Translate this page into:
Hypobaric and Normobaric Hypoxia Training in Aircrew: A Comparative Study
Abstract
Hypoxia has been known to be an omnipresent physiological threat at altitude. It has forced aircrew world over to device and look for countermeasures. Simulated hypoxia in a controlled environment of Hypobaric chamber (hypobaric hypoxia) is considered as the ‘gold standard’ for Hypoxia Awareness Training. Hypobaric chamber training has inherent hazards of decompression sickness (DCS), barotrauma and loss of consciousness (LOG). An alternative method being explored is simulated hypoxia at sea level by breathing a gas mixture containing 7.7 % Oxygen (normobaric hypoxia). The GO2Altitude® one man hypoxicator used in this study to give desired hypoxic gas mixture, places a subject at a physiological altitude of 25000 ft and enables demonstration of symptoms of hypoxia. This framing is inherently safer than traditional training as it poses no threat of DCS as well as barotrauma and has better transfer of training for fast jet aircrew (mask- on hypoxia). This study was conducted to validate normobaric hypoxia (NH) training through GO2Altitude® hypoxicator by comparing it with hypobaric hypoxia (HH) training in hypobaric chamber. 23 participants were exposed to two regimens of hypoxia training: HH and NH at a simulated altitude of 25,000 ft. Subjective, physiological and psychomotor performance was assessed, analysed and compared. No significant differences in the frequency and severity of the 24 commonly reported symptoms, physiological response or in the psychomotor performance between the two training paradigms were found. NH is similar to HH in terms of the type and severity of subjective symptoms experienced by the participants, physiological response generated and effect on psychomotor performance and is comparable to HH. NH is an effective, useful and safe hypoxia training tool.
Keywords
Hypoxia
Hypobaric hypoxia (HH)
Normobaric hypoxia (NH)
Hypoxia training tool
Introduction
Hypoxia has long been recognised as a significant physiological threat at high altitude (1). An analysis of military helicopter accidents in Indian Army brought out that hypoxia may have been at least partly responsible for 24.83% of all accidents and 30.43% of all Human Factors accidents (2). Over the last decade, helicopter and unpressurised transport aircraft operations in high altitude have increased substantially in quantum (3). IAF fighter aircraft and Army Aviation have been operating from high altitude bases and advance landing grounds (ALGs). Hence, encountering in-flight hypoxia remains to be a potent threat.
Early recognition of hypoxia symptoms is important in preventing incapacitation due to hypoxia so that corrective actions can be initiated on time. The hypobaric chamber training is a well-established method of imparting hypoxia awareness training (HAT) to aircrew. It helps in early recognition of signs and symptoms due toin-flight hypoxia. However, high cost, risk of decompression sickness (DCS), barotrauma and loss of consciousness associated with hypobaric chamber training has forced most of the aeromedical training centers in the world to think of alternative methods to provide effective simulation of hypoxia on ground (4). IAF has been imparting hypoxia awareness training to its aircrew in the hypobaric chamber for more than three decades now. While there has been no documented case of DCS in the IAF, advantages of having a convenient and cost effective alternative to present practice of Hypoxia awareness training cannot be ignored.
Reduced Oxygen Breathing Device (ROBD) is one such alternative which is portable, light-weight, cost effective and easy to use and maintain. It can be useful in remotely located bases, without the need for the aircrew to report to aeromedical training centers. Aircrew can complete the hypoxia awareness training and return to their respective squadrons same day, saving time and cost. Hypoxia awareness training through ROBD is more close to operational scenario of in-flight hypoxia where aircrew gets signs and symptoms of hypoxia while wearing the mask as against chamber training where aircrew gets it on doffing the mask. In addition, in ROBD, the instructor can participate in more runs, without risking re-exposures to high altitude. This allows efficiency gains for the training organization(5).
Despite the perceived advantages and possible usage of ROBD in Indian Armed Forces, the validity of ROBD as a hypoxia awareness training tool for aircrew and its equivalence with the traditional method of training in a hypobaric chamber with hypobaric hypoxia is not well established in Indian aircrew. Though, a study comparing reduced oxygen breathing mixtures at sea level have supported the validity of this type of training in Indian aircrew (6), there is no study to validate membrane based hypoxia training system which utilizes a nitrogen concentrator to produce a gas on site with the desired low oxygen concentration (7).
The aim of the study was to compare chamber training and membrane based ROBD as hypoxia awareness training tools (HAT). The objective was to collect, analyse and compare subjective and objective data from the same cohort of subjects during exposure to hypobaric hypoxia (HH) and ROBD induced normobaric hypoxia (NH).
Material and Methods
Participants were 23 healthy subjects (male & female) who reported for various courses at the Institute of Aerospace Medicine (IAM) during the period of Oct 2011- May 2013. Inclusion criteria were healthy individuals between the age group of 20 to 40 yrs of age. Informed written consent was obtained from all the participants after fully explaining the research protocol. All the participants were questioned about their current health status and were examined for medical fitness to undergo exposure to simulated altitude and hypoxia in a hypobaric chamber. Those with any history of illness, particularly in relation to sinuses and ears, blood donation, and SCUBA diving in the preceding week, and flying above 10,000 ft in the preceding 24 h, were excluded..
Each participant was exposed to both forms of hypoxia training at the Department of High Altitude Physiology and Hyperbaric Medicine at IAM [located at Bangalore, India, at an altitude of 3000 ft AMSL]. The first hypoxic exposure consisted of HH at a simulated altitude of 25,000 ft in hypobaric chamber while the other consisted of NH through an ROBD (GO2Altitude®One-Man Hypoxicator System, Melbourne, Australia) for the equivalent altitude of 25,000 feet, with the fraction of inspired oxygen (FIO2) held constant at 7.7%. For each group of participants the two hypoxia sessions were separated by a period of at least 24 h to rule out a carry-over effect, and the circadian bias was controlled by scheduling both hypoxia sessions for each group at the same time of the day. All altitude exposure in hypobaric chamber was preceded by an ear clearance run as per standard protocol. Before commencing hypoxia exposure to 25000 ft, the participants pre-breathed 100% oxygen for a period of 30 min to minimize the risk of DCS. Although the risk of DCS is only significant during HH, the participants pre-breathed 100% oxygen for both types of hypoxia exposure to ensure standardisation. The chamber was decompressed at a rate of 3000 ft/ min. During the period of HH exposure, the participants performed the 5 min psychomotor vigilance task (PVT) continuously. The symptoms assessment on visual analogue scale (VAS) was performed at the end of the test, while the mathematical processing test (MPT) was performed at the beginning and at the end of the test. The duration of exposure was limited to a maximum of 5 min, as time of useful consciousness (TUC) at 25,000 feet is around 5 min. Once the recovery from hypoxia was complete, the chamber descended to ground level at the rate of 3000 ft/ min. The same profile was repeated with the ROBD. After both the profiles were completed by the participants, they were asked to compare their perception regarding the rate of onset, severity of the symptoms and ease and quality of training given in both the methods. The null hypothesis of the study was that there are no subjective (symptoms) or objective(psycho-physiological) differences between NH and HH.
The hypobaric chamber in which the study was conductedis an indigenous custom made for the Institute. The chamber has got two sections- Main and Air Lock chamber (MC and ALC, respectively). The MC houses 10 seats and the ALC four seats, with simulation capacity for most oxygen systems of various aircrafts used in IAF. The MC can go up to 50,000 ft and the ALC up to 100,000 ft. The chamber has provision for both manual and automated control via a central control unit (work space).
Prior to each hypoxia exposure, the participants were fitted with a standard oxygen mask assembly (Scott’s Mask) which is installed in the hypobaric chamber and was modified to fit with GO2Altitude® hypoxicator system. It was ensured that there was no mask leak while participants were being subjected to hypoxia training. The participants were instrumented for non- invasive recording of heart rate (HR) and pulse oxymetry (peripheral arterial oxy-hemoglobin saturation, SpO2) via a probe on the middle finger of the non-dominant hand. The mean minimum SpO2 and mean increase in HR were calculated and analysed using the paired two tailed t-test.
The participants were provided with a sheet of paper containing two simple mathematical problems, each containing three single digit numbers with either an addition or subtraction sign between them. The participants were asked to calculate the answer and then write it in one of the two boxes, depending on whether the answer was less or more than five. The subjects performed the MPT immediately after starting the hypoxia exposure and at the end of 5 min of hypoxia exposure. The participants practiced the PVT and MPT at least three times prior to their first exposure to hypoxia to minimize any learning effect. The results of the PVT and MPT were analysed by the paired two-tailed t-test.
Participants were asked to mark the symptoms that theyhad experienced from a list of 24 most commonly reported symptoms of hypoxia. They also marked the severity of each symptom experienced on a 10-cm linear visual analogue scale (VAS) ranging from “nil”, “mild”, “moderate not bothering”, “moderate bothering” to “severe”, which was then converted to a digital scale of 0 - 10 by simple linear measurement. This represented the symptom severity score. The group- mean symptoms severity scores for HH and NH were comparedusing a two-tailed t -test. The significance level for entire statistical analysis was set at Pd”0.05.
Results
A total of 23 participants participated in this study in which 21 were males (91.3%) and 2 were females (8.7%). 10 out of the 23 participants were pilots (43.48%) and 13 (56.52%) were non- aircrew trainees of IAM. Their age ranged from 20 - 40 yrs (mean = 27.7 ±4.1 yrs).
Reported Symptoms
The mean severity of the symptoms and the rank order for the group was similar in both conditions (Fig 1).

- Frequency of symptoms, mean severity score and their difference in HH and NH, with the ordinate showing the numerical values, and abscissa showing the symptoms.
Frequency of reported symptoms
The frequency orders of symptoms experienced by participants were similar in both the hypoxia training profiles (Figure 1 and Table 1).The group mean frequency of the reported symptoms was similar in aircrew and non- aircrew participants during HH and NH (Table 2). Figure 1 shows that general trend of number of times a symptom was reported (frequency) during HH and NH was similar as both the lines are closely following each other for most of the reported symptoms. Table 1 shows that three out of five most frequently reported symptoms are same in both the profiles.
| Frequency of symptoms (Frequency) | Severity of symptoms (Severity ± SD) | ||
|---|---|---|---|
| HH | NH | HH | NH |
| Light headed(23) | Reaction slow (22) | Light Headed (4.5 ± 1.8) | Light Headed(4.9 ± 0.6) |
| Thinking slow (21) | Thinking slow (22) | Reaction Slow(4.6 ± 1.5) | Warm (4.2 ± 1.7) |
| Reaction slow (20) | Light headed (20) | Thinking Slow (4.5 ± 1.5) | Dizzy (4.1 ±2.0) |
| Concentration off (19) | Warm (20) | Concentration Off (4.2 ± 1.4) | Concentration Off (3.8 ± 1.5) |
| Dizzy (19) | Short of breath (19) | Dizzy (3.9 ±2.7) | Reaction Slow (3.8 ± 1.8) |
| Group mean symptom, frequency | Test | Significance |
|---|---|---|
| Aircrew | HH vs NH | NS (ýtý= 0.16< t0.05(2), 23; p = 0.88) |
| Non- aircrew | HH vs NH | NS (ýtý= - 0.74< t0.05(2), 23; p = 0.47) |
| Aircrew vs non- aircrew | HH | NS(ýtý=-0.74< t0.05(2), 23;p = 0.47) |
| Aircrew vs non- aircrew | NH | NS (ýtý=- 10.62< t0.05(2), 23; p = 2.44) |
| Group mean symptom severity | ||
| Aircrew | HH vs NH | NS (ýtý = 0.81< t0.05(2), 23; p = 0.43) |
| Non- aircrew | HH vsNH | NS (ýtý = 0.39< t0.05(2), 23; p = 0.70) |
| Aircrew vs non- aircrew | HH | S (ýtý = 3.70 > t0.05(2), 23; p = 0.001) |
| Aircrew vs non- aircrew | NH | NS (ýtý = 0.82< t0.05(2), 23; p = 0.42) |
Severity of reported symptoms
Table 1 shows the five most severe symptoms in HH and NH. Four of the five symptoms are same in both the profiles and similar in severity. Mean severity scores were higher in HH for all the symptoms except for warm (DMSS: -1.11), short of breath (DMSS: -1.07), weak (DMSS: -0.11), physically tired (DMSS: -0.65), sleepy (DMSS: - 79) and headache (DMSS: -0.1). Difference in mean severity score (DMSS) line in Fig 1 shows that there are hardly any difference in HH and NH as it is straight most of the time except for the above mentioned symptoms where it is negative (more severe in NH).
Group mean severity scorn for HH was 2.72 ±1.14 (mean ± SD) whereas for NH was 2.65 ± 1.04. The difference in group mean severity score (DMSS) of HH and NH was 0.06 ± 0.5 which means that participants, on an average, recorded their symptoms higher in HH than in NH. However, this apparent difference was not statistically significant (ýtý = 0.61< t0.05, (2), 23; p = 0.55). The group mean severity of reported symptoms was similar in aircrew and non- aircrew in NH whereas, during HH, reported severity was significantly higher among aircrew (Table 2).
Physiological Data
Mean SpO2 changes
There was an initial lag in the fall of SpO2 which was more pronounced in NH in comparison to HH (Fig 2).
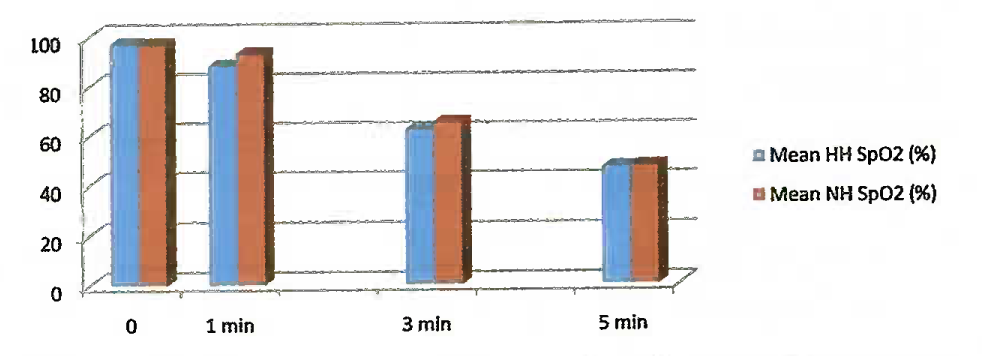
- Time course of change in Mean. SpO2 in HH and NH with ordinate showing saturation and abscissa showing time interval in minutes (0 stands for baseline)
Fall in SpO2 was more pronounced and steeper in HH than in NH, however, at the end of 5 min duration in both the exposures, minimum SpO2, attained were almost similar. The mean minimum SPO2 during the two training profiles were 46.7 ± 2.2 % in HH and 47.4 ± 1.5 % in NH. The mean minimum SpO2 during the two profiles were not significantly different (ýtý= -1.94< t0.05 (2), 22; p = 0.065). The mean drop in SpO2 in HH was 51 ± 2.30 % whereas in NH it was 50.40 ±1.0 %.The mean drop in Sp02 was also not significantly different in either profiles (ýtý=1.58< t0.05 (2), 2; P =0.129). Recovery was rapid in both the profiles as at the end of 1 min post recovery period the SpO2 returned to baseline in all the participants in both the profiles.
Fall in mean SpO2 during exposure to HH and NH was similar among aircrew, however, this drop in mean SpO2 was significantly higher than HH (51.39 ± 1.89) during exposure to NH (50.23 ± 1.83) among non- aircrew participants (Table 3). At the same time, there was no significant difference in fall in mean SpO2 among aircrew and non- aircrew participants during exposure to HH and NH (Table 3).
| Fall in mean SpO2 | Test | Significance |
|---|---|---|
| Aircrew | HH vs NH | NS (ýtý= 0<t0.05(2), 9; p=l) |
| Non- aircrew | HH vs NH | S (ýtý= 2.59 >t0.05(2), l2; p = 0.02) |
| Aircrew vs non- aircrew | HH | NS (ýtý= 0.69 <t0.05(2), 15; p = 0.50) |
| Aircrew vs non- aircrew | NH | NS (ýtý= 0.52<t0.05(2),21; p = 0.61) |
| Rise in mean heart rate | ||
| Aircrew | HH vs NH | S (ýtý= 5.36 > t0.05(2)>9; p = 0.0005) |
| Non- aircrew | HH vs NH | NS (ýtý)= 5.75 < t0.05(2),l2; p = 9.18) |
| Aircrew vs non- aircrew | HH | NS (ýtý= 0.33 <t0.05(2), 20; p = 0.74) |
| Aircrew vs non- aircrew | NH | NS (ýtý= 0.15 < t0.05 (2), 21; p = 0.88) |
Mean heart rate changes
The rise in HR was steeper and higher in HH than in NH (Fig 3), however, recovery was similar in both the cases. Mean change in HR was 37.9 ± 1.6 bpm in HH whereas in NH it was 33.3 ± 2.7 bpm. This mean change in HR was not significantly higher in HH in comparison to NH (ýtý= 8.03 > t0.05 (2),22; P =5.577).
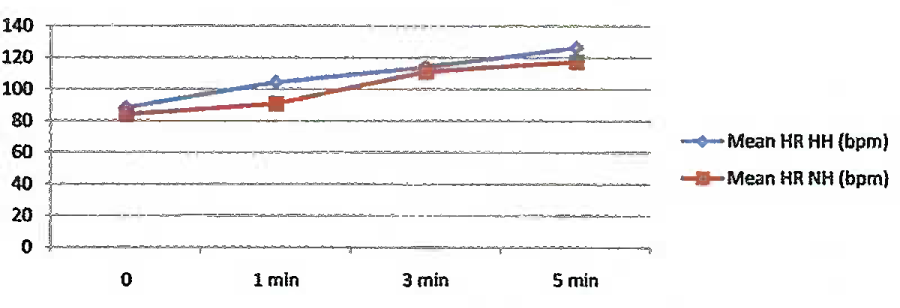
- Mean HR changes during HH and NH training profiles with ordinate showing HR in beats per minute (bpm) and abscissa showing time interval in minutes (0 stands for baseline)
Mean rise in HR among aircrew was significantly higher during exposure to HH (38 ± 1.63 bpm) than during exposure to NH (33.4 ± 2.55 bpm), however, this was not the same for non-aircrew participants. The rise in HR among non-aircrew participants was not significantly different during exposure to HH and NH. Similarly, during both the exposures rise in HR was not significantly different among aircrew and non- aircrew participants (Table 3).
Psychomotor performance
Psychomotor vigilance task monitor test: Mean reaction time
As expected, the mean reaction rime (RT) increased with the time of exposure to hypoxia. During HH, mean RT increased from 288.22 ±21.20 milli seconds (ms)to 531.22 ± 18.65ms (an 84% increase). At the same time, mean RT increased from 288.30 ± 17.52 msto 526.90 ± 14.45 ms (am 83% increase) in NH. However, the mean rise in RT during HH (243 ± 27.35 ms) and NH (238.57 ± 22.47 ms) was not significantly different (ýtý = 0.71< t0.05 (2), 22; P = 0.487).
The mean rise in RT was not significantly different among aircrew and non- aircrew participants during both the exposures (Table 4).
| Rise in mean reaction time | Test | Significance |
|---|---|---|
| Aircrew | HH vs NH | NS (ýtý= - 0.19< t0.05(2), 9; p = 0.86) |
| Non- aircrew | HH vs NH | NS (ýtý= 1.33 <t0.05(2), 12;p = 0.21) |
| Aircrew vs non- aircrew | HH | NS (ýtý= -1.35 < t0.05 (2), 21; p = 0.19) |
| Aircrew vs non- aircrew | NH | NS (ýtý= -0.32 < t0.05(2), 20; p = 0.75) |
| Rise in time to perform MPT | ||
| Aircrew | HH vs NH | NS (ýtý= -0.53 < t0 05(2), 9; p =0.61) |
| Non- aircrew | HH vs NH | NS (ýtý= -1.05 < t0.05 (2), 12; p = 0.32) |
| Aircrew vs non- aircrew | HH | NS (ýtý=-0.59 <t0.05(2), 21;p =0.56) |
| Aircrew vs non- aircrew | NH | NS (ýtý= -0.85 < t0.05(2), 16; p =0.41) |
Mathematical processing test
Mathematical Processing Test (MPT) was not a time- limited test, participant could take any amount of time to complete this task. Mean time taken to complete the task increased in comparison to MPT done at the beginning of hypoxia exposure (2.35 ± 0.57 secs in HH and 2 ± 0.52 secs in NH) and at the end of 5 min (11.57 ± 1.38 secs in HH and 11.70 ± 1.43 secs in NH ). This increase in time taken to complete the task in HH was not significantly different from the time taken to complete the task in NH (ýtý = -1.12<t0.05 (2), 22; p = 0.273). Similarly, this apparent rise in time taken to complete MPT was not statistically different among aircrew and non- aircrew members during both the exposures (Table 4).
Discussion
The 25,000 ft altitude is widely employed for hypoxia awareness training worldwide as well as at IAM, IAF as it is considered the most effective for demonstrating the effects of hypoxia and is consistent with the protocols of other investigators (8, 9). Hence, this altitude was used for HAT during HH and NH. The FIO2 of 7.7% was selected during NH because breathing an FIO2 of approximately 7.7% at 3,000 ft (altitude at which IAM IAF is located) gives an inspired partial pressure of oxygen (PIO2) equivalent to breathing air at 25,000 ft (7620 m). This is calculated to be 49 mm Hg using the equivalent air altitude model based on Dalton’s law of partial pressures after correcting for water vapour pressure (47 mm Hg at 37°C).
To achieve the desired PIO2, or hypoxic dose of 49 mm Hg at 3000 ft (where the barometric pressure is 681 mm Hg), we can calculate FIO2 by rearranging equation [1]:
Hypoxia studies have not shown any gender differences (10) and hence, participants from both genders were included in the study. The results show that the symptoms experienced by the participants were similar in both the types of hypoxia not only in frequency but also in severity. Even frequency of reported symptoms and their severity was not statistically different in both the profiles among aircrew and non- aircrew participantsexcept in HH where aircrew reported more severe symptoms than non- aircrew participants. This might prompt us to say that HAT makes a significant difference in early recognition of symptoms during subsequent exposure to hypoxia, however, this finding is intriguing as similar response is not seen during NH. The psycho - physiological parameters were similarly affected in both the hypoxia exposures and even among aircrew and non- aircrew participants except for mean drop in SpO2 which was significantly higher among non-aircrew participants during exposure to HH as compared to NH and mean rise in HR which was found to be significantly higher among aircrew during HH as compared to NH. This is difficult to explain, however, the mean difference in SpO2 was 1.08 ± 1.50 % and mean difference in rise in HR was 4.6 ± 2.72 bpm among the two exposures which doesn’t appear to be physiologically significant.
When asked to compare the two hypoxia profiles, 52% participants reported that symptoms were quicker and severe in HH whereas 48 %participants reported the same in NH. However, for the ease of administration and as an effective training tool, 70 % participants felt that NH was a better alternative and they would prefer it over HH. Out of these, 44% of the respondents were aircrew (04 transport, 01 helicopter and 02 fighters; 70% of aircrew participants). This is a significant outcome of the study as it reveals the perception of the target population (pilots) regarding both the hypoxia training tools.
Minor physiological differences, if any, are not of much relevance while evaluating various techniques of hypoxiainduction for the purpose of hypoxia awareness training (11). Ahypoxia awareness training tool should be considered valid as long as it helps an individual to experience and become familiar with the symptoms of acute hypoxia. The primary aim of hypoxiaawareness training is to encourage early recognition of hypoxia symptoms in order to enable an immediate recovery action, rather than to rely on late symptoms. From a training perspective it is, therefore, more important to show that these early symptoms are reproducible in both the training methods, as has been proved by this study. Equivalence with the time-tested ‘gold standard’ of hypoxia awareness training tool in the hypobaric chamberjustifiably validates this new tool of hypoxiaawareness training.
The ROBD is designed to demonstratemask-on hypoxia, which is a more realistic simulation of the situation prevailing in aircraft with low differential pressure or in other unpressurized cabins, where the pilotdonnes the oxygen mask throughout the flight (12). The actions required to be initiated by the pilot to recover from hypoxia during ROBD training are similar to those required in-flight. Due to these factors, NH is considered to be a more realistic and higher-fidelity training tool for fast jet aircrew. At the- same time, training in a hypobaric chamber (HH) simulates the transport and maritime patrolaircraft scenario, in which hypoxia is demonstrated bydoffing the mask at 25,000 ft, followed by arecovery action of donning the mask.
There are six major advantages of NH training over HH.
There is no risk of DCS. As a consequence, no pre-oxygenation is required, saving time and money.
Restrictions on air travel after hypobaric training in order to prevent DCS are not required (13). Therefore, aircrew can complete the hypoxia awareness training and return to their home base by air on the same day, saving time and cost.
Chamber instructors can participate in more than one run per 24 h, without risking re-exposures to high altitude. This allows efficiency gains for training organisations.
In case of a medical emergency, simply dropping the mask will terminate the hypoxia session. With HH, the cabin is at 25,000 ft at all times. In the event of a medical emergency, rapid descent may not be possible without risk of barotrauma to the participant.
Being compact and portable, an ROBD has less maintenance and operating cost. The entire system can be moved to the field and HAT can be imparted in the squadrons, under the guidance of an Aerospace Medicine specialist, who is always posted to such bases.
Even cases of questionable ear and sinus patency can undergo this training without need for ear clearance run.
Conclusion
The degrees of physiological hypoxia achieved by NH and HH at 25,000 ft appear to be similar as measured by the mean minimum SpO2 and mean change in HR during both exposures since they are not statistically significantly different. Symptom patterns and severity were also found to be similar in both exposures. Large p- values in the analysis of symptoms, physiological responses in terms of SpO2 and HR and psychomotor measures allow us to accept the null hypothesis that there is no subjective and objective difference in HH and NH. Majority of participants (16 of 23) and 70% of aircrew participants (7 out of 10) felt that ROBD was a better alternative and they would prefer it over chamber training. NH is successfully being utilised by US navy and Marine corps for refresher training of fast tactical jet aircrew (5) and by Royal Australian Air Force as a combined use of ROBD and hypobaric chamber known as CADO (Combined Altitude and Depleted Oxygen) (11) where reduced oxygen gas mixture equivalent to 25000 ft is given at simulated altitude of 10,000 ft inside the hypobaric chamber. This study further substantiates the efficacy of NH as HAT and brings out the acceptance of this training tool by Indian aircrew. Therefore, the study concludes that Normobaric Hypoxia is an effective and useful tool for hypoxia awareness training which can be employed in the IAF, especially in fields.
Recommendation
Simulated exposures to 25,000 ft for 5 min in Normobaric Hypoxia may be considered as an alternative mode for Hypoxia Awareness Training, especially in field conditions. Physiological monitoring and psychomotor tests will indicate the hypoxic status of the aircrew, while Visual Analogue Scale for hypoxia symptoms will make them understand their own hypoxia signature. Considering the cost, ease of installation, maintenance and operation of the equipment as well as availability of expertise (Aerospace Medicine specialist) for undertaking Hypoxia Awareness Training (especially Refresher training) in most of the flying stations, this can be incorporated in Indian Armed Forces in stage wise manner with minimal effort.
References
- Hypoxia and hyperventilation In: Ernsting J, Rainford DJ, Gradwell DP, eds. Aviation Medicine (4th ed). Oxford: Butterworth Heinemann; 2006. p. :41-56.
- [Google Scholar]
- Aircraft accidents in Indian Army Aviation-A general review since its inception. Ind. J Aerospace Med. 1996;40(1):7-21.
- [Google Scholar]
- Hypoxia recognition training in civil aviation: a neglected area of safety? JASAM Vol. 2010;5:4-6.
- [Google Scholar]
- TF 21-04 ROBD Feasibility Report: Using the Reduced Oxygen Breathing Device in the Naval Aviation Survival Training Program. In: Naval Operational Medicine Institute, Pensacola Florida. 2004.
- [Google Scholar]
- Cardiorespiratory and performance changes in graded hypoxia simulated with gas mixtures. Ind J Aerospace Med. 1994;38(2, Spl issue 1):32-8.
- [Google Scholar]
- Aeromedical aspects of aircrew training. Proceedings of the NATO Human Factors and Medicine Panel Worksho 14-18 October 1998. In: San Diego. CA, Neuilly-sur-Seine, France: NATO Research and Technology Organization; 1998.
- [Google Scholar]
- A closed-loop reduced oxygen breathing device for inducing hypoxia in humans. Aviat Space Environ Med. 2003;74:1190-7.
- [Google Scholar]
- Women’s health issues in Aerospace Medicine In: Davis JR, Stepanek J, Johnson R, Fogarty JA, eds. Fundamentals of Aerospace Medicine (4th ed). Wolter Kluwer: Lippincott Williams & Wilkins; p. :480-90.
- [Google Scholar]
- Hypoxia awareness training for aircrew: a comparison of two techniques. Avzrit Space Environ Med. 2010;81:857-63.
- [Google Scholar]
- Mask-on hypoxia training for tactical jet aviators: evaluation of an alternate instructional paradigm. Aviat Space Environ Med. 2006;77:857-63.
- [Google Scholar]
- The risk of developing decompression sickness during air travel following altitude chamber flight. Aviat Space Environ Med. 1990;61:1028-31.
- [Google Scholar]






