Translate this page into:
Reflighting of a Case of Lower Cranial Nerve Schwannoma
Abstract
Background:
Schwannomas are encapsulated tumours of pure Schwann cells, growing around the nerve. They can develop at all locations in the body where there are nerves with Schwann cells. Approximately 6-10% of the intracranial tumours affect the Cerebellopontine angle (CPA). 80-90% of these are Vestibular Schwannomas, rest 10-20% are a herterogenous mixture of predominantly benign tumours which can arise from any of the structure of the CPA. Schwannomas arising from the lower cranial nerves are very rare and occur commonly in the region of jugular foramen. The complications arising due to the tumour at the CPA have significant aeromedical risk and concerns.
Case Presentation:
A 29 year old military helicopter pilot presented with reduced hearing in right ear & altered taste perception on right side of the tongue. He was subsequently found to have Right CP angle Lower Cranial Nerve Schwannoma. He underwent conventional surgery followed by Gamma Knife Radiosurgery for the same. Post-surgery he developed late complications of right facial asymmetry, persistent tinnitus & intermittent headache. Hewas managed for all the complications. The pilot became completely asymptomatic and was awarded a flying category after aeromedical evaluation.
Discussion:
Lower Cranial Nerve Schwannomas have aeromedical implications due to the complications arising predominantly from the compression of the adjacent brain tissue. Treatment options involve both resection in a conventional surgery and or using Gamma Knife Radiosurgery. This case report highlights the aeromedical evaluation carried out for a partially resected tumour, before certifying the pilot fit to fly.
Keywords
Lower Cranial Nerve
Schwannoma
INTRODUCTION
Schwannomas are encapsulated tumours of pure Schwann cells, growing around the nerve. They can develop at all locations in the body where there are nerves with Schwann cells. Approximately 6-10% of the intracranial tumours affect the CPA. 80-90% of these are Vestibular Schwannomas. Rest 10-20% are a herterogenous mixture of predominantly benign tumours which can arise from any of the structure of the CPA [1]. Intracranial Schwannomas are not uncommon and account approximately for 7-10% of all the primary brain tumours. Lower Cranial Nerve (LCN) Schwannomas arise from the cranial nerves IX, X, XI in the jugular foramen & cranial nerve XII in the hypoglossal canal [1]. Schwannomas originating in the region of jugular foramen are rare & comprise only 2.9% of all intracranial schwannomas when not associated with neurofibromatosis. The ratio of jugular foramen schwannoma to vestibular schwannomas is 1:24 [2]. Less than 200 such cases have been reported in world literature [3].
Early symptoms depend on the cranial nerve of origin however, this may not be true in cases of jugular foramen tumours because the compartment is so small that all the cranial nerves may be affected at the same time, hence hearing impairment is the most common presentation. As per Hakuba et al. symptoms secondary to raised intracranial pressure viz. headache or blurred vision, are the most common complaints while the most common & earliest sign is the compromise of the Eighth Cranial Nerve complex [4].
Case Report
A 29 years old military aviator from helicopter stream presented with complaints of reduced hearing in right ear and altered taste perception on right side of the tongue. On Magnetic Resonance Imaging (MRI), he was found to have a lesion in the right cerebellopontine angle epicentered at the Jugular Foramen (Type D) (Fig 1). He underwent right retro-mastoid sub-occipital craniectomy & decompression of the intracerebral portion of the tumour one month after detection. Six months later he underwent Gamma Knife Radiosurgery for removal of the residual mass (Fig 2).
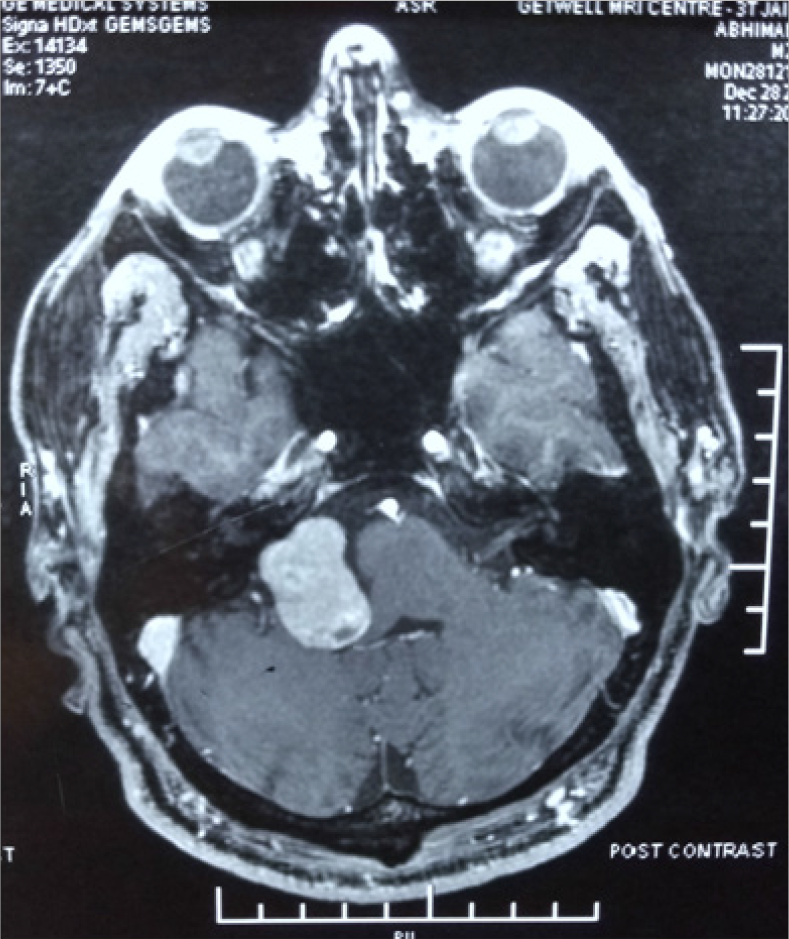
- Pre-operative post contrast MR Image of the tumour (Type D) at Cerebello-pontine angle epicentered in the Right Jugular Foramen.
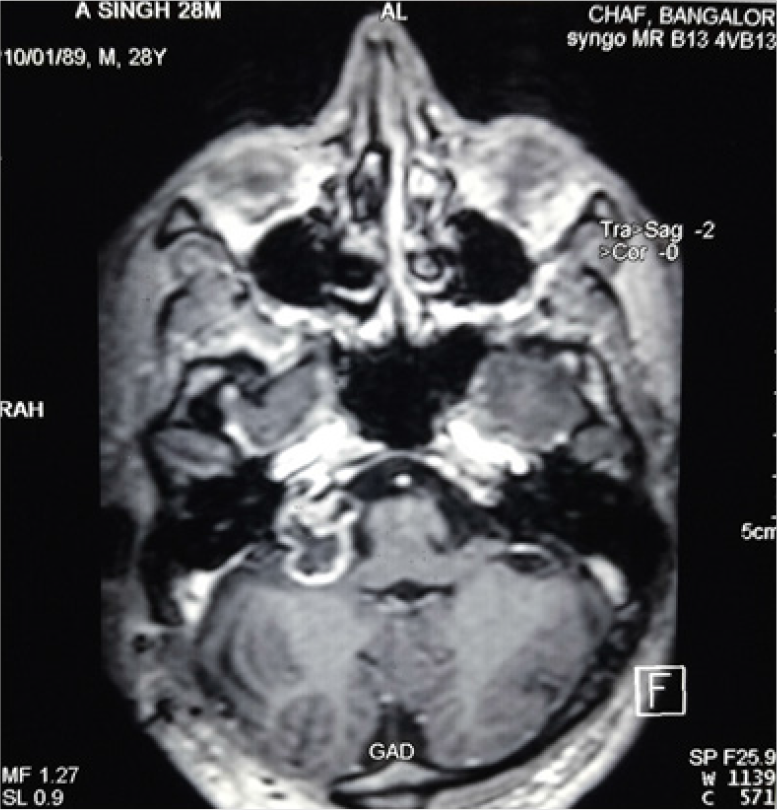
- Contrast enhanced image of remaining tumour mass post Stereotactic Radio-Surgery.
The pilot did not suffer from any immediate post operative complications and had a normal recovery with no symptoms of vertigo, imbalance or headache during the convalescence period. On completion of treatment and observation period of 6 months the aviator was considered for upgradation to a restricted flying category since he was completely asymptomatic. He flew a sortie for his executive report but during the sortie, he developed headache. Subsequently, he continued to have headache with a frequency of two-three episodes in a month. He also developed tinnitus, discharging sinus from the surgical site and diminished sleep. He was observed again in a non-flying category with an advice to maintain a headache diary, to document the frequency of headache. He underwent a sinus tract exploration for the intermittent discharge from the surgical site. Over a period of eighteen months his symptoms of tinnitus and headache reduced. He had undisturbed sleep at night. This was confirmed by Polysomnography (PSG). The report showed normal sleep pattern both in quantity and quality.
After 18 months of close follow up, the pilot reported to IAM with a complimentary ground executive report. All the treating physicians had declared him fit. He had no tinnitus and normal hearing so ENT surgeon had recommended flying fitness. He had no complaints of headache so the neurologist had recommended flying fitness. The surgical site had no discharge and the sinus had healed completely. The treating neurosurgeon had confirmed that his clinical condition (being reviewed by serial MRIs) was static. He also commented that he had residual facial nerve paresis post surgery. He recommended a period of further follow up due to residual mass. The pilot had been upgraded to a restricted flying category. The neurosurgeon did not recommend a further upgradation despite complimentary executive report on flying.
The aeromedical dilemma arose in disposal of an aircrew who was completely asymptomatic, but harboured a residual mass which did not warrant any active intervention. His executive report on flying was complimentary. Complicating further, the patient had a right sided facial nerve paresis which was not evaluated to assess the compatibility for flying.
Therefore, aeromedical evaluation was carried out to assess his fitness to fly with the Rt facial nerve paresis. With facial nerve paresis, fitment of an aviator’s mask without any leakage, was an aeromedical concern. The pilot was made to wear an aircrew assembly comprising of helmet and oxygen mask for 45 min (Fig 3) and his ability to don, doff and wear the assembly for 45 min was tested. The seal between the edge of mask and face was also tested. The air in the Inspiratory hose was squeezed out and the inlet was closed. The officer was asked to suck in all the air from the mask and create a vaccum (Fig 4). This effort created a vacuum in the mask cavity and thereby helped the mask to remain attached to the face without any support or anchoring. The test confirmed that the Rt. facial nerve paresis was not affecting the face mask seal.

- Ability to wear Helmet –Mask assembly for 45 min
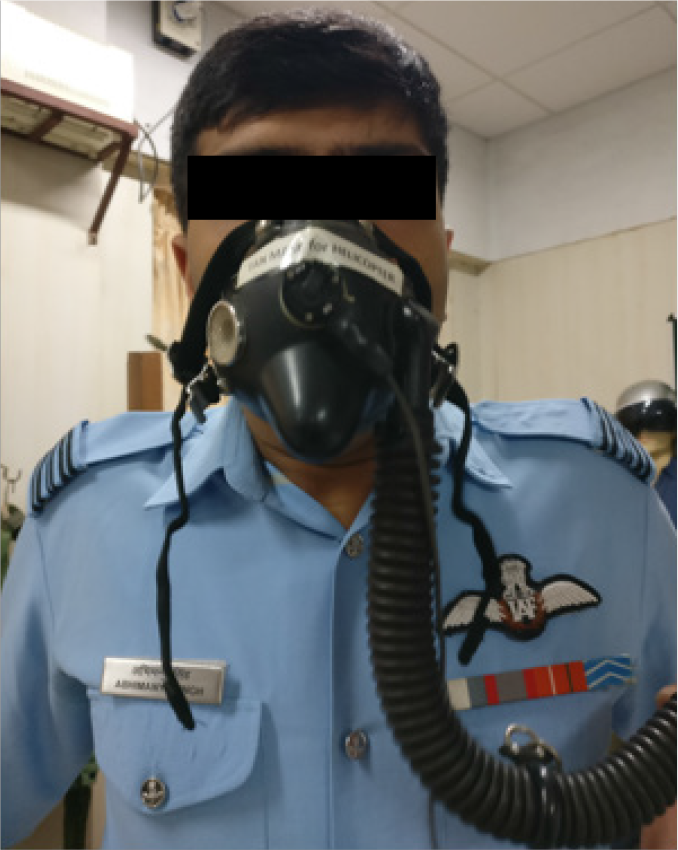
- Ability to create a vaccum after the inlet hose was closed. Displays adequate seal between edge of mask & face.
DISCUSSION
The clinical presentation of LCN schwannomas closely mimics vestibular schwannomas, thus, making it difficult to determine the nerve of origin preoperatively. With the available neuro-diagnostic techniques, these tumours can be detected almost certainly.
Patients often present with a unilateral palsy of one or more cranial nerves. The origin & size of the tumour define the clinical presentation. When tumour grows proximally, it presents as a posterior fossa mass & hearing loss is usually the first symptom to occur thus raising a suspicion of a tumour in the CPA. Distal spreading tumours present as extra-cranial, cervical or skull base masses with clinically evident LCN deficits. Tumours arising in the mid-region tend to expand the temporal bone thus causing facial nerve dysfunction [5].
Samii et al. have classified tumour extension into 4 types depending on the radiological & surgical features (Table 1).
| Tumour Type | Features |
|---|---|
| Type A | Tumour primarily at Cerebello-pontine angle with minimal enlargement of jugular foramen. |
| Type B | Tumour primarily in the Jugular Foramen with Intra-cranial extension. |
| Type C | Primarily extra-cranial tumour with extension into the Jugular Foramen. |
| Type D | Dumb-bell shaped tumour with both intracranial and extracranial components. |
Management of CPA tumours involve resection and Gamma Knife surgery. In the current case at the time of presentation, the tumour was large enough to cause compression of nerves and hence symptoms of tinnitus and hearing loss. During surgery to preserve the cranial nerves, a partial resection was done. The residual mass was treated with gamma knife surgery. The residual mass was followed up for two and half yearspost surgery with serial MRI which did not show any significant change in size of the residual mass.
The US Air Force [11] & US Navy Waiver Guides [6] recommend re-flighting of pilots only after complete resection of the tumour. According to the ICAO, medical certification may be possible with satisfactory follow up and current status reports [12]. In the present case, the pilot had recovered satisfactorily from the surgery with only a minimal cranial nerve damage. The biopsy of the resected mass confirmed that the tumour was benign, and hence chances of metastases and its implications were considered to be insignificant. During the period of observation there was no evidence of any growth of the residual mass. The treating neurosurgeon had opined that the condition was static but wanted further observation. An aeromedical assessment was done and subsequently decision was taken to re-flight a trained aircrew without jeopardizing aerospace safety.
Aeromedical concerns
CPA schwannomas have aeromedical implications due to an array of complications they present with, like progressive hearing loss, tinnitus, cranial nerve deficits, vertigo and imbalance, which can thus, incapacitate an aircrew during flying [6].
Post-surgery the possible complications include cerebrospinal fluid (CSF) leak, meningitis, vestibular compensation symptoms like vertigo and imbalance, hearing loss, tinnitus, facial weakness and headache. In case of partial removal of tumour mass, there is an increased risk of recurrence. By virtue of vestibular nerve dysfunction, the aircrew is also predisposed to an increased risk of spatial disorientation.
Hearing loss in most of the cases is sensorineural & retro-cochlear in origin, often associated with tinnitus. Aircrew with such disability could have difficulty in radio-communication and thereby cannot be considered for independent flying duties.
Unilateral facial weakness hinders in the integration of the face mask thus making an aircrew unfit as fighter flying and also, unfit to fly transport and helicopters in conditions where mask is required like in high altitude flying [5].
Vertigo, regardless of etiology, is unwelcome in the cockpit as it could cause spatial disorientation (SD) during flying and if unrecognized it could be extremely dangerous [7].
Accessory Nerve involvement commonly presents as shoulder pain with clinically evident drooping of shoulder and weakness resulting in difficulty in performing overhead tasks [8]. This can significantly affect an aircrew in performing tasks like operating overhead switches in modern transport or rotary wing aircraft and canopy or ejection handle in a fighter aircraft.
LCN Schwannomas though benign, have a high risk of recurrence if not resected completely thus, necessitating regular long term follow up with MR Imaging [2]. Radiosurgery in cases of partially resected tumours has shown to prolong the duration of recurrence with limited success [9].
Taking into consideration that there is no further progression or resurgence of cranial nerve deficits either as a complication of surgery or due to recurrence of tumour, an approach algorithm was suggested for evaluation of such cases (Fig 5) [10].
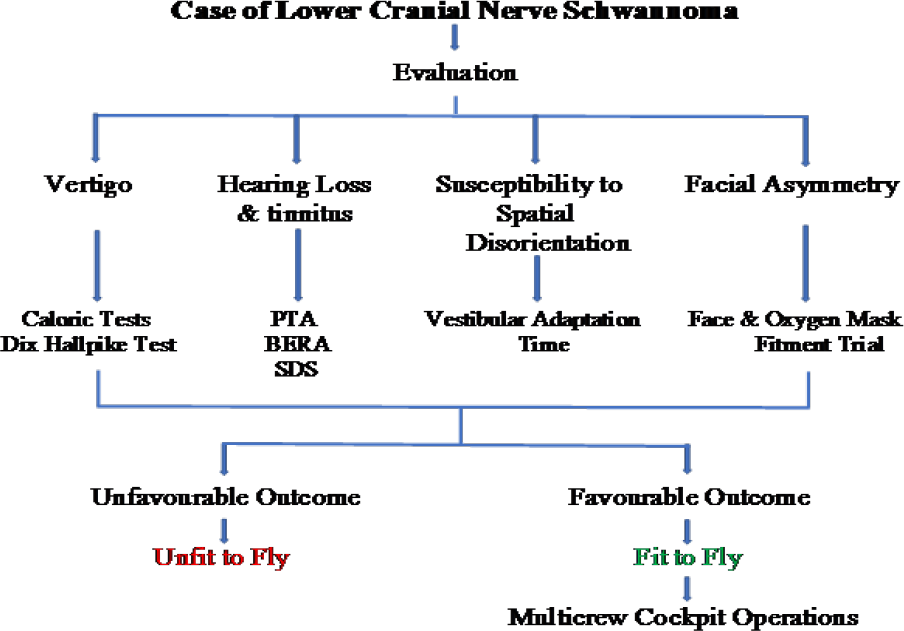
- Approach to a case of LCN Schwannoma – an overview
CONCLUSION
After careful deliberation of all the aeromedical concerns, a decision was taken to reflight the pilot, who is a static case of partially resected LCN Schwannoma. The residual facial nerve paresis and its effect on difficulty in using an oxygen mask was ruled out by the Helmet Mask Fitment trial. Though it had been proposed that susceptibility to Spatial Disorientation by measuring the Vestibular Adaptation Time (VAT) or Coriolis Time Interval (CTI) be checked in such cases; in the absence of normative data, no such test was carried out as such indices would not yield any significant objective value. The last medical board held at IAM recommended the aviator to be upgraded to an unrestricted flying category with an advice to undergo half yearly clinical review at nearest service multispecialty center.
References
- Schwanommas: Jugular foramen lesions and their management. In: Gleeson M, Browning GG, Burton MJ, Hibbert J, eds. Scott - Brown’s Otorhinolaryngology, Head and Neck surgery Vol 2. (7th ed). London (UK): Edward Arnold Publishers Ltd; 2008. p. :2030-35.
- [Google Scholar]
- The lower cranial nerves: IX, X, XI, XII. Diagn Interv Imaging. 2013;94(10):1051-62.
- [Google Scholar]
- Surgical Management of Jugular Foramen Schwannomas With Hearing and Facial Nerve Function Preservation: A Series of 23 Cases and Review of the Literature. Laryngoscope. 2006;116(12):2191-204.
- [Google Scholar]
- Section 6.8. In: Chapter 14 (ENT): Acoustic Neuroma. In: US Navy Aeromedical Reference and Waiver Guide. 2013. p. :96.
- [Google Scholar]
- Otolaryngology. In: Rayman RB, Devenport ED, Rampon DM, Giltow S, Hastings JD, Ivan DJ, Kruyer WB, Pickard J, eds. Rayman’s Clincal Aviation Medicine (5th ed). New York (USA): Castle Connolly Graduate Medical Publishing Ltd; 2013. p. :299-300.
- [Google Scholar]
- Shoulder Disability After Different Selective Neck Dissections (Levels II-IV Versus Levels II-V): A Comparative Study. Laryngoscope. 2005;115(2):259-63.
- [Google Scholar]
- Long Term Outcomes of Gamma Knife Radiosurgery for Vestibular Schwannoma. Journal of Neurosurgery-Part B. 2014;75
- [Google Scholar]
- Fitness to Fly: Lower Cranial Nerve Schwannoma Poster presented at 89th Annual Scientific meeting of AsMA, Dallas, Texas 2018. p. :6-10.
- [Google Scholar]
- Section 10.5.2. Chapter 10 (Neurological disorders): Benign neoplasm. Manual of Civil Aviation Medicine, Doc 8984 AN/895. In: International Civil Aviation Organization (3rd ed). 2012. p. :317.
- [Google Scholar]






