Translate this page into:
Radiological evaluation of lumbar intervertebral instability
Abstract
Spinal instability is defined as an abnormal response to applied loads and is characterized by movement of spinal segments beyond the normal. This abnormal response is due to damage to restraints that hold the spine in stable position. The aim of this article is to review the current concepts of lumbar instability, evaluate the various imaging modalities used and analyze the available diagnostic criteria. Plain radiographs form the base-line investigation but have uncertain diagnostic value as they provide only indirect evidence of spinal instability. Functional radiography is promising however it has its limitations of inaccurate reproducibility, non-standardized techniques and lack of a gold standard. Computed Tomography offers a higher sensitivity than plain radiographs due to its superior contrast resolution and better delineation of bony structures. Functional CT illustrates abnormal motion between the facet joints and objectively establishes spinal instability. MR imaging is highly sensitive in detection of soft tissue abnormalities that contribute to spinal instability. Analysis of the various imaging modalities reveal that no single modality is complete in itself and needs to be complemented by the other.
Keywords
Spinal instability
abnormal translation
Functional radiography
Spinal instability is frequently mentioned, rarely defined and remains a controversial concept due to lack of well-defined clinical or radiological criteria for its evaluation [1].
Lumbar spinal segmental instability is frequently cited as a cause of low backache but its clinical symptoms and signs are non-specific. The clinical history associated with this condition includes recurrent episodes of low back pain, sometimes associated with scoliosis. These episodes are more frequent and severe as the condition progresses.
The associated radiographic signs include traction spurs, disc space narrowing and asymmetric collapse of disc in flexion-extension, mal-alignment of vertebrae in the sagittal plane and abnormal translation and rotation as the spine flexes and extends [2].
Computed Tomography and MR imaging contribute towards better understanding of the cause of spinal instability by evaluating the soft tissues and ligaments with greater detail so as to delineate the associated pathological changes. However, diagnostic criteria and confirmatory radiological signs remain controversial
Definition of Lumbar Spinal Instability
According to the American Academy of Orthopedic Surgeons [3], instability is defined as an abnormal response to applied loads, characterized by movement in the motion segment beyond normal constraints.
A motion segment is the smallest functional spinal unit exhibiting the generic biomechanical characteristics of the spine. It consists of two adjacent vertebrae, an intervertebral disc, various ligaments and apophyseal joints. Stability to the motion segment is provided by the ligaments, facet joints and intervertebral discs which restrict its range of movements [4].
Stokes and Frymoyer [5] defined segmental instability as loss of spinal motion segmental stiffness in such a way that force application to the motion segment produces greater displacement than is seen in a normal structure. This leads to a painful condition with the potential of progressive deformity and places neurological structures at risk.
Panjabi [6] proposed to define clinical instability as a significant decrease in the capacity of the stabilizing system of the spine to maintain the intervertebral neutral zones within the physiological limits, so that there is no neurological dysfunction, no major deformity and no incapacitating pain.
Biomechanical Aspects of Spinal Instability
Spinal stability depends on three functionally interdependent sub-systems namely-active subsystem, passive subsystem and a neural control subsystem. These three subsystems maintain spinal stability both in neutral and extreme positions [6].
The active subsystem consists of muscles and tendon and provides active voluntary or reflex stabilization. Unisegmental muscles such as intertransversarii and interspinalis, located near the intervertebral centre of rotation act as transducers sending information to the neural control subsystem for motion and position controls. Pleurisegmental muscles such as abdominal muscles and erector spinae produce and control movements of the lumbar spine.
The passive subsystem includes vertebral bodies, facet joints and their capsules and spinal ligaments. In flexion the main stabilizing structures are the posterior ligaments, facet joints and the intervertebral disc. In extension, the main stabilizing structures are the anterior part of annulus fibrous and the facet joints. Rotational movements are controlled mainly by the intervertebral disc and facet joints. In the neutral zone of range of motion, muscles and tendons act as transducers alerting changes in position and providing feedback to the neural control subsystem.
The neural control subsystem includes the various transducers and the neural control centers. The transducers provide information to the control centers that determine the requirements to achieve stability.
Segmental lumbar spinal instability is a temporary phase in the degenerative process of the lumbar spine. This process of degeneration [7] has been sub-divided into three phases.
Dysfunction - is the earliest phase in which the affected level of the lumbar spine does not function normally but pathological changes are minimal.
Instability - intermediate phase in which the disc height is diminished and the annulus fibroses bulges all around the circumference of the disc, the ligaments and capsule of the posterior facet joint are lax and the articular cartilage is degenerated. This leads to increased and abnormal movement.
Restabilization - fibrotic and osteophytic stabilization of the segment occurs. This phase is associated with fibrosis within the intervertebral joint, enlargement and locking of the facets and particular fibrosis. It is also associated with loss of nuclear material within the disc and peripheral osteophyte formation. These changes result in increasing stiffness of the joint [8].
Causes of Spinal Instability
Degenerative disease
Post-operative status
Trauma to spine or its surrounding structures.
Development disorders like scoliosis and other congenital spine lesions.
Infection
Tumors - primary or metastasis
Instability of lumbar spine from degenerative causes is a common problem involving mainly the L4-5 and L5-S1 levels. This instability comes from the degeneration of facets and discs resulting in laxity and causes abnormal motion under the physiological load of daily activity. Clinical symptoms and signs of segmental instability are non-specific and include low backache with radicular pain especially when changing position.
Post-operative spinal instability occurs in an operated intervertebral level after disc excision, extensive decompression or at a level adjacent to a spinal fusion. Decompressive surgery leads to muscular and ligamentous damage and any bone removal impair stability at the operated levels. Spinal fusion has been shown to produce stress on the adjacent cephalad or caudal non-fused segments which displaces the center of rotation of the lumbar spine in a cephalad and posterior direction [2].
Radiological Evaluation
The diagnosis of intervertebral instability is based on the indirect and direct radiological findings of an abnormal vertebral motion. Differentiation between normal and abnormal motion, however remains uncertain and challenging. A variety of imaging modalities are currently used to assess spinal instability with each having its merits and demerits.
-
Neutral Radiographs : Provide several indirect signs, which are indicative of or associated with spinal instability :
Moderate disc degeneration with mild space narrowing, osteosclerosis and osteophytosis of the vertebral end plates. In contrast marked space narrowing is considered to be indicative of the later stabilization phase [9].
Presence of traction spur, which is a particular type of osteophyte that is located2-3 mm from the end plate and has a horizontal orientation. It is due to the tensile stress exerted by the outer most fibers of the annulus or the anterior longitudinal ligament on the vertebral body periosteum in cases of segmental instability [2].
Intervertebral vacuum phenomenon is the presence of gas collection within the disc and has two main radiological appearances. The typical central vacuum phenomenon is a gas collection that fills large neo-cavity occupying both the nucleus and annulus and is indicative of advanced disc degeneration. The other type of vacuum phenomenon is characterized by gas collection located at the outermost part of the annulus fibroses close to the vertebral corner. It is due to rupture of the insertion of Sharpey's fibers and may be the result of vertebral instability.
The diagnostic value of these indirect signs of spinal instability remains unknown because their sensitivity and specificity cannot be determined in the absence of a well-defined gold standard [2].
Functional Radiography : Can demonstrate intervertebral instability or abnormal motion between two vertebrae. Dynamic radiographs obtained in both flexion and extension prove to be a simple and reliable method to determine motion segment instability apd can also indicate the lesions located in specific areas based on the “dominant lesion” concept [10]. The location of the dominant lesion determines the pattern of instability. If the dominant lesion is anterior primary restraint failure, there is posterior horizontal translation in the extension views. If the dominant lesion is primary posterior restraint failure one should find anterior horizontal displacement in the flexion view and radiologically detectable abnormal patterns of coupling in the posterior elements.
Flexion-extension views can detect four types of segmental instability [11] :
Forward translation of one vertebra over the other - anterior sliding instability.
Backward translation - posterior sliding instability.
Excessive angular movement of a motion segment / rotation - angular instability.
Abnormal axial rotation in which posterior margin of the vertebral body has a focal double contour during bending.
Normal and abnormal measurements
Studies on asymptomatic individuals have shown that even the normal lumbar spine shows translatory and rotational motion of flexion and extension [8]-, however there.is an upper limit beyond which the motion is termed as instability. A number •of studies have been done using flexion-extension radiographs to evaluate the normal and abnormal range of motion, both translatory and angular. Translatory motion is the forward or backward displacement of the vertebral body measured in extreme flexion or extension-respectively (Fig. 1), while rotation is the angle measured at the vertebral end plates adjacent to the discs; a negative angle is seen in extreme extension and a positive angle is seen is extreme flexion (Fig. 2). The results obtained by various studies using functional radiography are given in Table 1 [12, 13, 14].
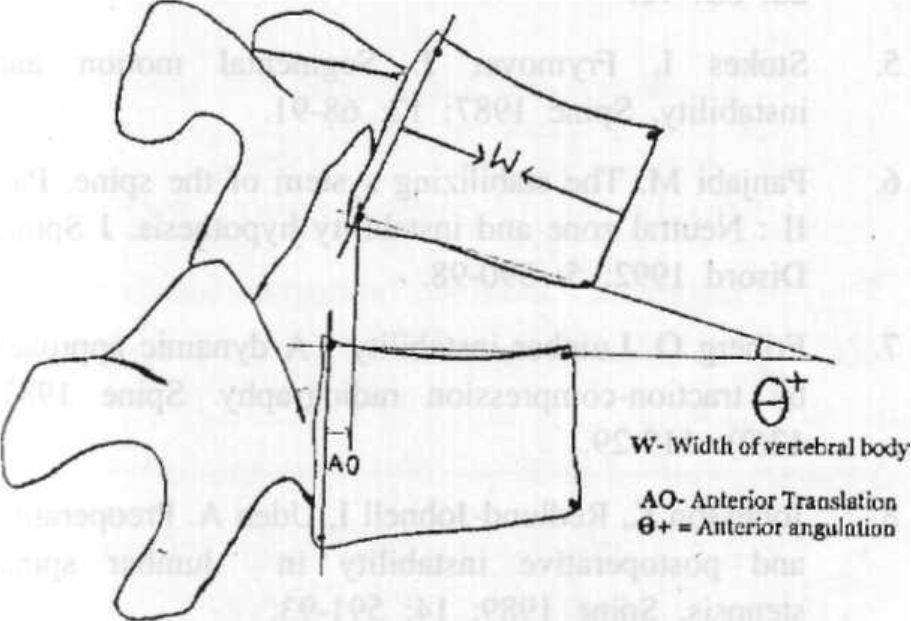
- Technique of measurement of anterior translation and positive / anterior rotation on lateral flexion view of the lumbar spine.
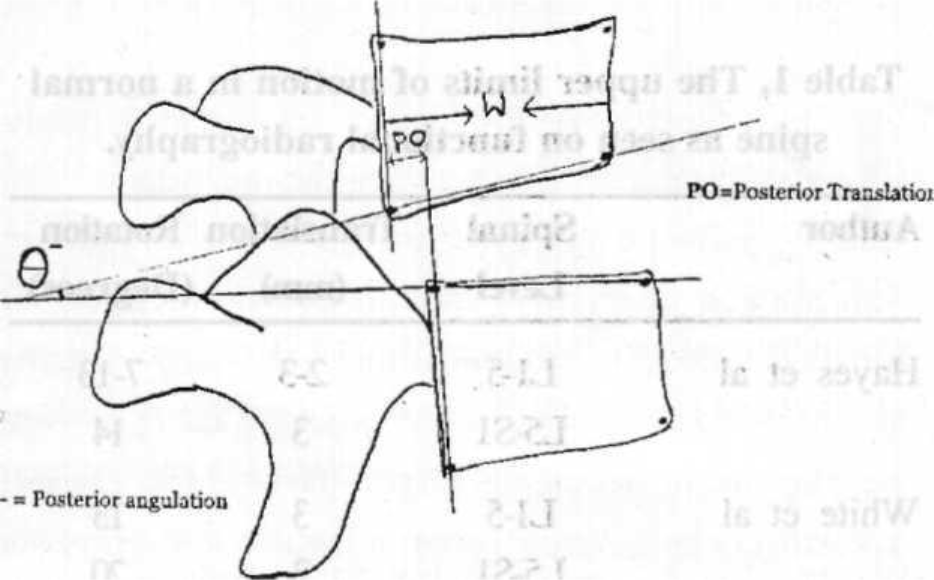
- Technique of measurement of posterior translation and negative / posterior rotation on lateral extension view of the lumbar spine.
Posner et al [15, 16] have measured anterior and posterior translation as a percentage of the vertebral body width and according to their studies the upper limit of normal translatory and angular motions are :
| Level | Anterior translation | Posterior translation | Angulation |
|---|---|---|---|
| Ll-5 | 8% | 9% | , 9% |
| t |
It is quite evident that despite numerous efforts, this method is also debatable and not unequivocal due to reasons like difficulty in exact reproducibility of functional radiography, lack of standardized methods to perform and measure displacements and finally due to lack of well established criteria, to define spinal instability.
References
- Radiological diagnosis of degenerative lumbar spinal instability. Spine. 1985;10(3):262-76.
- [Google Scholar]
- Limited usefulness of traction-compression films in the radiographic diagnosis of lumbar spinal instability : Comparison with flexion-extension films. Spine. 1997;22:193-97.
- [Google Scholar]
- Roentgen graphs evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine. 1989;14:327-31.
- [Google Scholar]
- Phase lag of the intersegment motion in flexion-extension of the lumbar and lumbosacral spine : An in vivo study. Spine. 1996;20:1416-22.
- [Google Scholar]
- A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982;7:374-80.
- [Google Scholar]
- MR abnormalities of the intervertebral discs and adjacent marrow as predictors of segmental instability of the lumbar spine. Acta Radiol. 1998;39:18-24.
- [Google Scholar]
- Lumbar disc high intensity /one Correlation of MRI and Discography. Spine. 1996;21:79-86.
- [Google Scholar]






