Translate this page into:
Human Engineering Assessment of a rare Musculoskeletal Disability: Sprengel Deformity
Abstract
Sprengel Deformity, a rare developmental condition, is a complex anomaly that is associated with malposition and dysplasia of the scapula.This condition also involves regional muscle hypoplasia or atrophy, which causes disfigurement and limitation of shoulder movement. This study talks about a 25 year old student pilot with the deformity of her left shoulder, who came for her DGCA Class II and Class I medicals. After ruling our complications and co-existing disabilities by thorough clinicoradiological evaluation, the functional restrictions and the extent of shoulder ROM, especially the overhead abduction (about 23% restriction), were considered to address specific aeromedical concerns related to the deformity. To confirm functionality in actual flying scenario, medical flight tests in occupational environment were desired. She was, therefore, referred to a QFI for assessment in flight simulators. After a satisfactory performance on cockpit trials on three different types of aircraft simulators (Boeing-737, Airbus-320, Cessna 152/172), she was recommended ‘fit’ to undergo training. Although, fitness to fly was justified based on her smooth and satisfactory performance, it was important to counsel her about the possible limited career prospects in the commercial civil aviation scenario.
Keywords
Sprengel Deformity
Aircrew
Civil Aviation
Fitness to Fly
Introduction
Sprengel Deformity is a rare condition of scapula in which there is failure of descent of the scapular bone during its development. It can be unilateral or bilateral. It is the most common malformation of shoulder girdle [1]. The scapula on the affected side appears to be elevated and rotated medially towards the spine due to an abrupt arrest in descent.Arrest in the development of bone, cartilage, and muscle also occurs. Some of the muscles in the region may be hypoplastic or have adhesions. The deformity is caused by an abnormal fibrous, cartilaginous, or osseous omovertebral connection of the scapula to the lower cervical vertebrae (mostly C4-C7) [2, 3]. During the organogenesis period of gestation (week 3 through 8) the scapula develops in the cervical region and then gradually descends down into the posterior thorax by third month of fetal development [2]. The reason for interruption of the descent has no satisfactory explanation [4]. Some theories have been postulated which attribute Sprengel Deformity to CSF leak through the membranes of the roof of the fourth ventricle into the adjacent tissues of the neck, increased intrauterine pressure, and abnormal articulation of the scapula to the cervical vertebrae with abnormal muscle formation[5]. The condition is sporadic, although it may, rarely, run in families (Autosomal Dominant hereditary pattern) [6, 7]. There is always an association of other conditions with Sprengel Deformity. The most common anomalies are absent or fused ribs, chest-wall asymmetry, Klippel-Feil syndrome, cervical ribs, congenital scoliosis, and cervical spina bifida.It is mainly a congenital deformity, however, there has been case report of Sprengel Deformity presenting as a post-traumatic injury [5]. Major concerns with this disability are cosmetic appearance and limitation in abduction of the affected shoulder.
The case discussed here is a 25 year old female student pilot who had come for her initial medicals at Institute of Aerospace Medicine (IAM), Bangalore. She was a case of Sprengel Deformity of the left shoulder by birth.
She was extensively evaluated at the Human Engineering department at IAM with specific assessment of her left shoulder based on the aeromedical standards laid down in current guidelines [8].
Case Report
A 25 year old female student pilot reported to IAM for her DGCA Medicals. Her left scapula appeared to be elevated and slightly rotated towards the spine. She had been asymptomatic throughout her life, and was able to carry out her routine activities without any discomfort. Antero-posterior X-ray scan was performed which showed left Sprengel Deformity, Spina Bifida of cervical region C4-C5, Dextroscoliosis, and hypoplastic ribs bilaterally (Fig 1, 2). On Examination, She was average built and well nourished. There was no problem with her gait. Locally, there was fullness of left shoulder which was elevated and internally rotated. Scoliosis was seen in spine. Functional assessment revealed restriction of range of movements of left shoulder joint. The degrees of freedom of movement measured by goniometry were given below in Table 1.

- AP views of Chest X-ray showing Elevated Scapula (Left), Dextroscoliosis and Hypoplastic ribs
| Movement | Right | Left | Normal Range |
|---|---|---|---|
| Flexion | 180° | 100° | 188 +/- 12 ° |
| Extension | 55° | 55° | 61 +/- 14° |
| Adduction | 48° | 25° | 48 +/- 9° |
| Abduction | 120° | 90° | 134 +/- 17° |
| Internal Rotation | 100 | 100 | 90 |
| External Rotation | 40 | 45 | 45 |
Results of Functional Assessment of Shoulders / Normal ranges [9]:-
Hand grip Dynamometry - Right- 22 kgf, Left - 25 kgf
Apley’s scratch test: Normal
Satisfactory racket swing and throwing motions of left shoulder
Results of Functional Assessment of Spine:-
Finger – to – Toe Distance: Forward flexion – 20 cms, Right Lateral Felxion – 34 cms, Left Lateral Flexion – 35 cms
Functional Movement Screen: 20/21 (2/3 on shoulder mobility. Satisfactory trunk stability push-ups)
The individual was unable to carry out the Apley’s scratch test, Throwing test and Racket swing test on the Left side. She could shrug her both shoulders though. Despite the restriction of motion the Orthopedic Surgeon recommended her fit to perform flying duties provided the seat of the aircraft and the controls can be adjusted to accommodate her restricted reach. For evaluation in a particular class of aircraft in which she would commence her flying training, she was referred to a qualified flight instructor on the type of aircraft for a detailed cockpit evaluation. There was a specific mention on the following aspects that were needed to be assessed in her cockpit trial:
Ability to carry out preflight checks.
Ability to ingress the aircraft, access the seat and strap up independently.
Ability to reach controls and switches to their limit of play on the left side in fully strapped position.
Ability to reach overhead and access controls and switches on the left side.
Ability to actuate controls in abnormal force environments such as hydraulic failures.
Ability to egress the aircraft as per procedure in case of an emergency.
The student pilot underwent cockpit trials on three different aircraft simulators – Boeing 737, Airbus-320, and Cessna 152/172. Her performance on all three trials was adequate and satisfactory, with the QFI commenting that only her range of overhead motion, although was slightly restricted, was likely to improve with practice. She had adequate application of force with actuation. In view of her ability to actuate aircraft controls (especially overhead switches) during simulator flying she was considered fit for flying duties in both DGCA Class II and subsequent Class I Medicals. However, it was important to counsel her about the limited career opportunities that she might get in the commercial civil aviation industry.
Discussion
Sprengel Deformity was first described in 1863. However, it got its name in 1891 after Otto Sprengel reported it with his observations. It is a result of interrupted caudal migration of the scapula. The scapula appears dysmorphic, with a convex medial border and a concave lateral border. The Scapula on the other side may also be slightly dysmorphic [10]. Other abnormalities associated with Sprengel Deformity are costal hypoplasia, synostosis, spina bifida, clavicular abnormalities, Scoliosis. Kilppel-Fleil syndrome is one of the syndromes which is found frequently in association with Sprengel shoulder and is characterized by congenital fusion of two or more of the seven cervical vertebrae [10]. These bony defects’ association explains the embryological origin of their physiopathology, as both vertebra and scapula are derived from paraxial mesoderm. However the most common association is with an omovertebral bar, even though this is not always present, which is an abnormal fibrous, cartilaginous, or osseous connection of the scapula to the lower cervical vertebrae [5, 12].
Sprengel Deformity is usually unilateral (90%), and more common in females. It is often diagnosed in early adulthood when it begins to pose a cosmetic problem on the individual. Cavendish Classification is used to differentiate the clinical grades of Sprengel Deformity (Table 2). Rigault and Pouliquen’s classification differentiates the amount by which the scapula is raised on standard radiological images (Table 3).
| Grade | Position of the medial angle of the scapula |
| Grade 1 | Between the transverse processes of T2 and T4 |
| Grade 2 | Between the transverse processes of C5 and T2 |
| Grade 3 | Above the transverse process of C5 |
| Grade 1 | Shoulders at the same level; deformity invisible when patient is dressed |
| Grade 2 | Shoulders at the same level; deformity visible when patient is dressed (lump at the base of the neck) |
| Grade 3 | Shoulders asymmetric: the affected shoulder is raised by 2 to 5 cm |
| Grade 4 | The affected shoulder is raised by more than 5 cm (superior angle close to the occiput) |
Complications of Sprengel Deformity include neonatal paralysis of brachial plexus on the affected side, Serratus anterior muscle palsy leading to winging of scapula, fascioscapulohumeral muscular dystrophy, scapuloiliacdysostosis [13]. Sprengel Deformity is often treated surgically. Some vital structures are at risk during the extensive dissection that is required as part of the relocation procedure [14]. Those with minor cosmetic deformity and minimal functional impairment need no surgery as the benefit may be minimal [15]. These structures include the dorsal scapular nerve, spinal accessory nerve, and the suprascapular nerve. Prognosis depends on the severity of the deformity, age at surgery, type of relocation procedure, and associated anomalies. Our case did not have any symptoms apart from mild restriction. She did not undergo surgery in her childhood and is leading her life actively without any physical discomfort because of her disability. During her assessment in the department of Human Engineering at IAM, certain specific aspects were looked into which would be of aeromedical concerns considering the restriction of movement in her left shoulder. The aeromedical decision making to consider her fit for flying duties was based on the following algorithm given in Fig 3.
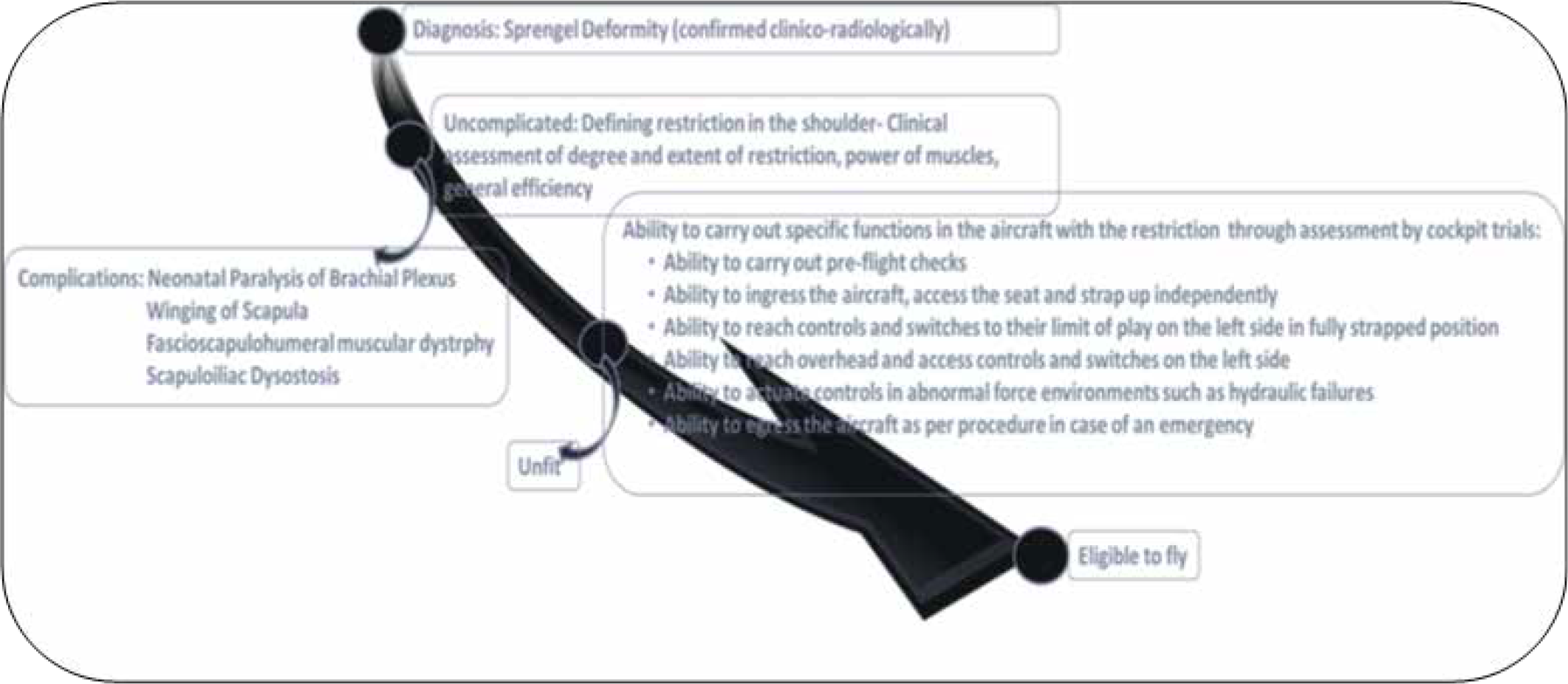
- Aeromedical Consternations of a case of Sprengel Deformity
The minimum levels of fitness to be accepted when assessing the musculoskeletal system of an applicantare detailed in the ICAO Manual of Civil Aviation Medicine, Annex 1, 6.3.2.23. The applicant shall not possess any abnormality of the bones, joints, muscles, tendons or related structures, which is likely to interfere with the safe exercise of the applicant’s license and rating privileges. Any sequelae after lesions affecting the bones, joints, muscles or tendons, and certain anatomical defects will normally require functional assessment to determine fitness. The Joint Aviation Authorities Manual of Civil Aviation Medicine states that many physically disabled pilots are able to compensate for their disability without a reduction in flight safety by a change in flying technique, a limb prosthesis, or the judicious use of assistance when on the ground. Whilst it is difficult to predict every possible problem a disabled individual may encounter when flying, or when undertaking flying-related tasks, there are some general principles which can be applied, namely:-
The pre-flight check must be accomplished adequately.
All controls must be operated safely using the aircraft modifications.
QFI should, ideally, be qualified to use any of the hand controls or devices which enables the disabled pilot to overcome his/her handicap.
In this case, despite the restriction, freedom of movements of her left shoulder was within acceptable limits for sufficient aerospace safety, in order for her to fly an aircraft in both peace and crisis situations. The disability was permanent and had reached its finality. The medical flight tests carried out revealed satisfactory performance in handling aircraft controls and operation. Although, there were no grounds based on which she could be made unfit, it was important that she understood that her career as a pilot in commercial aviation industry might not be guaranteed based on her DGCA medical clearance. The commercial airline agencies have their own laid down criteria for selection and they are within their rights not to select a pilot with such disability for their aviation duties. Therefore, she was counselled on these terms before recommending her fit in DGCA Class I Medicals.
Conclusion
This case report provides an insight into the aeromedical considerations that are to be made in evaluating a case of Sprengel shoulder with limited range of motion. Ensuring aerospace safety is of paramount importance for any aeromedical decision making and this case was no exception to the rule. Quantification and stratification of risk are desirable before justifying fitness for flying, and therefore, thorough assessment, both in human engineering aspect and cockpit trials, is important.
Acknowledgement
I am sincerely thankful to the Specialists and Staff in Department of Human Engineering IAM, IAF for their encouragement, guidance and assistance.
References
- The congenital undescended scapula. Surgical correction by the Woodward procedure. J Bone Joint Surg Br. 1983;65(5):598-605.
- [Google Scholar]
- Sprengel deformity: pathogenesis and management. J Am Acad Orthop Surg. 2012;20(3):177-86.
- [Google Scholar]
- Bilateral congenital undescended scapula (Sprengel deformity) Am J Phys Med Rehabil. 2012;91(4):374.
- [Google Scholar]
- Sprengel’s deformity. Radiology of the pathologic deformation Skeletal Radiol. 1979;4(4):204-11.
- [Google Scholar]
- Sprengel Deformity presenting as a post traumatic injury in an Afghan boy: A case report. Military Medicine. 2013;178(12):1379-83.
- [Google Scholar]
- Syndromes and disorders associated with omphalocele (III): single gene disorders, neural tube defects, diaphragmatic defects and others. Taiwan J Obstet Gynecol. 2007;46(2):111-20.
- [Google Scholar]
- Hydrocephalus, skeletal anomalies, and mental disturbances in a mother and three daughters: a new syndrome. Am J Med Genet. 1995;59(4):506-11.
- [Google Scholar]
- Human Engineering guide to equipment design In: Clifford Thomas Morgan editors (1st ed). 1963. p. :553-5.
- [Google Scholar]
- The Sprengel deformity. Morphometric analysis using 3D-CT and its clinical relevance. J Bone Joint Surg Br. 2000;82:711-18.
- [Google Scholar]
- Mutation in MEOX1 gene causes a recessive Klippel-Feil syndrome subtype. BMC Genet. 2013;14(1):1-7.
- [Google Scholar]
- Ipsilateral omovertebral bones in the levator scapulae and the rhomboid muscle in a Sprengel Deformity: A case report. Acta Orthopaedica Belgica. 1998;64(1):92-5.
- [Google Scholar]
- Developmental anomalies of the scapulathe most forgotten bone. Am J Med Genet A. 2003;120:583-87.
- [Google Scholar]
- Congenital undescended scapula (Sprengel deformity): a case study. Clin Anat. 2002;15(2):139-42.
- [Google Scholar]






