Translate this page into:
Role of Myocardial Perfusion Imaging in the Cardiac Evaluation of Aviators
Abstract
In an attempt to provide more accurate and inclusive information regarding the physiological significance of cardiac disease, nuclear myocardial perfusion imaging has evolved into a very sensitive and accurate modality. MPI has the advantage of being able to detect even mild ischemia when only flow heterogeneity is present. All the data available today indicate that a normal stress MPI means <1% chances of hard cardiac events per year and this figure has particular relevance for certification of aviators. Stress MPI has a high negative predictive value for death up to 10 yrs. There is a need to analyze the present trends of its usage in Air force. Hence we undertook this study of retrospectively analyzing 50 consecutive Air force officers referred to our centre for MPI. 50 consecutive Air force officers who were referred for MPI to nuclear medicine centre of command hospital Air force were retrospectively analyzed. Single day protocol was used and Bruce protocol was used for physical stress. Siemens ECAM dual headed gamma camera was used for imaging. Stress gated images were obtained and Emory tool box auto cardiac software was used for processing the image. QGS and QPS software was used for scoring and functional analysis. 26 cases were referred for ECG abnormality out of which 4 cases were detected to have perfusion defects and later underwent coronary angiography followed by revascularization. All these 4 MPIs were true positive. 5 cases were referred for having positive TMT to exclude false positivity. Only one out them (20%) was detected to be positive. There were 7 cases referred for atypical chest pain out of which one case turned out to have RPD in inferior segments. Three MPIs were done for patients who underwent primary PTCA to check for the success of revascularization. Nine cases were follow-up cases of CAD. 7 out of these 9 cases had abnormal MPI, out of which 1 had reversible defect and the others had fixed defects. Among the non-invasive methods of cardiac evaluation MPI has emerged as one of the most important modality in the past few years. It has the advantage of detection of CAD at a very early stage when only flow heterogeneity is present. MPI has a much better diagnostic accuracy than stress ECG alone and hence this leads to avoiding unnecessary angiographies. Although coronary angiography provides clinically valuable information, its invasive nature and costs precludes its routine use in the evaluation of patients after intervention. MPI with its ability to provide information about the physiological significance of stenosis, extent of ischemia and scar, global LV function, viability and prognosis is hence ideally suited to assess patients after intervention also. Myocardial perfusion imaging has a high diagnostic accuracy in the detection, prognosis and follow-up of patients of coronary artery disease. The aviators are a special group of people in whom we need to use MPI more liberally due to its high negative predictive value, non-invasive nature and lower costs.
Keywords
MPI
stress
coronary artery disease (CAD)
reversible perfusion defect
Introduction
CAD is a major cause of death around the world. In an attempt to provide more accurate and inclusive information regarding the physiological significance of cardiac disease at lower or comparable cost, nuclear cardiology has evolved into a very accurate and cost effective modality (1, 2). In the ischemic cascade of coronary artery disease, first change to occur is flow heterogeneity followed by diastolic dysfunction, systolic dysfunction then later ECG changes and lastly angina (3). Myocardial perfusion imaging has the advantage of detecting even mild ischemia when only flow heterogeneity is present where as stress ECG requires much higher levels of ischemia to be positive (4). Then there are certain factors such as abnormal ECG, prior MI, hyperventilation, neurasthenic changes, drug intake and LVH that impede the interpretation of ECG (5). Hence one can conceptualize that perfusion imaging has greater sensitivity and specificity for detecting and ruling out CAD (6). In post intervention patients also routine ECG stress testing has been reported to have a low sensitivity (60%) despite a high specificity (86%) for detecting graft occlusion or stenosis (7). In this regard MPI sensitivity and specificity are comparable to those in native vessels – 86-96% sensitivity and 62-82%specificity (8, 9).
All the data available today indicate that a normal stress MPI means <1% chance of hard cardiac event per year and it has a high negative predictive value for death up to 10 yrs ( 10, 11). This figure has particular relevance for certification of aviators. This modality should be used more liberally especially in a special group like the aviators. There is a need to analyze the present trends of its usage in Air force. Hence we undertook this study of retrospectively analysing 50 consecutive Air force officers referred to our centre for MPI.
Material and Methods
50 consecutive Air force officers who were referred for MPI to nuclear medicine centre of command hospital Air force were retrospectively analysed. There were three subgroups of patients – 1) Aviators referred for asymptomatic ECG abnormalities, 2) Those having routine stress ECG positive for inducible ischemia and 3) Patients referred for MPI after primary PCI. Single day protocol was used and Bruce protocol was used for physical stress. At peak exercise patients were injected with 10 mci of Tc-99m Tetrofosmin / MIBI and imaging was done 30 minutes post injection. Siemens ECAM dual headed gamma camera was used for imaging. Stress gated images were obtained and Emory tool box auto cardiac software was used for processing the image. QGS and QPS software was used for scoring and functional analysis. If the study was normal no further imaging was done. If there was abnormality detected, the patient was re-injected with 30 mci of same radiopharmaceutical after 4 hrs and rest imaging was done 45 minutes post injection. Written consent was taken from all the patients and all were explained the radiation and risks involved.
Results
In our analysis 52% cases referred for MPI were for asymptomatic ECG abnormality. Out of this13 cases (26% of total) were for changes in Inferior leads (Table-1). The other ECG abnormalities for which the patients were referred were RBBB, LBBB and changes in chest leads (Table-2). Out of these 26 cases referred for ECG abnormality, 4 cases were detected to have perfusion defects and later underwent coronary angiography followed by revascularization. All these 4 MPIs were true positive.
| INDICATION | NORMAL | ABNORMAL | TOTAL |
|---|---|---|---|
| CHEST PAIN | 6 | 1 | 7 |
| CAD | 2 | 7 | 9 |
| ECGABNORMALITY | 22 | 4 | 26 |
| TMT POSITIVE | 4 | 1 | 5 |
| PRIMARY PTCA | 0 | 3 | 3 |
| INDICATION | NORMAL | ABNORMAL | TOTAL |
|---|---|---|---|
| RBBB | 7 | 0 | 7 |
| LBBB | 0 | 1 | 1 |
| T INV INFERIOR LEADS | 13 | 3 | 16 |
| T INV OTHER LEADS | 2 | 0 | 2 |
| TOTAL | 22 | 4 | 26 |
There were 5 cases referred for having positive TMT to exclude false positivity. Only one out them (20%) was detected to be positive with reversible perfusion defect in the antero-septal and apical segments (Fig-1). This case later was detected to have TVD and was referred for CABG. The other 4 cases had normal perfusion and function at stress. There were 7 cases referred for atypical chest pain out of which one case turned out to have RPD in inferior segments. He under went CAG and was found to have 99% RCA block. He underwent successful PTCA.

- Stress MPI study (long and short axis view) showing reversible perfusion defect in the antero-septal and apical segments.
Three MPIs were done for patients who underwent primary PTCA to check for the success of revascularization. Nine cases were follow up cases of CAD. 7 out of these 9 cases had abnormal MPI, out of which 1 had reversible defect and the others had fixed defects. The case which had reversible defect underwent angiography and was detected to have re-stenosis of RCA stent.
Discussion
Among the non-invasive methods of cardiac evaluation MPI has emerged as one of the most important modality in the past few years. It has the advantage of detection of CAD at a very early stage when only flow heterogeneity is present (3). The aviators belong to a special group where we need a diagnostic modality with high negative predictive value. A normal MPI as shown in many multicentric registry studies means a less than 1% hard cardiac event rate per year (11). This has also been shown in many individual studies (10). Hence this has an immense importance in certification of aviators.
MPI has a much better diagnostic accuracy than stress ECG alone and hence this leads to avoiding unnecessary angiographies due to high false positive rates (6). In our study MPI resulted in detecting 80% false positive stress tests and hence avoided unnecessary interventions.
Although coronary angiography provides clinically valuable information, its invasive nature and costs precludes its routine use in the evaluation of patients after intervention. MPI with its ability to provide information about the physiological significance of stenosis, extent of ischemia and scar, global LV function, viability and prognosis is ideally suited to assess patients after intervention (12). In our analysis there were 9 cases of CAD who had undergone revascularization earlier and were referred for ruling out ischemia due to either clinical suspicion of restenosis or positive stress ECG. There was only one patient detected to have reversible ischemia. All others had fixed defects. Development or recurrence of chest pain post revascularization may have different causes and therefore its sensitivity for graft dysfunction is only 60% and specificity 20% (13). Routine ECG stress testing has also been reported to have a low sensitivity (60%) despite a high specificity (86%) for detecting graft occlusion or stenosis (7). In this regard MPI sensitivity and specificity are comparable to those in native vessels – 86-96% sensitivity and 62-82%specificity ( 8, 9). Serial Tl-201myocardial perfusion scan has shown to have an overall accuracy of 86% in detecting or excluding graft occlusion (14). Now with better imaging equipment and newer radio pharmaceuticals the diagnostic yield is even better. The other advantage of MPI over stress ECG is in the localization of zone of ischemia, capability of detecting ischemia within a zone of infarction, assessment of viability, assessment of LV function, detection of culprit vessel prior to intervention, assessment of periinterventional myocardial damage and the follow up of patients post intervention.
Another important subgroup of patients in our analysis was patients with baseline ECG changes who were directly sent for MPI. In this group there were total 26 patients out of whom 4 were detected to have reversible perfusion defects. Out of these 4, one had LBBB who was detected to have defect in the inferolateral segments and the rest 3 had inverted T in inferior leads and they were detected to have defects in the inferior segments. In the patient with LBBB we undertook Adenosine stress as is recommended. A physical stress leads to false positivity in these cases due to septal defect normally seen at high heart rates. Hence a vasodilator stress is recommended (15). We found reversible defect in the infero-lateral segments and angiography revealed circumflex disease.
There were 2 cases referred for MPI immediately after primary PTCA to assess the success of revascularization and residual damage. Also the functional analysis and scoring at this time served as the baseline for subsequent follow up. One patient showed improvement in the perfusion score by 12 after 6months (Fig-2 & 3) and improvement in the LVEF from 41% to 49%. The other patients follow up scan is still awaited. MPI has been frequently used for monitoring the serial changes in myocardial perfusion and function and studies have shown that improvement in both perfusion and function occur over time in patient who undergo revascularization and more in those with increased use of cardiac medications (16).
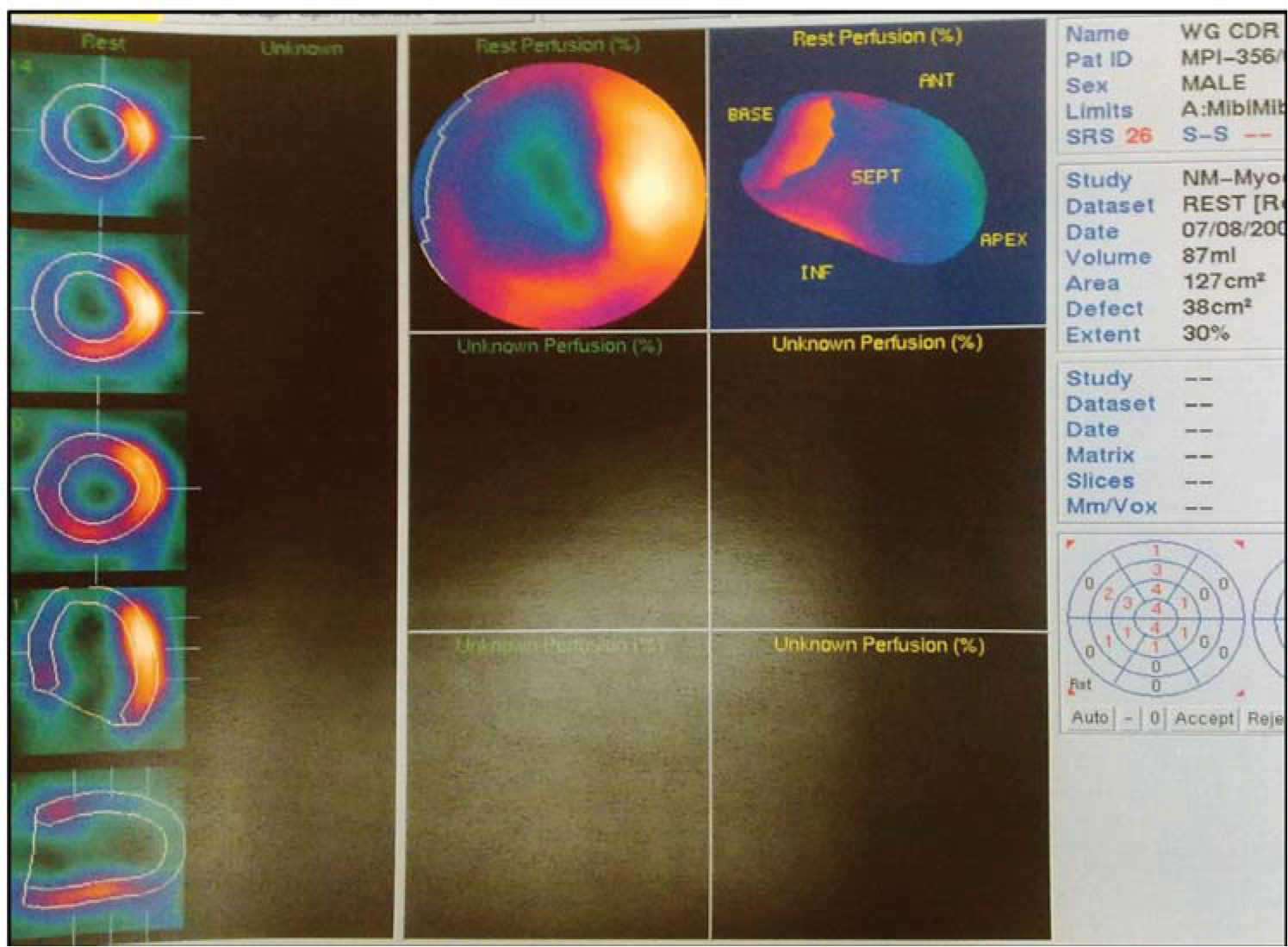
- Resting MPI study done immediately after primary PTCA. Bull’s eye image showing a large perfusion defect in the LAD territory with resting score of 26 and extent of 30%.
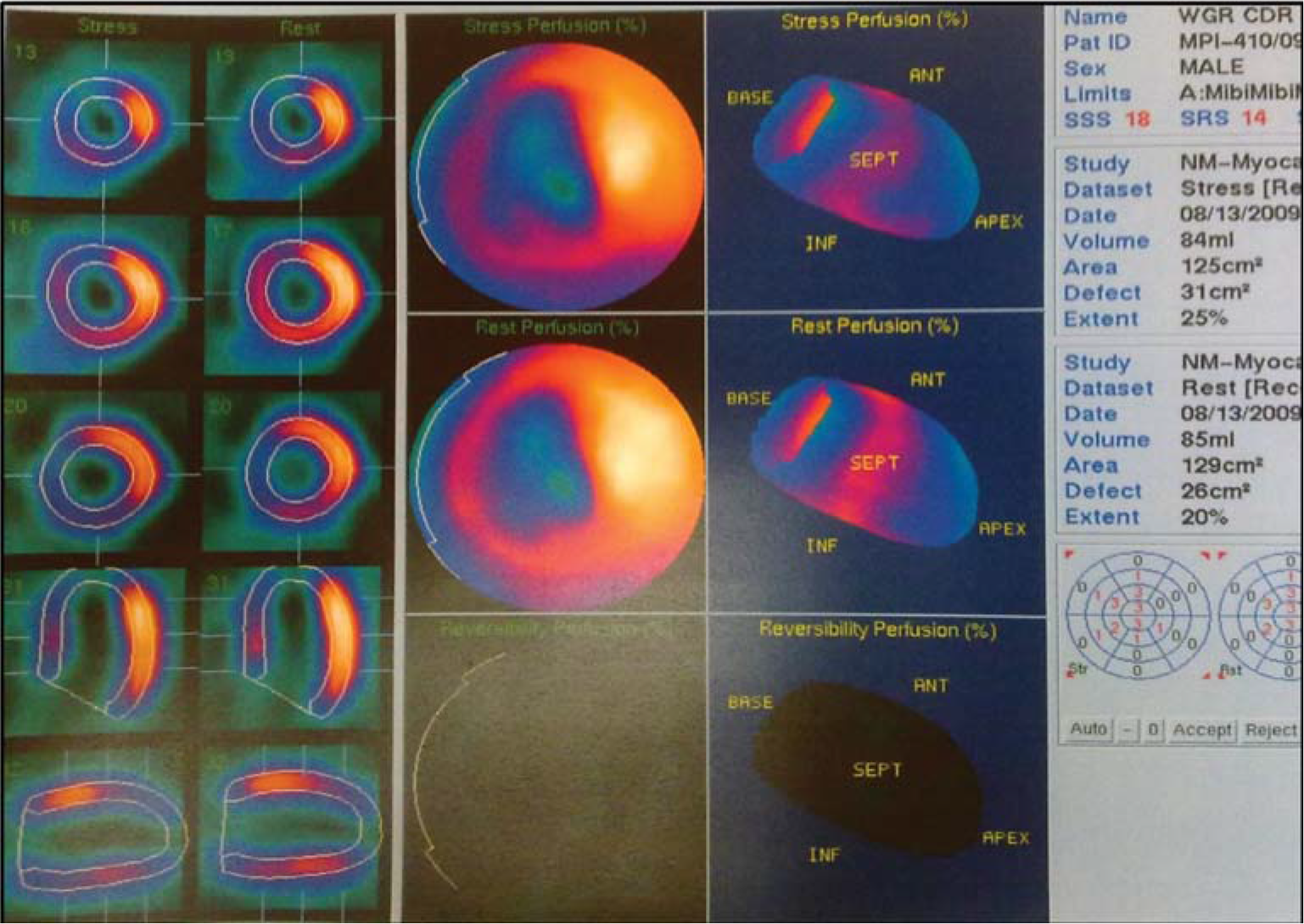
- Stress MPI study of the same patient (Fig-1) after 6months showing decrease in size of perfusion defect with score of 14 and extent of 20%.
Conclusion
Myocardial perfusion imaging has a high diagnostic accuracy in the detection, prognosis and follow-up of patients of coronary artery disease. The aviators are a special group of people in whom we need to use MPI more liberally due to its high negative predictive value, non-invasive nature and lower costs.
References
- Non invasive strategies for the estimation of cardiac risk in stable chest pain patients. The economics of noninvasive diagnosis (END) study group. Am J Cardiol. 2000;86:1-7.
- [Google Scholar]
- The ischemic cascade: Temporal sequence of hemodyanamic, electrocardiographic and symptomatic expressions of ischemia. Am J Cardiol. 1987;59:23-30.
- [Google Scholar]
- Coronory insufficiency: relation between hemodyanamic, electrical and biochemical parameters. Circ Res 1966:18-178.
- [Google Scholar]
- Inability of the submaximal tredmill stress test to predict the location of coronary disease. Circulation. 1973;47:250-256.
- [Google Scholar]
- The efficacy of cardiovascular nuclear medicine exercise studies. Semin Nuc Med. 1987;17:104-120.
- [Google Scholar]
- Relation of silent myocardial ischemia after coronary artery bypass grafting to angiographic completeness of revascularization and long term prognosis. Am J Cardiol. 1990;65:14-22.
- [Google Scholar]
- Long term out come of a residual scar from myocardial infarction after coronary artery bypass grafting-a 100 month study using myocardial perfusion scintigraphy. Circ J. 2002;66:445-449.
- [Google Scholar]
- The value of stress Tl-201 single photon emmission CT imaging as a predictor of outcome and long term prognosis after CABG. J Med. 2001;32:271-282.
- [Google Scholar]
- Risk assessment using single photon emmission computed tomographic Tc-99m sestamibi imaging. J Am Coll Cardiol. 1998;32:57-62.
- [Google Scholar]
- Prognostic value of normal exercise and adenosine Tc-99m Tetrofosmin SPECT imaging–results from multicentric registry of 4728 patients. J Nucl Med. 2003;44:134-139.
- [Google Scholar]
- When to stress patients after coronary artery bypass surgery? Risk stratification in patients early and late post-CABG using stress myocardial perfusion SPECT: implications of appropriate clinical strategies. J Am Coll Cardiol. 2001;37:144-152.
- [Google Scholar]
- Angina in patients with occluded aorto-coronary vein grafts. Br Heart J. 1980;43:426-435.
- [Google Scholar]
- Accuracy of serial myocardial perfusion scintigraphy with Tl-201 for prediction of graft patency early and late after CABG. A controlled prospective study. Circulation. 1982;66:1017-1024.
- [Google Scholar]
- ACC/ AHA 2002 guidelines update for the management of patients with chronic stable angina-summary article: a report of the americal college of cardiology/ American heart association task force on practice guidelines. Circulation. 2003;107:149-158.
- [Google Scholar]
- Serial changes on quantitative myocardial SPECT in patients undergoing revascularization or conservative therapy. J Nucl Cardiol. 2001;8:428-437.
- [Google Scholar]






