) cannot be estimated by spirometry. For these special tests need to be done, e.g., Plethysmography, N2wash out, Helium Dilution techniques.
Case Report
A 46 years old male with past history of chronic bronchitis has complaints of worsening cough over the last one month. The cough is productive of two teaspoon full of yellowish mucus. Patient notes dyspnea on exertion. No chest pain or wheezing. No history of fever or chills. The patient also reports fatigue, decreased appetite. He has not been exposed to patients with TB. His last PPD (Purified Protein Derivative) test was done one year back and was negative. On OTC cough syrup, multivitamins and AsthalinTM MDI.
Personal History: Tonsillectomy and adenoidectomy done at age 11. Smoking cigarettes, one to two packs per day for 35 years; stopped 2 years ago.
Physical Examination : Patient is in no acute distress and vitals are normal.
ENT: Mouth and oropharynx WNL.
Neck: No raised JVP, no lymphadenopathy.
Chest: RR-24/min, Bibasal crepts, rhonchi. tactile vocal fremitus normal on both sides.
Heart: Apical impulse not displaced; normal S1/S2; no murmurs, rubs, or gallops.
Abdomen: Soft, non-tender, no hepato-splenomegaly. Extremities: No clubbing, cyanosis, or edema.
Interpretation of obtained values
Interpretation of PFTs is usually based on data measured in an individual subject with reference (predicted) values based on healthy subjects. Predicted values are obtained from studies of healthy subjects with the same anthropometric and, if relevant, ethnic characteristics of the patient being tested. Criteria to define subjects as 'normal' or healthy have been discussed in ATS and ERS statements. There are also criteria for acceptability and reproducibility laid down by ATS to ensure the PFT does not become an effort dependant imprecise test. These are:-
Criteria for acceptability
Lack of artefact induced by coughing, glottis closure, or equipment problems.
Satisfactory start to the test without hesitation.
Satisfactory exhalation with six seconds of smooth continuous exhalation and/or a plateau in the volume time curve of at least one second, or a reasonable duration of exhalation with plateau.
Criteria for reproducabilty
Largest FVC within 0.2L of next largest FVC.
Largest FEV1 within 0.2L of next largest FEV1.
If the two above criteria have not been met, additional spirograms should be obtained.
The parameters can be tabulated and classified into three conditions / abnormalities enumerated in Table 1.

Discussion
As per the introduction given before, the measurements in this case Fig 1.,2 & 3clearly suggest an obstructive pattern in his spirometry, more specifically a variable intrathoracic type of obstruction. His FEV1 came out to be decreased despite salbutamol inhalation. Further classification of his obstructive lung disease, according to GOLD criteria for COPD is given in Table 2.

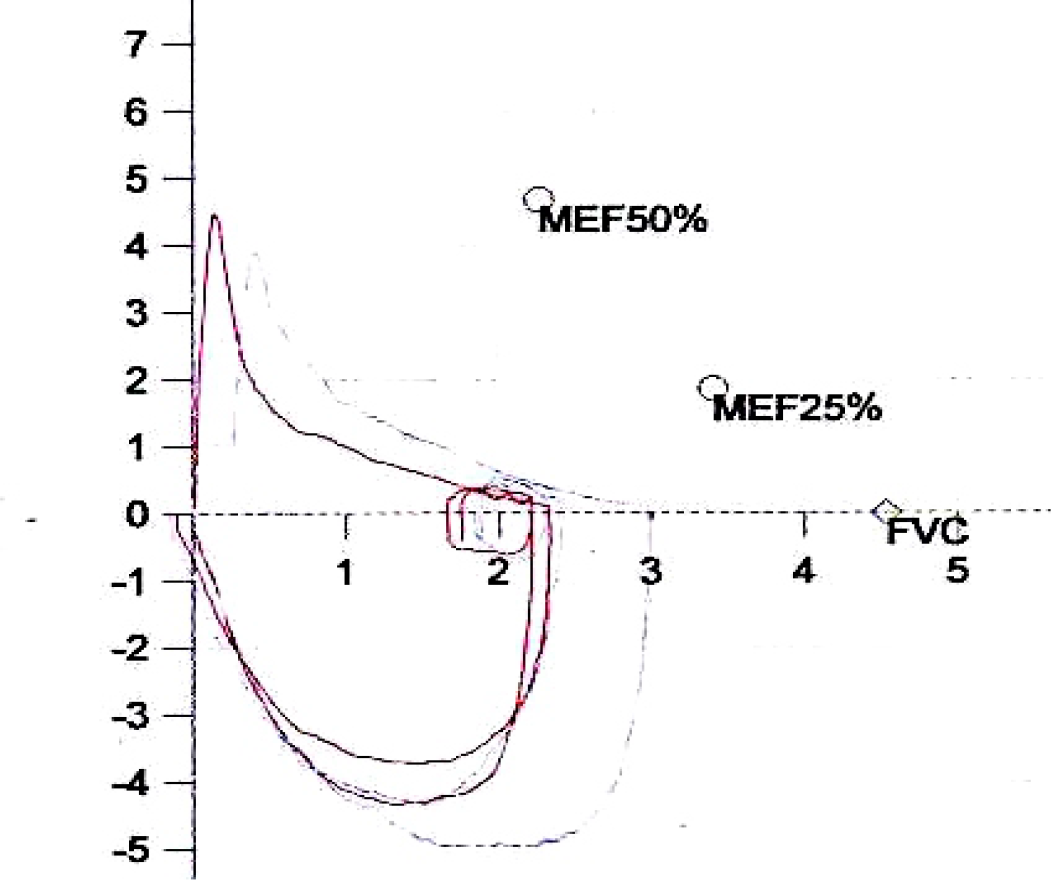
- Flow-Volume Loop
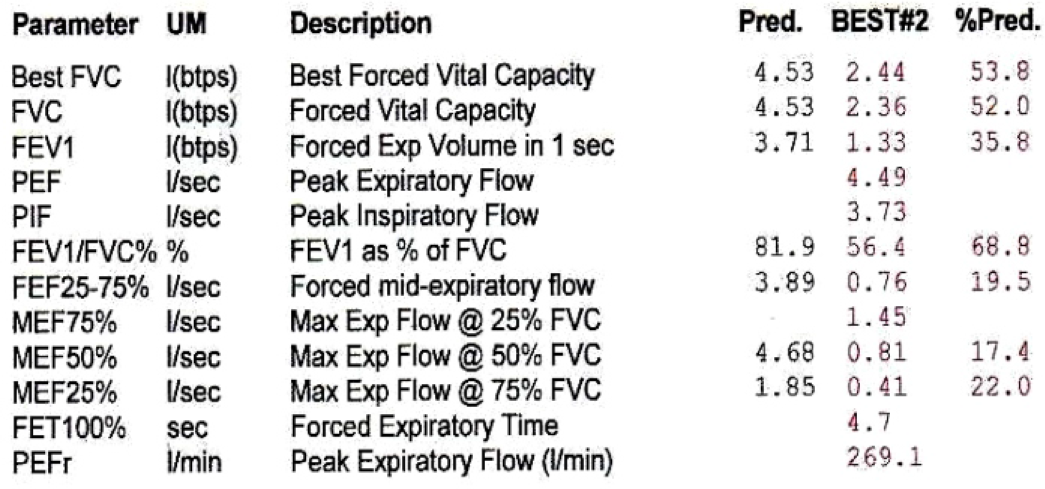
- Patient's Dynamic Spirometry (Measured Values)
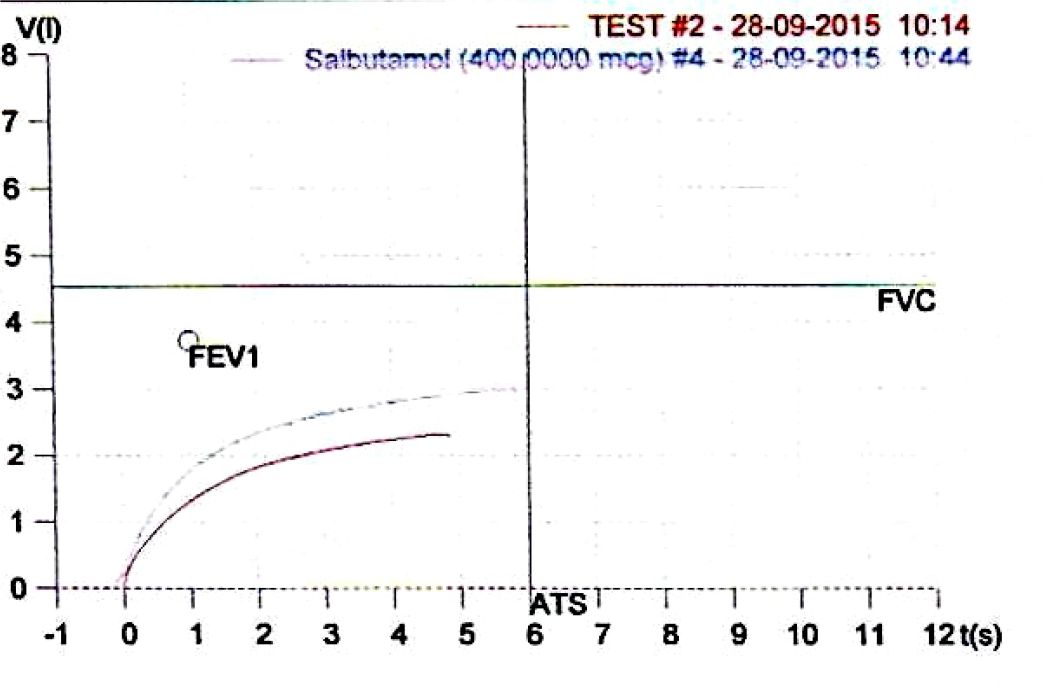
- FEV1 Post Salbutamol Inhalation
Correlating the history and the corresponding data, he is probably a case of exacerbation of chronic bronchitis, in need of augmentation of treatment modalities. His Chest X-ray showed increased bronchovascular markings. He was then sent to the Internal Medicine Specialist for further management and disposal.
Assessing bronchodilator reversibility is important to determine whether fixed airway narrowing is present. Short acting bronchodilators to be withheld 04 hours prior to the testing and 12 hours for long acting bronchodilators. Recent treatment with corticosteroids can also reduce bronchodilator reversibility because the pre bronchodilator FEV1 may improve significantly with inhale corticosteroid therapy, especially if asthma is present. The reversibility of obstruction is checked after administering 400µg of inhaled β2 agonists like Salbutamol (04 inhalations, 100µg each) or 160µg Ipratropium Bromide (04 inhalations, 40µg each). Spirometry is carried out after 20 min of Salbutamol inhalation and 30 min in case of Ipratropium Bromide inhalation. Improvement should be observed by both 12% and 200ml increase either in FVC or in FEV1 post bronchodilator inhalation.
%FEV1 or %FVC Reversibility = [(Post-bronchodilator FEV1 or FVC – Pre-bronchodilator FEV1 or FVC) ÷ Prebronchodilator FEV1 or FVC] x 100
References
- Standardization of spirometry : American Thoracic Society Standardization of spirometry 2005. update
- [Google Scholar]
- European Respiratory System Taskforce for Standardisation of Lung function testing.
- [Google Scholar]
- The rise and dwell time for peak expiratory flow in patients with and without airflow limitation. Am J Respir Crit Care Med
- [Google Scholar]





