Translate this page into:
Incidence and transmission dynamics of Coronavirus Disease 2019 (COVID-19) among fresh recruits in a Training Establishment of Indian Armed Forces: An observational study

*Corresponding author: Dr MM Sakre, MBBS, MD (Community Medicine), Station Health Organization, Air Force Station, Panagarh, Indian Air Force, Birudiha - 713148, West Bengal, India. drmoinsakre@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sakre MM, Kunte R, Lakhveer S, Sannigrahi P, Devi A. Incidence and transmission dynamics of Coronavirus Disease 2019 (COVID-19) among fresh recruits in a Training Establishment of Indian Armed Forces: An observational study. Indian J Aerosp Med 2021;65:97-104.
Abstract
Introduction:
In times of COVID-19, when all institutions remained closed even post lock-down, the Airmen Training School of Indian Air Force proceeded with the recruitment of airmen. The present study intends to explore the incidence and transmission dynamics of COVID-19 among these freshly recruits who were quarantined in barracks with each barrack serving as one cohort.
Material and Methods:
In an observational study, 2978 male Air Force recruits, between the age group of 18-22 years, in two batches between 1st to 31st July 2020, were followed up in the quarantine period post recruitment. Since the quarantine was unconventional in terms of being in barracks, special and unique precautions such as repeated screening, delegation of specific toilets per billets, three ply mask distributions, Bio-Medical Waste Disposal etc were paid utmost attention. The COVID 19 cases were treated at the in-house isolation facility and the contacts with the symptomatics tested with RT-PCR or RAT before release from quarantine. All individuals were monitored with active surveillance and the data was meticulously maintained with zero attrition. Incidence, Secondary Attack Rate (SAR), demographic characteristics and others aspects of transmission dynamics were analyzed.
Results:
The incidence and SAR was observed to be 8.1% (71 primary cases) and 15.59% (170 secondary cases). 64.7% of cases were symptomatic with an average of 15 days of hospitalization. The rate positivity of testing with RTPCR or RAT was 11.44%. Severity was more marked in the first batch than the second batch of recruits. The overall R0 was found to be 2.39.
Conclusion:
The results of the study revealed some interesting characteristics of COVID-19 transmission dynamics. The cumulative incidence was found to be higher than national average. The variations between the recruits from different part of the country and the two batches could be attributed to the travel distance and mode of conveyance. The study also validates the mild nature of the infection in young adults. Fair conclusion on the implication of good quarantine and isolation measures and regular surveillance for symptoms for early diagnosis has also been compellingly indicated from these observations.
Keywords
Coronavirus disease 2019 (COVID-19)
Incidence
Secondary attack rate
Transmission dynamics
Quarantine
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) coronavirus disease 2019 (COVID-19) – the biggest pandemic the world has ever seen started with a case fatality ratio of as low as 1.49%[1] and yet created havoc among the global population with its vast geographical spread, rate of infectivity, associated morbidity, and the resultant burden on the economy. The effects were more apparent in the second wave witnessed during the months of April–June 2021 in India. In the three complete lockdowns that the nation has witnessed starting from March 24 to June 1, 2020, the most severe was that of interstate travel. The unlocking of the economy started from June 1, 2020, and brought with it the surge of COVID-19 cases making India the country with the second highest numbers of total COVID-19 cases and the third highest numbers of associated deaths.[1] However, even post unlocking, all institutions ranging from primary schools to centers of higher education remained shut indefinitely.
The Indian Air Force, however, decided to go ahead with its process of regular recruitment and basic training of Air Warriors in June, so as not to compromise in the needs and the demands of the Defence system of the country. The usual process of recruitment is usually distributed at various pre-determined stations across the country and such recruited individuals are then sent to the said Institution for subsequent training. In the backdrop of the first wave of the pandemic, in the pre-vaccination era, the otherwise geographically distributed recruitment process of Air Warriors had to be conducted exclusively in this one single ab-initio Training Institute (TI) of the Air Force. Thus, induction of nearly 4000 trainees arriving from different parts of the country was planned and executed meticulously at every stage. It included screening at arrival, compulsory institutional quarantine in barracks, active surveillance for symptoms and testing, isolation, and case management as per the existing protocols. A large number of cases were reported amongst the inductees on arrival with further spread amidst their contacts. This study describes the epidemiology and transmission dynamics of the COVID-19 cases as observed in an institutional setting during this process of induction of nearly 3000 trainees in the period July–August 2020.
Incidence is a good parameter to know the risk/probability of disease in a particular population while Secondary Attack Rate (SAR) serves as a good indicator of success of control measures and gives an idea of the probability of infection in a household or closed community.[2] This report sheds light on these two parameters and aspects of transmission dynamics of COVID-19 in Air Force recruits in a TI in South India in a never before attempted recruitment process in the times of COVID-19.
MATERIAL AND METHODS
A cohort of newly recruited and subsequently quarantined Air Force trainees was followed up and observed for COVID-19 during the first wave in the country. In the scope of this study, 2978 trainees recruited from July 1 to 31, 2020, in first two phases of recruitment in a TI of Air Force have been considered. A negative RTPCR was not mandatory as the disease was in its incipient stage and testing was not as convenient and widespread. The data was collected based on available records during recruitment and training at the Institute.
The trainees reported to the TI in batches of 200 per day and were accommodated in pre-determined flanks in billets as they arrived, thereby creating cohorts of 20 each, that were to be quarantined for 14 days. The blocks were filled up consecutively as the recruits began their quarantine. The quarantine process involved regular bed side screening by medical officers as active surveillance, ear marked toilets per cohort, and adequate protection of the recruitment personnel. Three-ply mask distribution with emphasis on strict compliance on its use, cleanliness and hygiene maintenance at all times, food packaging and delivery at the entrance of each billet, regular Information Education and Communication (IEC) activities, attention to biomedical waste disposal, and ensuring zero contact in between cohorts to ensure no mixing up of individuals was constantly paid utmost attention. Disinfection with sodium hypochlorite was undertaken 2–3 times a day as per the guidelines by the health authorities. All wastes, including food wastes, disposable plates, and masks, were treated as biomedical wastes so as to leave no stone unturned to reduce transmission.
Recording of demographic and enrolment data was taken before the individuals entered the facility. RT-PCR or Rapid Antigen Testing (RAT) was taken up on appearance of symptoms and on high index of suspicion. If positive for COVID-19, they were managed in the designated isolation facility as per the existing guidelines and released only after being tested negative by RT-PCR or RAT. Contacts of the cases who were those sharing the flanks/toilets were labeled as high-risk contacts and were requarantined in the same flank for 14 days from the day of last contact with the case. They were tested on the 8–10th day before exiting the quarantine with a negative test report. The transmission chain was followed up in its entirety till there was no further chance of transmission from the said cohort.
All cases (tested positive on RT-PCR) were treated symptomatically at the in-house 48 bedded isolation facility set up for the purpose of recruitment in the Institute. Those with moderate and severe symptoms were referred to higher center. The criterion for discharge was a negative RTPCR/ RAT after disappearance of all symptoms. In the scope of this report, the following case definitions have been adhered to:
Case: An individual found positive for COVID-19 with or without symptoms by RT-PCR and/or RAT[3]
Contacts: All the individuals in contact with the case 5 days before the onset of symptoms
Incidence: The total number of new cases found positive after arrival among those quarantined individuals[3]
Primary case: An individual found positive for COVID-19 within 5 days (median incubation period) of arrival and being quarantined[4]
Secondary cases: The COVID-19-positive cases that were found subsequent to exposure to a primary case[5]
SAR: The total number of cases found among contacts of the primary cases 5 days after last exposure.[5]
Necessary administrative permissions were taken from the Head of the Institution. Data were collected from observations and available records and were analyzed using statistics that is essentially descriptive in nature. MS Excel and SPSS 23 were used for statistical analysis.
RESULTS
The sample population of 2978, all males between 18 and 22 years, was diverse and represented various parts of the country with varied backgrounds and so did the COVID-19 cases observed among the recruits. While the individuals traveling from northern parts of the country, such as Delhi, Rajasthan, Haryana, UP, MP, and North Eastern states used public transport as a mode of conveyance as bus, train, and flights by a few, the ones from South India were able to choose safer modes of travel such as self-driven cars and taxis.
The cohorts in this study were the barracks in which the recruited trainees were quarantined. A total of 148 such cohorts were created. The overall incidence of COVID-19 among these 2978 recruits was found to be 8.1% (95% CI – 7.96–8.24) with 241 cases. The incidence was much more (10.92%) in the first batch of 2162 recruits with 236 cases than in the second batch (0.61%) among 816 recruits with 5 cases [Table 1].
| Population | Cases | Incidence% (95% CI) |
|---|---|---|
| 1st lot of trainees (n=2162) | 236 | 10.92 (9.7–12.3) |
| 2nd lot of trainees (n=816) | 5 | 0.61 (0.2-–1.4) |
| Total (n=2978) | 241 | 8.1 (7.2–9.1) |
The total strength and number of individuals turning positive in each individual block are depicted in Table 2. The maximum cases came from L2 block (28.22%) followed by K block (26.56%). The incidence within the cohorts varied from 0% to 20% with the maximum incidence in L2 block (20%) followed by S block (15%) and K block (11%).
| S. No. | Quarantine block | Total strength | Total no. of positives | % of positives (incidence) |
|---|---|---|---|---|
| 1. | K | 621 | 64 | 26.56 |
| 2. | M1 | 634 | 49 | 20.33 |
| 3. | M2 | 448 | 0 | 0 |
| 4. | L1 | 471 | 28 | 11.67 |
| 5. | L2 | 470 | 68 | 28.22 |
| 6. | S | 334 | 32 | 13.28 |
| Total | 2978 | 241 | 100% | |
As regard the time distribution of cases, the epidemic curve [Figure 1] showed gradual increase until July 30, 2020, to flatten over the next week and gradually decreased until August 19, 2020. A sharp rise in the epidemic curve that resulted from the contacts turning positive could be noticed from August 20 to 29, 2020. Among the overall cases in these recruits, the maximum number was seen from Uttar Pradesh (41.9%) followed by Rajasthan (19.1%) and Haryana (15.8%) [Figure 2]. The least number of cases among the recruits was seen from Karnataka at 0.41%.
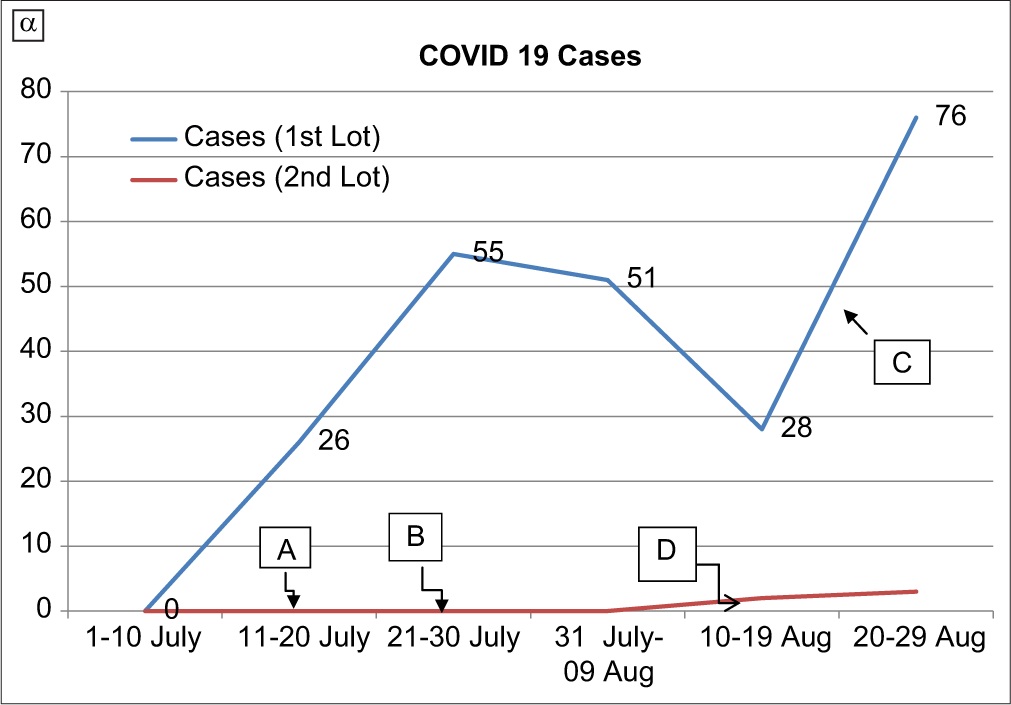
- Epidemic curve of cases of COVID-19 among recruits. A: The end of the first round of recruitment. B: The end of the second round of recruitment. C: The rise in the curve due to the appearance of secondary cases among the first batch of recruits. D: The appearance of two primary and subsequent three secondary cases among the second lot of recruits.
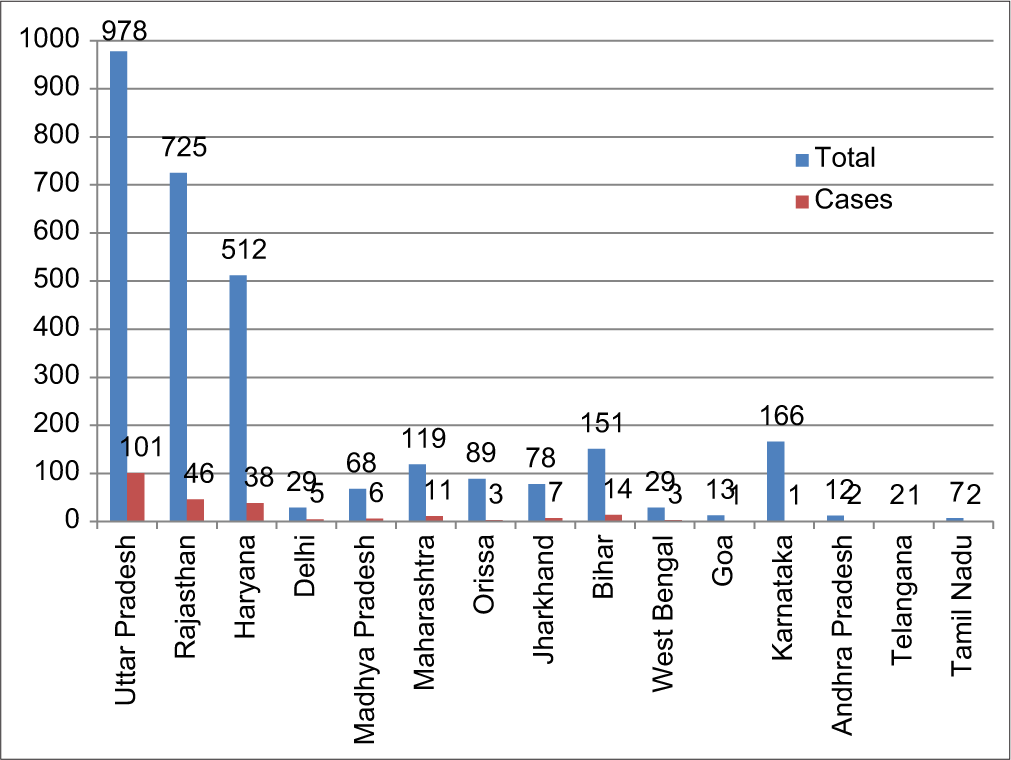
- State wise population and proportion of cases.
The total number of primary cases was 71 with 170 secondary cases [Table 3]. The overall SAR was found to be 15.59% and was more in the first batch (15.97%) of trainees as compared to the second (5.4%) [Table 4]. It was found to be directly proportional to the incidence with the highest being in L2 block (16.2%) followed by S (12.2%) and K block (9.8%) [Table 5]. Incidence and, hence, SAR were nil in M2 block. Averages of 2.39 secondary infections were reported from each infected case. This number or the crude R0 was 2.42 for the first batch of trainees and 1.5 for the second.
| Total population | 2978 (100%) |
| Primary cases | 71 (2.4%) |
| Secondary cases | 170 (5.7%) |
| Total cases | 241 (8.1%) |
| Population | SAR (%) |
|---|---|
| 1stlot of trainees (n=2162) | 15.97 |
| 2ndlot of trainees (n=816) | 5.4 |
| Total | 15.59 |
| S. No. | Quarantine block | Incidence (%) | SAR (%) |
|---|---|---|---|
| 1. | K | 26.6 | 9.8 |
| 2. | M1 | 20.3 | 5.5 |
| 3. | M2 | 0 | 0 |
| 4. | L1 | 11.7 | 4.6 |
| 5. | L2 | 28.2 | 16.2 |
| 6. | S | 13.3 | 12.2 |
Each case was followed up along its transmission chain till the end when no further spread was observed. Observation of the incubation periods of the disease (i.e. appearance of symptoms from the date of last contact) among separate cohorts showed that at least two generations of the disease were noticed among the contact recruits. The serial interval between symptomatic primary and secondary cases was 3 to 11 days with a median of 7 days. Evidence was also sought regarding transmission from asymptomatic cases and it could not be conclusively inferred that such transmission was present, as almost every case was linked to a symptomatic individual and all the transmission chains did not continue beyond for the asymptomatic cases.
Out of the total of 241 cases, a majority of 156 (64.7%) were symptomatic, and 85 (35.3%) were asymptomatic. Of the symptomatic, 93% (145) were mild cases (SpO2 > 94%, pulse rate < 100, respiratory rate < 24, temp < 99° Fahrenheit and/or with mild symptoms such as anosmia, loss of taste, headache, lethargy, and malaise). A few also presented with mild-to-moderate diarrhea. The other 7% showed moderate-to-severe symptoms and were referred to a predetermined referral center for further management. It was noticed that the average duration of symptoms was 12 days and the average length of hospitalization was around 15 days including disappearance of symptoms and discharge after being tested negative with RT-PCR or RAT test. All the 241 cases were discharged post-hospitalization with no residual symptoms and/or complications. All cases made excellent recovery.
In the period between July 1, 2020, and August 31, 2020, following the testing protocol levied at the time, a total of 2106 RT-PCRs and RAT tests were conducted among the symptomatic and the high-risk contacts of those having turned positive. No overlap of RAT and RTPCR was ensured. Two hundred and forty-one of the 2106 tests conducted turned out to be positive for COVID-19 giving an aggregate rate of positivity of testing at 11.44%.
As is required, after the appearance of each case, reset of quarantine clocks for another 14 days was done promptly for all the other inmates of that flank. Longest duration of quarantine was required in several billets of K block with the residents staying locked for more than 30 days in some cases, leading to the loss of numerous man days. The average number of man days lost due to quarantine in the first batch was 26–28 days, whereas in the second batch, it was for 18 days and only from the three infected billets.
DISCUSSION
The cumulative incidence of COVID-19 among the recruits was found to be 8.1%. This number is higher than the national average of of 6.12%[6] at the time of recruitment (July and August 2020). This finding is in consensus with several studies that cite a marginally higher incidence in the youth of the country[7] and in general globally.[8] The high incidence can be attributed first to the travel during the surge of cases in the country followed by secondary infections in the institutional setting. The incidence here is, however, much lower than that observed in a similar setting during a sleep away youth camp at Georgia where more than 50% of the 627 attendees of ages 14–20 years were affected (attack rate 56%) during June 10–July 1, 2020.[9]
The place wise distribution of cases in these recruits from different parts of the country was at variance with the national data[10] where Karnataka had higher number of cases than Haryana and Rajasthan during the period. Uttar Pradesh with the 4th highest number of cases in the country is at par with our findings, whereas Karnataka with only 0.6% of the recruits turning positive projects discrepancy.[11] This aberration from the national data may be attributed to the fact that majority of recruits hailed from the North Indian states of Uttar Pradesh, Haryana, and Rajasthan and had to travel longer using public transport, while those from Karnataka had the feasibility of safer modes of travel such as self-driven cars and private transports due to proximity. While several studies have cited that air travel elevates the spread of any infectious disease and not just COVID-19,[12] a study conducted in China has reported a similar outcome with train travel as well.[13]
There was a stark difference between the two batches of recruits as regard to incidence of 10.92% versus 0.61% and corresponding SAR of 15.97% versus 5.4%. The national average of incidence at the time of the recruitment was 6.12%[6] and the average SAR between 4.6% and 49.56%.[14] As no guidelines or protocols were changed between the two batches, it could be ascribed to the place from where the recruits came; the second batch entrants came from areas geographically closer to the said Institute as opposed to the first batch who had to travel longer distance from the north of India. Better and stricter implementation of the quarantine protocols in the 2nd batch could also contribute to the above finding.
The lack of a primary case in M2 block was pondered over and it was found that M2 block was filled in the later phase of recruitment process and had mostly accommodated people from the southern parts of the country such as those from Karnataka, Goa, and Telangana as the dates given to the recruits varied geographically.
From the epidemic curve [Figure 2], it can be inferred that peak rise in the curve was due to the explosive appearance of secondary cases following exposure to primary cases of the first batch of trainees itself. The second batch of trainees was accommodated in separate block without any contact with the first batch and almost all of the cases corresponding to the rise in the curve were from the first batch of recruits. The CDC has unequivocally declared a similar trend in the disease progression with the appearance of secondary cases following exposure to primary cases.[15]
The SAR among the quarantined was 15.59% against a figure of 4.6–49.56% of the national data.[14-16] In a study conducted by the Guangzhou Centre for Disease Control and Prevention, China, it was found that the SAR of COVID-19 among household contacts was at 16%.[17] Another study by ICMR has suggested an average SAR of 6%.[18] On consideration of closed environments and spread of COVID-19, the incident of the infamous cruise ship comes to mind that was stranded off the coasts of Norway and harbored 712 positive cases, with an SAR of 45%.[19] In India, a study by Laxminarayan et al. on transmission dynamics in states of Tamil Nadu and Andhra Pradesh, SAR estimates ranged from 1.2% (0.0–5.1%) in health-care settings to 2.6% (1.6–3.9%) in the community, 9.0% (7.5–10.5%) in the household and up to 79.3% in those who traveled and shared conveyances for more than 6 h.[20] In comparison, the SAR of 15.59% in this study, despite the congregated setting, can be credited to the strict quarantine, stringent adherence to preventive measures, isolation, and cohorting employed by the administration.
Among the recruits, 64.7% were symptomatic with only 7% showing moderate-to-severe symptoms, whereas 35.3% were found to be asymptomatic. These findings were in accordance with ICMR data and data from other countries which reported that a majority of the cases of COVID 19 were indeed symptomatic (72%).[21] However, a study conducted in Karnataka, the state, where the Institute is located, reported contrary findings, wherein, 91% were found to be asymptomatic.[22] This stark variation could be attributed to the fact that population in this study hailed from different places with a history of travel during the surge of cases in the country, making them more susceptible.
Regarding severity of symptoms, the findings were similar to the retrospective cohort study in the youth camp in Georgia in June 2020 where majority were mildly symptomatic or asymptomatic, that was characteristic of SARS-CoV-2 infection among younger age group.[23] The same has been corroborated in other studies too. This observation supports the policy decision for the lower order of priority given by the government for vaccination for younger age groups.
Among symptoms, fever had the maximum prevalence at 72.4% followed by GI symptoms at 8.3% and anosmia at 7.69%. A thorough review of articles that included 148 citations from nine countries cited that ILI-like symptoms with fever were the most commonly found symptom in positive COVID-19 cases with a prevalence of 78%.[24] To substantiate the prevalence of anosmia and GI symptoms in our study, a study from Pune with similar prevalence of anosmia (14.8)[25] and a systemic country wide review of GI symptoms (01/05 cases)[26] can be cited. The average duration of hospitalization among the symptomatic cases was 15 days. A study conducted in China depicted a median of 10–19 days of hospitalization for +ve COVID-19 patients.[27] A study in India on random sample of 221 cases assessed that the average duration of hospital stay in COVID-19 fell between the class interval of 16–34 days.[28] The rate of positivity of COVID-19 testing by both RTPCR and RAT in this report was at 11.44% which was greater than the national average of 8.04%[29] in the months of July and August, corresponding with the time of recruitment undertaken in our study.
While it is understood that SAR is a true estimate of the spread of the disease and that the depiction of R0 is a matter of mathematical representation and meticulous calculation, in the scope of the study, a crude estimation and depiction of the R0 could shed light on the transmission dynamics as our sample was completely closed cohorts, entire data were available with no attrition and all the contacts were presumed to be susceptible, and hence, minutely monitored. The overall R0 found among the trainees was at 2.39; greater than the national average of R0 varying between 1.73 and 1.08.[30] This swell in the number is justified seeing as the population of the study were confined to closed premises and quarantined in groups. However, it is lower than that observed in the youth camp making it evident that scrupulous surveillance and regular testing can reduce transmission even in an institutional setting.[9]
Although this study did not find substantial evidence as regard transmission from asymptomatic individuals, a study from Karnataka available as a preprint did find evidence of transmission from both symptomatic and asymptomatic cases, though the transmission was mainly driven by symptomatic cases.[31] The serial interval in our study was 7 days, similar to the mean serial interval of 6.3 observed in more than 3000 cases reported in Jodhpur district over a span of 120 days from March to July 2020.[32] The difference in numbers of the incidence, SAR, and the R0 between the first and the second batch of recruits clearly justifies the benefit of employment of good quarantine measures despite claims that quarantine in such demography could perhaps be a waste of resources.
In times of the first wave of COVID-19, when vaccination was not an option, travel and recruitment came with the additional baggage of quarantine, thence begging the question, should quarantine have been levied mandatorily in institutions proceeding with recruitment of healthy, physically tested and proven fit youngsters between the ages of 18 and 25. Considering the fact that the morbidity among them is minute if not negligible,[33] it can nonetheless be feasibly argued that they are not excused from the threats of COVID-19.[34] More so the fact that asymptomatic transmission from such healthy carriers might have infected someone in the general population with a susceptibility to advanced disease is a grave concern that begets utmost caution, especially in the absence of a vaccine during the period of the study. However, post successful execution of vaccination drive in the country, it can be deliberated whether vaccinated and healthy individuals may be exempted form quarantine on traveling from one protected area to another.
The strengths of this study lie in the fact that the population while being large was followed up in its entirety without any loss or attrition of data, thereby depicting a good estimate of the transmission dynamics of COVID-19 in a cohort of young adults in the prevaccination era. Strict quarantine and screening for symptoms for early diagnosis could control effectively control transmission. The only limitation was quarantine in a military fashion, that is, in barracks as opposed to separate rooms.
CONCLUSION
Set in times of the first wave of COVID-19 in the country, this report has successfully ensued on its objective of giving an insight into the incidence and important aspects of transmission dynamics of COVID-19 as observed in the congregate setting of an Armed Forces Training Establishment. The arrival of recruits from different parts of the country led to occurrence of primary cases followed by secondary transmission of the disease of much larger extent. The study also validates the asymptomatic/mild nature of the infection in young adults. Fair conclusion on the implication of good quarantine and isolation measures and regular surveillance for symptoms for early diagnosis has also been compellingly indicated from these observations.
What this study adds
Describes natural history of COVID-19 in young unvaccinated individuals.
The accurate observations on transmission dynamics show that introduction of COVID-19 in a congregate setting has the potential to cause explosive outbreaks, however, proper quarantine and surveillance can effectively reduce transmission.
Reiterates that COVID-19 infection among healthy young adults is essentially mild/asymptomatic with minimal proportion with severe symptoms. The risk of mortality is negligible.
Transmission from asymptomatic cases if at all is insignificant.
Travel is an important risk factor for infection with COVID-19.
Declaration of patient consent
Patient’s consent not required as partients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Worldometer. 2020. Available from: https://www.worldometers.info/coronavirus [Last accessed on 2020 Nov 20]
- [Google Scholar]
- An Introduction to Applied Epidemiology and Biostatistics. Vol 3. (3rd ed). United States: CDC; 2001.
- [Google Scholar]
- Household secondary attack rate of COVID 19 and associated determinants in Guangzhou, China: A retrospective cohort study. Lancet Infect Dis. 2020;20:1141-50.
- [CrossRef] [Google Scholar]
- 2020. Geneva: World Health Organization; Available from: https://www.who.int/docs/default-source/coronavirus/who-china-joint-mission-on-covid-19-final-report.pdf [Last accessed on 2020 Oct 27]
- [Google Scholar]
- Coronavirus Disease 2019 (COVID-19) Situation Report-73 Geneva: World Health Organization; 2020.
- [Google Scholar]
- Ministry of Health and Family Welfare. 2020. India: Government of India; Available from: https://www.moffw.gov.in [Last accessed on 2020 Oct 29]
- [Google Scholar]
- Epidemiology and transmission dynamics of COVID-19 in two Indian States. Science. 2020;370:691-7.
- [CrossRef] [PubMed] [Google Scholar]
- Changing age distribution of the COVID-19 pandemic-United States, May-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1404-9.
- [CrossRef] [PubMed] [Google Scholar]
- 2020. Available from: https://www.covidindia.org [Last accessed on 2020 Nov 04]
- Ministry of Health and Family Welfare. 2020. India: Government of India; Available from: https://www.mohfw.gov.in [Last accessed on 2020 Oct 20]
- [Google Scholar]
- Transmission of infectious diseases during air travel. Lancet. 2005;365:989-96.
- [CrossRef] [Google Scholar]
- Risk of Coronavirus disease 2019 transmission in train passengers: An epidemiological and modeling study. Clin Infect Dis. 2021;72:604-10.
- [CrossRef] [PubMed] [Google Scholar]
- Secondary attack rate of COVID-19 in household contacts: A systematic review. QJM. 2020;113:841-50.
- [CrossRef] [PubMed] [Google Scholar]
- High contagiousness and rapid spread of severe acute respiratory syndrome Coronavirus 2. Emerg Infect Dis. 2020;26:1470-7.
- [CrossRef] [PubMed] [Google Scholar]
- Secondary transmission of coronavirus disease from presymptomatic persons, China. Emerg Infect Dis. 2020;26:1924-6.
- [CrossRef] [PubMed] [Google Scholar]
- Laboratory Surveillance for SARS-CoV-2 in India: Performance of testing and descriptive epidemiology of detected COVID-19, January 22-April 30, 2020. Indian J Med Res. 2020;151:424-37.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative analysis of control measures on-board ship against COVID 19 and similar novel viral respiratory disease outbreak: Quarantine ship or disembark suspects? Med J Armed Forces India. 2020;77(Suppl 2):S430-6.
- [CrossRef] [PubMed] [Google Scholar]
- 28% of 40,184 COVID Positive cases in India Till 30 April were Asymptomatic: ICMR Study, The Print. 2020.
- [Google Scholar]
- Epidemiology of SARS-CoV-2 Infection in Karnataka State, South India: Transmission Dynamics of Symptomatic vs. Asymptomatic Infections. medRxiv 2020
- [CrossRef] [Google Scholar]
- The prevalence of symptoms in 24, 410 adults infected by the novel Coronavirus (SARSCoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries. PLoS One. 2020;15:e0234765.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of new onset anosmia in COVID-19 patients: Is the trend different between European and Indian population? Indian J Otolaryngol Head Neck Surg. 2020;72:484-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and mortality of COVID 19 patients with gastrointestinal symptoms: A systematic review and meta-analysis. Mayo Clin Proc. 2020;95:1632-48.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 2020;18:270.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 pandemic and its recovery time of patients in India: A pilot study. Diabetes Metab Syndr. 2020;14:1205-11.
- [CrossRef] [PubMed] [Google Scholar]
- Health World. 2020. Economic Times. Available from: https://www.health.economictimes.indiatimes.com/news/industry/covid-19-tests-in-india-cross9-crores-20states-uts-report-positivity-rate-less-than-national-average/78659852 [Last accessed on 2020 Nov 25]
- [Google Scholar]
- A Comprehensive Analysis of R0 with Different Lockdown Phase During COVID-19 in India. In: medRxiv. 2020.
- [Google Scholar]
- Coronavirus disease 2019 in children-United States, February 12-April 2 2020. MMWR Morb Mortal Wkly Rep. 2020;69:422-6.
- [CrossRef] [PubMed] [Google Scholar]
- Research: USCF. 2020. Available from: https://www.uscf.edu/news/2020/07/418081 [Last accessed on 2020 Nov 02]
- [Google Scholar]
- A comprehensive analysis of R0 with different lockdown phase during covid-19 in India. BMJ. 2020;10:e041778.
- [Google Scholar]
- Descriptive epidemiology of SARSCoV-2 infection in Karnataka state, South India: Transmission dynamics of symptomatic vs. asymptomatic infections. EClinicalMedicine. 2021;32:100717.
- [CrossRef] [PubMed] [Google Scholar]
- Transmission dynamics of the COVID-19 epidemic at the district level in India: Prospective observational study. JMIR Public Health Surv. 2020;6:e22678.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus Disease 2019 in Children United States, February 12-April 2. MMWR Morb Mortal Weekly Report. 2020;69:422-6.
- [CrossRef] [PubMed] [Google Scholar]
- Research: USCF. Available from: https://www.uscf.edu/news/2020/07/418081 [Last accessed on 2020 Nov 02]
- [Google Scholar]






