Translate this page into:
Prediction of Simulated Blood Pooling in the Leg Segment of an Aircraft Pilot Under G Stress
Abstract
It has been found that G induced loss of consciousness (G-LOC) can abruptly result in pilot incapacitation, mission compromise, loss of aircraft and loss of life. The G-LOC is due to reduced blood flow to the nervous system and reduced flow of blood occurs because of blood pooling in the lower extremity of the aircraft pilot. Therefore, blood pooling has been investigated properly and predicted in the leg segment of aircraft pilot quantitatively, which may be used to avoid the G-LOC. Applied pressure used for occluding the veins is assumed equal to its hydrostatic pressure acting on the leg segment of aircraft pilot during high G stress. The different amount of blood pooling simulated in the leg segment of human volunteers using venous occlusion plethysmography (VOP). Electrical Impedance plethysmography (EIP) has been used to measure simulated blood pooling of leg segment in the laboratory. A characteristic curve is drawn between occluding cuff pressure and its corresponding simulated blood pooling. The drawn curve has been assumed equivalent to the curve drawn between hydrostatic pressure (PII) and its corresponding blood pooling (V) in leg segment under high G-stress. A new formula has been presented using technical geometry that predicts blood pooling in the leg segment of an aircraft pilot against the inertial forces between 1 to 10 G. The predicted range of blood pooling in leg segment of aircraft pilot is 0 to 399 ml. The various graphs have been plotted for blood pooling and hydrostatic pressure of the calf versus inertial forces of aircraft pilot under G stress. Prediction of blood pooling has been made for leg segment of an aircraft pilot using VOP, EIP and technical geometry. A desired profile for inflation of anti-G suit has been proposed to counter the blood pooling occurring during high G maneuvers.
Keywords
Simulated blood pooling
VOP
EIP
Technical geometry
G-LOC
Anti G-suit
Acceleration is an unique environment, which acts directly and continuously upon the body of aircraft pilots during all gravity (G) exposures. The 1 G acceleration is experienced while we stand still on the ground and 2G by making a 60 degree banked turn [1]. Further higher G values are experienced in the human centrifuge. The human centrifuge may be described into four generations such as First Generation (1935-64): Single generation of freedom, slow G onset, passive cab; Second Generation (1964-84): Multi axis (2 degree of freedom), some visuals, some gimbaled; Third Generation (1984-98): 6 G/sec, some flight simulation, gimbaled (active) cab; Fourth Generation (1998-present): 10-15 G/ sec, full flight simulation, gimbaled (active) cab [2]. The G tolerance of the aircraft pilots is increased by so called ‘G protective’ methods such that anti-G suits (AGS), anti-G straining maneuvers (AGSM), positive pressure breathing during G (PBG) and body reclining systems. Ail countermeasures achieve their results restricting the flow of blood from and/or forcing blood to flow’ into particular body segments of the pilot in G cycle [3].
The G is taken as +Gz when the body is accelerated in the headward direction. Blood is constantly pumped into the head against gravity and continued, no matter how hard the heart may work [4,5]. If the +Gz is of high value, little or no blood flow reaches to the head; the eyes and brain exhaust their limited sugar and oxygen supplies and cease to function [6], Maintenance of adequate retinal blood flow is necessary for a full field of vision. The decrement of retinal blood flow causes loss of peripheral vision, central vision, and finally leading to a complete blackout. It leads a threat that can abruptly result in pilot incapacitation, mission compromise, loss of aircraft and loss of life [7]. The G-LOC is the transition from normal consciousness to a state of unconsciousness that results when blood flow to the nervous system is reduced below the critical level necessary to support conscious function. The blood pooling in the different lower body segments is responsible for blood flow decrement that occurs in the head and nervous system [2,6].
Earlier, scientists measured the fluid and blood volume change of abdomen, thigh, and calf of aircraft pilot using electrical impedance plethysmography [8, 9, 10]. The approximate values were defined and failed to give accurate measurements of blood volume change. None of them predicted blood volume or blood volume change in any body segment of the pilot. However, authors analyzed and attempted to predict simulated blood pooling in the leg segment of an aircraft pilot in their earlier study [11]. In the present research paper, a detailed study has been given to predict blood pooling in the leg segment of an aircraft pilot under G stress.
Materials and methods
Sphygmomanometer
The sphygmomanometer is mainly used to measure blood pressure of a person in day-to-day life. The sphygmomanometer consists of an inflatable pressure cuff and a mercury or aneroid manometer to measure the pressure in the cuff. The cuff consists of a rubber bladder inside an inelastic fabric covering it, that can be wrapped around the upper arm and fastened with either hooks or a Velcro fastener. The cuff is normally inflated manually with a rubber bulb and deflated slowly through a needle valve. In present study, sphygmomanometer has been used to simulate leg segment blood pooling of an aircraft in leg of human volunteers in the laboratory. The blood pooling was simulated by placing a blood pressure cuff around the thigh of human volunteers. When the cuff was inflated to pressures beyond venous pressure but below arterial pressure, blood pooling in the leg below the cuff was recorded. The simulated blood pooling has been measured using electrical impedance plethysmography, a non-invasive technique.
Electrical Impedance Plethysmograph
A number of instruments are available commercially with different characteristics and rating for electrical impedance plethysmography. But Electrical Impedance Plethysmograph (EIP) used to measure simulated blood pooling has been designed and developed in the laboratory keeping good sensitivity and reliability. It comprises a circuit consisting of integrated chip (IC) of 20 KHz oscillator coupled through a transformer to a modified Kelvin’s bridge. The current is kept constant at 3 milli ampere. Electrical impedance has been measured by balancing the bridge and observing the result on digital display through an amplifier.
Let all blood vessels of the leg segment be represented by a single cylinder of height equal to length of the leg segment. Cylinder consists of skin, fat, muscles, bones and blood vessels. It is also assumed that the entry of blood changes the diameter only, while the height (Length) remains constant during venous occluding plethysmography. The influence of acceleration and gravitational forces on thé cylinder filled with blood is such that subsequent Eqn. 1 gives hydrostatic pressure (PH) at any point. (1)
r = Specific density of blood, G = Inertial force in G units, and h = blood column height
The hydrostatic pressure developed by inertial response of the blood within the vascular system opposes the systemic arterial pressure of the heart (100 to 120 mm Hg). At higher G, hydrostatic pressure developed significantly reduces blood flow to the brain and consequently blood pooling occurs in the lower body of aircraft pilot. Blood pooling of leg segment of pilot has been simulated in laboratory using sphygmomanometer on the principle of venous occlusion plethysmography.
In the present study, 10 healthy volunteers between the age group of 20 to 45 years were allowed to relax for 5 minutes in the laboratory before the study. The procedure of experiment was explained thoroughly and their consents were taken. Subjects were then made to sit on a chair comfortably. The blood pooling was simulated in leg segment of volunteers using sphygmomanometer and measured noninvasively using electrical impedance plethysmography with tetrapolar configuration. In practice, both bipolar and tetrapolar electrode systems have been employed with EIP [10]. Of these tetrapolar system has a definite advantage, that it provides a uniform current density distribution in the body segment and measures impedance with less electrode interface artifact and impedance errors. In tetrapolar system a pair of surface electrodes (I1, I2) are used as current electrodes to introduce low intensity constant current at high frequency into the leg segment. A separate pair of electrodes (E1, E2) measures changes accompanying physiological events. Voltage has been measured across E1 - E2 that is directly proportional to leg segment electrical impedance (LEI) of human subject. Use of surface circular flat electrodes as well as band type electrodes has been advocated by a number of scientists. But, types of electrodes insignificantly affect the EIP output. Therefore in the present case, 4 band electrodes have been used for convenience.
The current electrodes (I1, I2) were placed around the bottom of leg and below the knee joint to drive 3 milli ampere at 20 KHz of constant current onto leg segment. Potential electrodes E1-E2 were placed towards inner side of current electrodes maintaining a distance of 2 cm. Constant spacing was kept between each current and voltage electrode for repeatable results. All the four electrodes were connected to a Kelvin’s Double Bridge to quantitate impedance value. Bridge was balanced by varying the resistive and capacitive component alternatively. Thereafter, LEI of human leg was observed on the digital output display of electrical impedance plethysmograph.
The LEI lowered during simulated blood pooling in the leg segment of human volunteers. A cuff placed around the thigh just above the knee joint and inflated quickly to a pressure of 20,40,60,80,100,120, and 140 mm Hg. Applied cuff pressures induced different amount of blood pooling in leg below the cuff. The inflation of pressure cuff was maintained for 5 seconds to record electrical impedance of leg segment of human volunteers. The magnitude of blood pooling is assumed to be constant for observation time of 5 seconds at every specific applied cuff pressure. The average values were taken for LEI of human volunteers against the applied cuff pressures and shown in Table 1. The values of electrical impedance change has been used to calculate simulated blood pooling in the leg segment using following Eqn. 2.
(2)Where
Δ Z = Change in electrical impedance of leg segment, Z0 = Normal impedance of leg segment.
V = Volume of leg segment without blood pooling and calculated measuring length and perimeter at mid of the leg segment of human volunteers.
| LEG SEGMENT | |||
| Applied on the thigh (mmHg) | Average Electrical Impedance (Ohms) | Electrical Impedance Change (Ohms) | Simulated Blood pooling (mL) |
| 00 | 46.00 | 0.00 | 0 |
| 20 | 46.00 | 0.00 | 0 |
| 40 | 45.00 | 1.00 | 108 |
| 60 | 44.33 | 1.67 | 184 |
| 80 | 43.33 | 2.67 | 292 |
| 100 | 43.00 | 3.00 | 324 |
| 120 | 42.33 | 3.67 | 399 |
| 140 | 41.67 | 4.33 | 464 |
The 0-10 G equivalent pressures were applied in one sitting and same day on one human volunteer. Thereafter, electrical impedance measurements were made for leg segment of volunteers. The experiments repeated for other subjects on different days and completed within 15 days. Average value of leg segment electrical impedance (LEI) calculated at different cuff pressures and used for further prediction of simulated blood pooling.
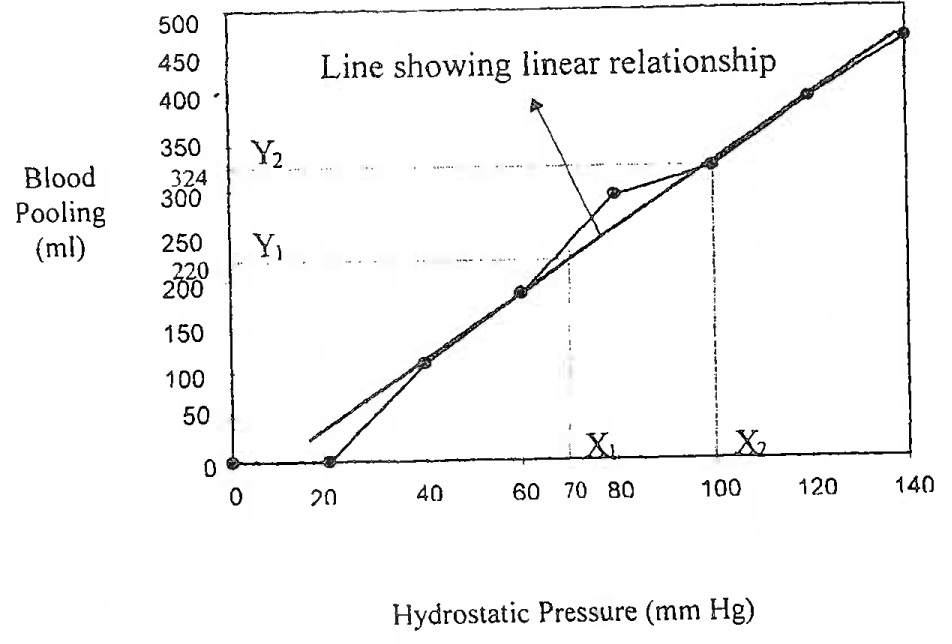
A characteristic curve has been drawn between computed blood pooling and occluding cuff pressure around thigh. The drawn curve shows linear relationship between the simulated blood pooling values and occluding pressures in the cuff.
In sitting posture, occluding cuff pressure inducing simulated blood pooling in the leg segment is assumed equal to its hydrostatic pressure acting during high G maneuvers. It implied that characteristic curve drawn between occluding cuff pressures and its corresponding blood pooling has been considered equivalent to the curve drawn between hydrostatic pressure (pH) and blood pooling (V) of leg segment under G stress. A line approximately passing through all points has been drawn and shown in Fig. 1. The technical geometry of mathematics further used to derive the new expression for predicted blood pooling in the leg segment. The derived equation is given below:
(3)
Detail Of Technical Geometry Used To Derive New Expression For Prediction Of Simulated Blood Pooling In The Leg Segment.
Hydrostatic pressure acting on the leg segment has been found for the given values of G from Eqn. 1. The main effect of high G maneuvers is the blood pooling in the lower extremities of an aircraft pilot such as the abdomen, thighs and legs. Finally the values of blood pooling have been predicted using Eqn. 3. Table II shows prediction of various values of blood pooling in the leg segment of pilot against the G variation from 1 to 10. Further a correlation curve is plotted between inertial forces versus predicted blood pooling of leg segment.
Pressurization levels of an anti G-suit have been proposed against the predicted range of blood pooling in the leg segment under G stress. First pressure level of anti-G suit is in the range of 100-170 mm Hg, if predicted blood pooling is from 0 to 90 ml in leg segment. A corresponding amount of air/O2 producing first level is passed into anti G-suit from sources. Other pressure ranges such as 175 - 225 mm Hg, 325-400 mm Hg, 450-525 mm Hg and 500-600 mm Hg have been defined for blood pooling range of 91-180 ml, 181 -270 ml, 271 -360 ml and 361-450 ml respectively. Anti G-suit is to be deflated to corresponding pressure level if selected blood pooling level falls below the previous level.
| Inertial Force in G units | Hydrostatic Pressure (mm Hg) | Predicted blood Pooling in leg seqment (ml) |
| 1 | 12.8 | 0 |
| 2 | 25.6 | 44.4 |
| 3 | 38.4 | 88.8 |
| 4 | 51.2 | 133.1 |
| 5 | 63.9 | 199.8 |
| 6 | 76.7 | 221.5 |
| 7 | 89.5 | 265.9 |
| 8 | 102.3 | 310.2 |
| 9 | 115.1 | 354.6 |
| 10 | 1127.9 | 399.0 |
Results and discussions
Leg segment Electrical Impedance (LEI) of human volunteers measured using EEP with tetrapolar electrodes configuration and found as 46.0 ohms at normal physiological conditions. Prediction of LEI was also made separately through computer model and found as 46.7 ohms; the value corresponds well with experimental value of 46.0 ohms. The lowered values of LEI have been recorded for different amount of simulated blood pooling.
A new expression has been presented for the prediction of simulated blood pooling in the segment of human volunteers. The graphical representation of predicted blood pooling in the leg segment versus inertial forces is shown in Fig. 2.
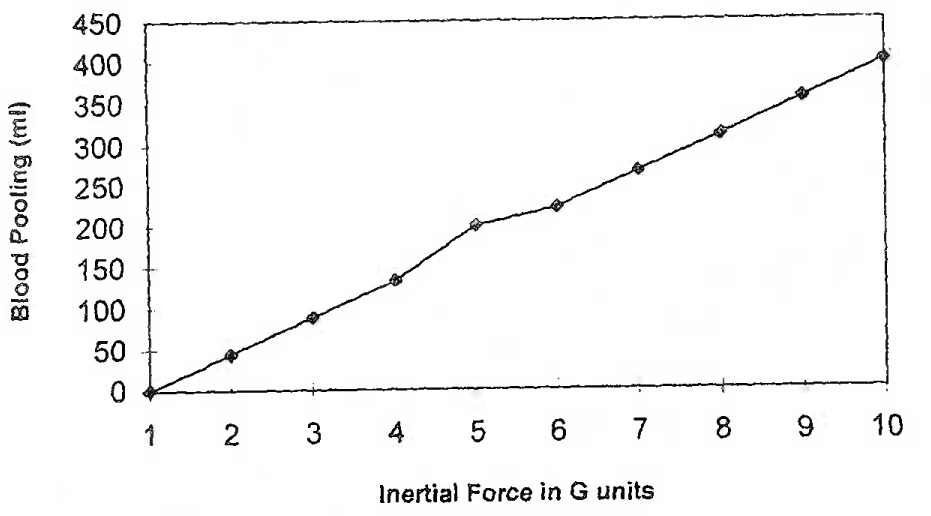
Predicted Simulated Blood Pooling In The Leg Segment Of An Aircraft Pilot.
The blood pooling increases approximately in the linear fashion with increasing the inertial forces in G units. Further pressurization levels have been proposed for an anti G-suit against simulated blood pooling in the leg segment of volunteers and shown in Fig. 3.
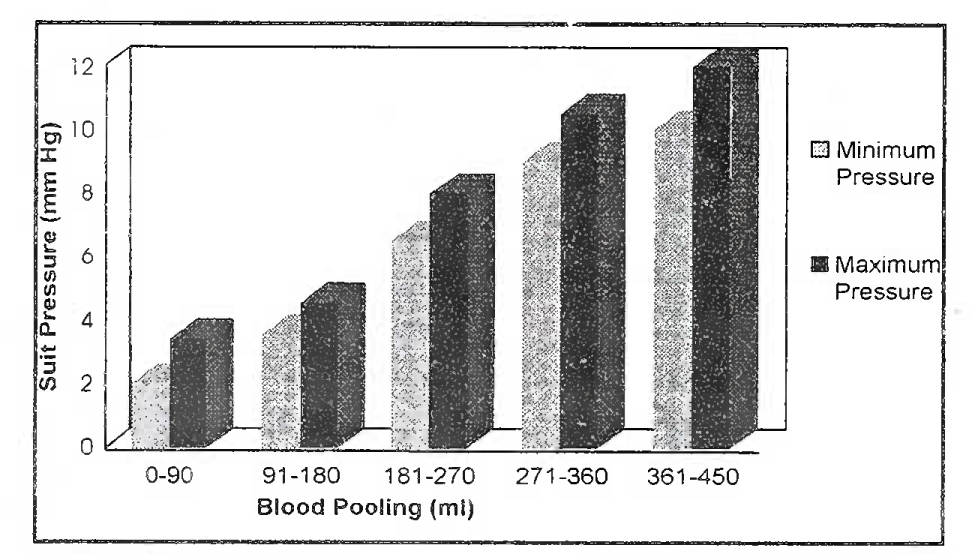
Proposed Pressurization Levels For An Anti G - Suit Of An Aircraft Pilot Under G Stress.
The high inertial and gravitational forces are responsible for producing blood pooling in the lower extremities especially legs of aircraft pilot. Blood pooling plays an important role during complete blackout and G-induced loss of consciousness (G-LOC). These visual symptoms begin to occur when arterial pressure (Pa) at eye level falls below 50 mm Fig. Blackout occurs, if Pa equals the intraocular pressure of approximately 20 mm Hg (3,12). Every pilot has a G-tolerance limit that even with existing protective technology can be exceeded and results in G-LOC. The values of predicted blood pooling may be useful to design a perfect anti-G protection system. The leg coverage of the anti-G suit is being considered the basic component of anti-G protection systems. The leg coverage of the anti-G suit has been recently increased with the development of the advance technology anti-G suit (ATAGS). Flight test results yielded an increased G - level and duration tolerance, by improving blood flow through the skeletal leg muscles (13). It increases the total vascular resistance below the heart, maintaining blood volume distribution within the body, which is found at 1G environment. The results of present study may be used or useful to modify anti-G suit that would remove or reduce the blood pooling in the leg segment of aircraft pilot under G-stress. Thus modifications in the form of advanced anti G-suit will increase the G-tolerance of aircraft pilot. Importance of the predictions will also become more significant when it has to be applied on normal pilots operating in adverse G conditions.
Simulation and modeling processes with slight modification may be used to predict thigh, abdomen and arm blood pooling. Findings of various blood pooling may be used to correiate to the vision of pilots that would start a new era of research in aerospace medicine [10].
The blood pooling of leg segment has been predicted using a totally new approach. An approach can be applied to the pilots before attending actual high G flights and corrective measure would be decided. The predictions of blood pooling in the leg segments may also be exploited in the medical therapy options such as for treating deep vein thrombosis (DVT) and angina pectoris of heart patients. DVT continues to be one of the most common causes of death in the course of medical and surgical illness. It may be diagnosed using a pressure cuff placed on the thigh and inflated to 200 mm Hg to cause the increase of blood volume in the limb. An impedance ratio calculated for leg segment at normal and with increased blood volume helps in detection of DVT [14]. A concept of applied external pressure to lower body segment may be used in Enhanced External Counter Pulsation (EECP). The EECP is a non-invasive technique for treatment of chronic angina due to coronary artery disease [15]. The EECP uses unique equipment to inflate and deflate a series of pneumatic compressive cuffs enclosing the lower extremities. A padded table in which three sets of electronically controlled inflation and deflation valves are located may be administering treatment. These valves are connected to specially designed adjustable cuffs wrapped around patient’s calves, lower thighs and upper thighs, including the buttocks.
Electrical impedance plethysmography (EIP) is a reliable, promising and non-invasive technique for measurement of blood volume changes [10, 16, 17]. The prediction of the blood pooling is based on the measurements of blood pooling using EIP. The experimental verification will be made by measuring the blood pooling in the leg segment of an aircraft pilot in the centrifuge test runs. Based on the results obtained, a system may be designed and developed easily that would measure blood pooling in the lower extremities of an aircraft pilot [17]. A microcomputer controlled biofeedback controller may also be designed and developed for an anti G-suit. The inflation / deflation of an anti G-suit would be according to the actual blood pooling of aircraft pilot [18].
Conclusion
The sphygmomanometer has been used to simulate leg segment blood pooling of an aircraft pilot in the laboratory. Placing and inflation of a blood pressure cuff around the thigh of human volunteers has simulated the blood pooling. When the cuff was inflated to pressures beyond venous pressure but below arterial pressure, blood pooling in the leg below the cuff was recorded. The difference of simulated blood pooling has been measured noninvasively using electrical impedance plethysmography (EIP). The measured values of simulated blood pooling are used to derive a new expression. This new expression predicts a particular amount of blood pooling for each value of G. The range of blood pooling predicted is from 0 to 399 ml in the leg segment of an aircraft pilot under different G stress. The minimum and maximum pressures of air, which are already applied in the anti-G suit according to gravitational forces, have been proposed to different levels of blood pooling. If these proposed levels of air are to be pumped into the anti G-suit, then corresponding blood pooling would vanish or reduce significantly.
References
- G-LOC, Could it happen to you? AOPA (Australia) Magazine. 1990;43(8):1-10. Web pages
- [Google Scholar]
- Human centrifuge: A tool for research and training. Ind J Aerosp Med. 2001;45(2):101-5.
- [Google Scholar]
- Biodynamics. Sustained Acceleration In: DeHart RL, ed. Fundamentals of aerospace medicine Vol 9. (2nd ed). Maryland, USA: William & Wilkins; 1996. p. :201-60. In:
- [Google Scholar]
- Effect of gravitational and inertial force on vertical distribution of pulmonary blood flow. Aviat Space Environ Med. 1978;49(6):768-78.
- [Google Scholar]
- Effects of inertial load and countermeasures on the distribution of pulmonary blood flow. J Appi Physiol. 2000;89:445-57.
- [Google Scholar]
- Observations on the neurophysiologic theory of acceleration (+GZ) induced loss of consciousness. Aviat Space Environ Med. 1989;60:589-93.
- [Google Scholar]
- Characterization of resulting incapacitation following unexpected +GZ induced loss of consiousness. Aviat Space Environ Med. 1987;58:631-6.
- [Google Scholar]
- G-induced loss of consciousness-definition, history, current status. Avia Space Environ Med. 1988;59:2-5.
- [Google Scholar]
- The use of thoracic impedance for determining thoracic blood volume changes in man. Aviat Space Environ Med. 1986;57:49-53.
- [Google Scholar]
- Bioelectric impedance as an index of thoracic fluid. Aviat’Space Environ Med. 1999;70:58-61.
- [Google Scholar]
- Prediction of electrical impedance parameters for the simulated leg segment of an aircraft pilot under G-stress. Aviat Space Environ Med. 2002;73(6):558-64.
- [Google Scholar]
- Prediction of blood pooling in the leg segment of aircraft pilot during high G maneuvers.
- Human centrifuge non-invasive measurements of arterial pressure at eye level during Gz acceleration. Aviat Space Environ Med. 1989;60(10 Pt 1):1005-10.
- [Google Scholar]
- A simple method for detecting deep vein thrombosis: an improved electrical impedance technique. Am J Surg. 1974;127:349.
- [Google Scholar]
- Effects of enhanced external counter pulsation on stress radionuclide coronary perfusion and exercise capacity in chronic stable angina pectoris. Am J Cardiol. 2002;89(7):822-4.
- [Google Scholar]
- Physiologic correlates of protection afforded by anti-G suits. Aviat Space Environ Med. 1990;61:106-111.
- [Google Scholar]
- A system to measure lower body volume changes during rapid onset high-G acceleration. Avia Space Environ Med. 1988;59:1098-102.
- [Google Scholar]
- An experimental microcomputer controlled system for synchronized pulsating anti-gravity suit. Aviat Space Environ Med. 1987;58:710-4.
- [Google Scholar]






