Translate this page into:
Describing the continuum from ALOC to G-LOC

*Corresponding author: Dr A Kumar, MBBS, MD (Aerospace Medicine), Department of Acceleration Physiology and Spatial Orientation, Institute of Aerospace Medicine IAF, Vimanapura, Bengaluru -560 017, Karnataka, India. ajay4757giri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar A, Nataraja MS. Describing the continuum from ALOC to G-LOC. Indian J Aerosp Med 2020;64(1):32-6.
Abstract
Introduction:
G-induced loss of consciousness (G-LOC) has been extensively investigated and pathophysiology of the same has been well elucidated in the literature. The syndrome of almost loss of consciousness or ALOC has also been described which is a loose collection of signs and symptoms of a physiological, emotional, and cognitive nature. This is believed to occur under +Gz stress which is insufficient to cause G-LOC. Institute of Aerospace Medicine IAF regularly conducts high-G training for its fighter pilots in the High Performance Human Centrifuge. Episodes of G-LOC and ALOC are unintended outcomes of such training. A study was conducted to understand the nature of these episodes in the Department of Acceleration Physiology and Spatial Orientation.
Material and Methods:
A G-LOC/ALOC proforma was designed in the Department of Acceleration Physiology and Spatial Orientation to understand the nature and causes of the G-LOC/ALOC and was filled up by the aircrew on a voluntary basis. The data were analyzed using Microsoft Excel and SPSS 20 with significance set at 95% confidence interval and alpha at 0.05.
Results:
Forty-seven aircrew experiencing G-LOC/ALOC agreed to be part of the study and filled up the proforma after the episodes. However, only 42 proforma (31 G-LOC and 11 ALOC) was found suitable for the analysis. There was no statistical difference in heart rate (HR) measured during the rate of onset and G-level at which G-LOC and ALOC resulted. There was no difference in psycho-somatic manifestations of G-LOC and ALOC episodes.
Conclusion:
ALOC and G-LOC have similar manifestations and operational implications. There is ample evidence to suggest that ALOC is a manifestation of G-LOC syndrome rather than a separate entity.
Keywords
Almost loss of consciousness
G-induced loss of consciousness
High-G training
High Performance Human Centrifuge
INTRODUCTION
Fighter flying routinely entails exposure to high-G environment which manifests in cardiovascular and neurocognitive compromise in the form of grey-out or Peripheral Light Loss (PLL), blackout or Complete Light loss (CLL), almost loss of consciousness (ALOC), and G-induced loss of consciousness (G-LOC).[1] Whinnery expanded the entity G-LOC to “G-LOC syndrome” and defined it as, “a spectrum of neuro- and psycho-physiological changes and symptoms that result from G-induced alterations in the supply of oxygenated blood to the central nervous system which includes not only the loss of consciousness but also loss of vision, loss of muscle control, convulsive activity, dreams, altered memory, and EEG alterations.”[2,3] Cammarota constructed a mathematical model based on this theory and successfully demonstrated the “G-LOC induction time (6.25 s)” similar to Rossen et al. and Beckman et al. who studied G-LOC produced after acute arrest of cerebral circulation in man and G-LOC produced by rapid onset high +Gz pulses, respectively.[4-7]
It has been argued that even if the +Gz stress is insufficient to cause G-LOC, deficits in motor and cognitive functions can still occur.[8] Thus, it is a continuum from PLL, through CLL and ALOC to G-LOC. Even though ALOC as a phenomenon has been reported extensively during centrifuge studies, there are very limited reports of ALOC as a cause of accident.[8-12] US Navy has implicated a large number of in-flight incidents of altered states of awareness to ALOC.[3,9] IAF has not reported any incidence of in-flight ALOC leading to accident.[13,14]
IAM IAF has been conducting high-G training for aircrew since March 1991 using the old centrifuge installed at the Institute in 1966. In 2009, new High Performance Human Centrifuge (HPHC) got commissioned in IAF. HPHC is being used to impart high-G training to IAF aircrew (Operational Training in Aerospace Medicine – OPTRAM) since then. Even though centrifuge training is supervised and all efforts are made to limit pilot incapacitation due to G-LOC or ALOC to a minimum, episodes of loss of consciousness do occur during such training. The aim of this study was to understand the phenomenon of G-LOC and ALOC reported during the HPHC training among the aircrew.
MATERIAL AND METHODS
The study was conducted at the Department of Acceleration Physiology and Spatial Orientation (AP & SO) at IAM IAF as a part of bigger study on analysis of G-LOC and ALOC episodes in the HPHC.[15] A “G-LOC/ALOC proforma” was designed in the Department of AP and SO which was filled by the aircrew who experienced inadvertent G-LOC/ALOC during the OPTRAM (Operational Training in Aerospace Medicine) training on voluntary basis. Analysis of +Gz training videos and filled proforma was used to collect data for the study.
Informed consent was given by all participating aircrew. The G-LOC and ALOC episode was identified by the medical operator controlling the run. The actual running of the centrifuge was controlled using a “stick” available to the pilot inside the gondola. The G-LOC was defined by the loss of consciousness and head slump (loss of postural control) and ALOC was defined by a dazed look, blank facial expression, uprolling of the eye-balls and manifestation of loss of cognitive functions (e.g., stopping AGSM) without loss of consciousness. In all cases, medical operator initiated “medical stop” at the slightest hint of aircrew showing features leading to inadvertent G-LOC/ALOC. The time of absolute incapacitation (AIP) was defined as the time from dazed/ blank facial expression, rolling of the aircrew’s eyeballs, or sudden slumping of the head or a combination of these, to the aircrew trying to purposefully raise his head from a slumped position. The relative incapacitation period (RIP) was defined as the period from the aircrew trying to raise his head from a slumped posture to the time when he gave a definite verbal response to repeated calls from the centrifuge controller.
All the filled-up G-LOC/ALOC proforma received during Jan 2018 to Jan 2019 were analyzed using Microsoft Excel™ 2010 version 14.0.4760.1000 (32 bit) and SPSS 20. Descriptive statistics were applied to analyze age, flying hours, time of the day, the incapacitation periods, the duration of the myoclonic flail movements, and G-level at which ALOC/ G-LOC occurred and G-onset rate. ANOVA was used to analyze the difference between the incapacitation periods of the aircrew during ALOC and G-LOC. Significance was set at 95% confidence interval and P < 0.05.
RESULTS
Forty-seven aircrew experiencing G-LOC/ALOC agreed to be part of the study and filled up the proforma after the episodes. However, only 42 proforma (31 G-LOC and 11 ALOC) was found suitable for the analysis. The mean age of aircrew experiencing ALOC and G-LOC was similar (26 years ±4.73 for ALOC and 26.02 years ±4.5 for G-LOC). The trend of episodes of ALOC and G-LOC was similar from trainee pilots (U/T) to senior supervisors. About 24% of aircrew experiencing G-LOC had history of G-LOC in the past whereas 33% of aircrew experiencing ALOC had experienced G-LOC in the past.
Mean flying hours of respondents for ALOC were 693.45 h (range 180 – 2400 h) and for G-LOC were 569.91 h (range 140 – 3400 h). Median time of the day at which ALOC occurred was 1156 h (range: 0915–1600 h) and for G-LOC it was 1240 h (range: 0930–1609 h). Mean G-level at which ALOC occurred was 7.5 G (SD-1.2, range 5.4– 8.9 G). Similarly, mean G-level at which G-LOC occurred was also 7.5 G (SD-1.5, range 1.44–8.9 G). Mean G-onset rate for ALOC was 3.44 ± 2.5 G/s and for G-LOC, it was 2.2 ± 2 G/s. The onset rate was not significantly different between ALOC and G-LOC (P > 0.05). Offset rate was 2G/s for all episodes as the entire run was terminated by the medical operator by pressing the “Medical Stop” button of the centrifuge.
G-LOC and ALOC syndromes were described based on the total incapacitation period (TIP) and RIP [Table 1]. The TIP for ALOC was 10.09 ± 4.9 s and for G-LOC was 12.22 ± 4.3 s. Similarly, AIP for G-LOC was 7.29 ± 2.4 s and RIP for G-LOC was 4.92 ± 3.2 s. TIP was not significantly different between ALOC and G-LOC (P > 0.05).
| Incapacitation period | ALOC | G-LOC | ||
|---|---|---|---|---|
| Mean duration (s) | SD | Mean duration (s) | SD | |
| Relative (RIP) | -- | -- | 4.92 | 3.2 |
| Total (TIP) | 10.09 | 4.9 | 12.22 | 4.3 |
The ALOC and G-LOC syndrome was studied based on their clinical manifestations as well [Figure 1]. No myoclonic jerk (flail movements) and tingling sensation in face were reported during ALOC. At the same time, myoclonic jerk with mean duration of 3.6 ± 1.14 s was reported in 22% of the G-LOC episodes and tingling sensation in the face during 6% of G-LOC episodes. Facial twitching was reported during 36% of ALOC episodes and 19% of G-LOC episodes. Loss of motor control was reported in all the episodes of ALOC and G-LOC. Tingling in extremities was reported during 36% of ALOC episodes and 13% of G-LOC episodes. Amnesia was associated with 18% of ALOC episodes and 50% of G-LOC episodes. Confusion was reported during 36% of ALOC episodes and 63% of G-LOC. There were seven episodes (22%) of dreamlets in G-LOC and two episodes (18%) in ALOC.
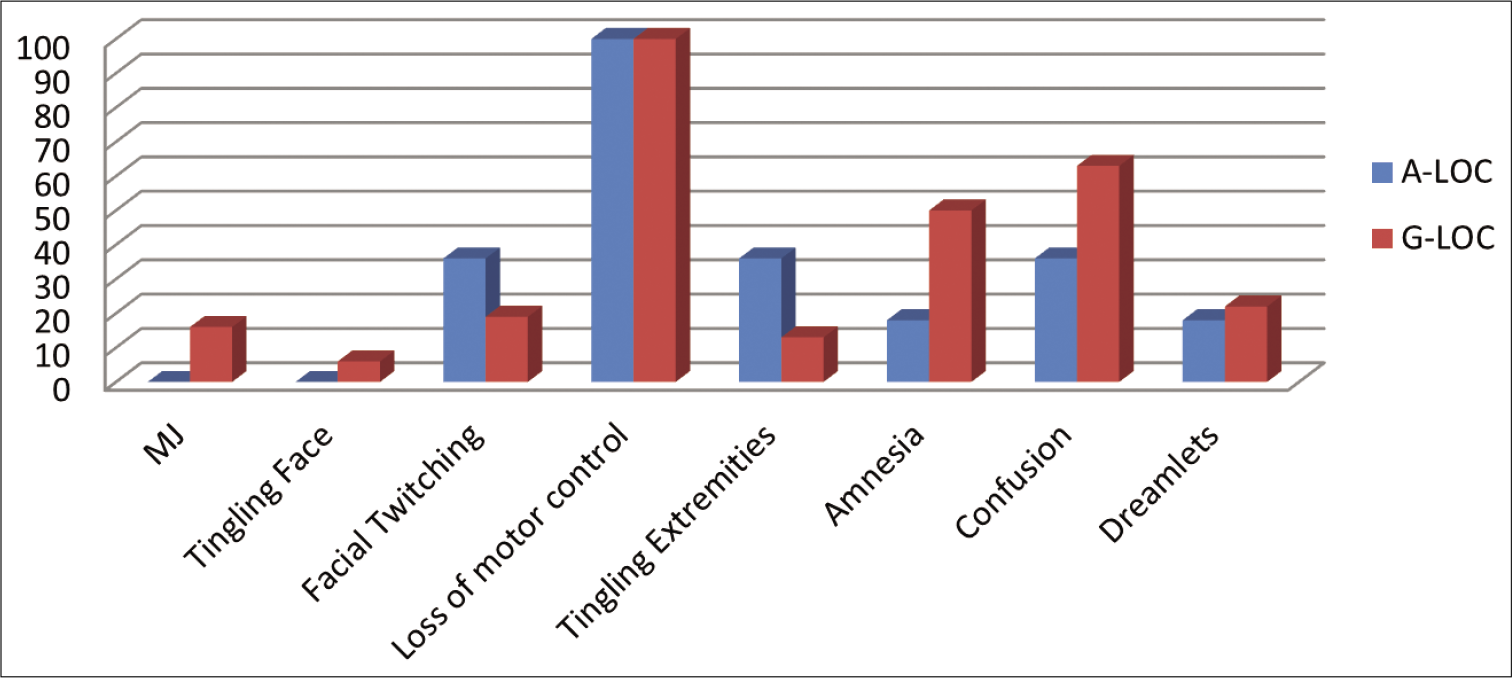
- Clinical manifestation in X-axis and percentage of reporting in Y-axis.
The only physiological parameter that was assessed during the study was heart rate [Figure 2]. Mean basal heart rate during ALOC was 109 ± 14 beats/min (bpm) and during G-LOC was 116 ± 20 bpm. Mean peak heart rate during ALOC was 199 ± 20 bpm and during G-LOC was 191 ± 21 bpm. The mean heart rate at which ALOC occurred was 178 ± 14 and at which G-LOC occurred was 168 ± 27 bpm. The mean rise in heart rate (difference in peak heart rate and basal heart rate) during ALOC was 91 ± 15 bpm and during G-LOC was 75 ± 27 bpm. The fall in heart rate (difference in peak heart rate and heart rate at which ALOC/G-LOC occurred) for ALOC was 21 ± 16 bpm and for G-LOC was 21 ± 18 bpm. One-way ANOVA was applied for all these parameters to compare ALOC and G-LOC. None of these parameters were statistically significant between ALOC and G-LOC.
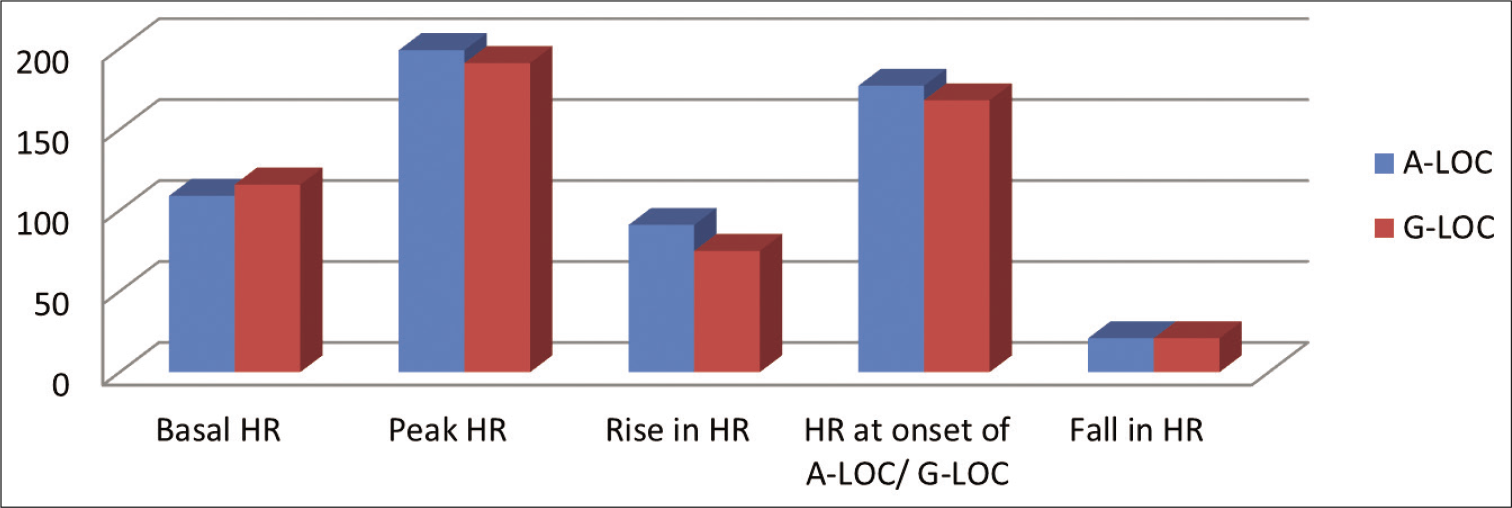
- Heart rates in X-axis and values in Y-axis for ALOC and G-LOC.
About 18% of aircrew who experienced ALOC and 16% of aircrew who experienced G-LOC reported that they had light snack before the run implying that their stomach was not full during the run.
State of anti-G Suit (AGS) during the run and quality of AGSM for all ALOC and G-LOC episodes was assessed by the medical operator and documented in the proforma. Anti-G suit was adequately tight during all episodes of ALOC. AGSM was not adequate during 50% of ALOC and 55% of G-LOC.
Figure 3 shows distribution of ALOC and G-LOC during various HPHC runs of the OPTRAM training. One proforma of ALOC did not mention the run profile. One episode of ALOC (9%) was reported during GOR (Gradual onset rate run at 0.1 G/s). No G-LOC was reported during this run. No ALOC was reported during ROR (Rapid onset rate run at 0.5 G/s), 4.5G Target Tracking (TT) and 6G TT. Mean onset rate during closed loop (Pilot in control) runs, namely, 4.5G TT was 1G/s, 6G TT was 2G/s, 7G TT was 1.82G/s, and 9G TT was 3.16 G/s. There was no significant difference between the peak G level and G-onset rates at which ALOC and G-LOC occurred (P > 0.05).
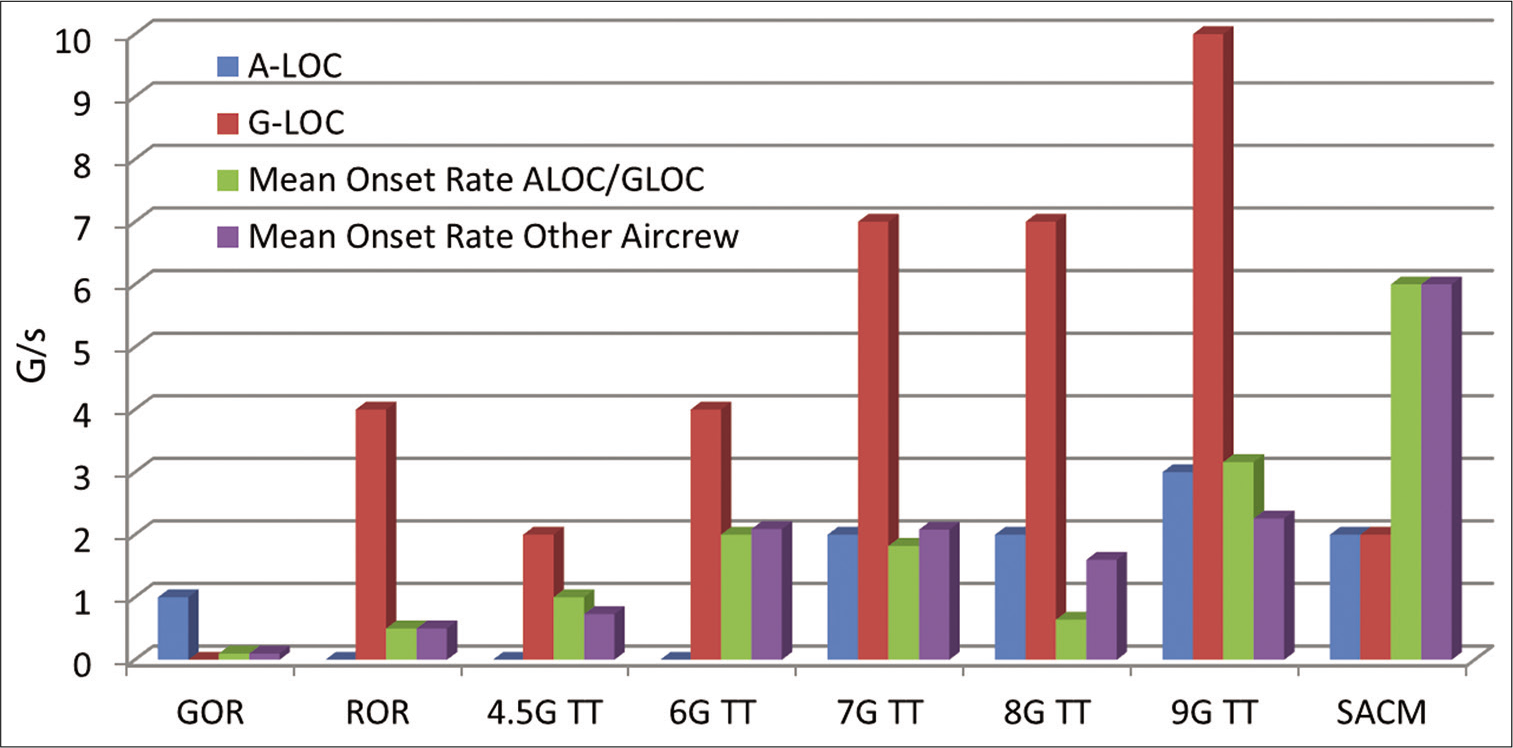
- Number of G-LOC and ALOC episodes during various OPTRAM runs with their mean G-onset rates (G/s) and mean G-onset rates for other aircrew who did not experienced it.
DISCUSSION
Psychological, somatic, and physiological manifestations of G-LOC and ALOC were found to be similar. Features of ALOC included sensory abnormalities, amnesia, confusion, euphoria, paralysis, and reduced auditory acuity. One particularly notable feature was the apparent disconnection between the desire and the ability to perform an action. Certain features (e.g. tremor, facial twitching, and tingling) were seen to persist for some time after the acceleration exposure was over. Tyagi has mentioned that incidences of ALOC during operational flying are likely to be high as it occurs at lower G-levels of shorter duration especially if it follows negative G due to Push-Pull effect.[10] However, this was not observed in our study, where the +Gz levels were seen to be the same. In an earlier study spanning over a decade of centrifuge training at IAM IAF, more than 200 episodes of G-LOC in 400 pilots have been recorded. Despite the fact that the incidence of G-LOC was more than 30%, no incidence of ALOC was reported in the study.[14]
The postulated mechanism of ALOC and G-LOC is the same; the only argument is ALOC occurs when the +Gz stress is “insufficient” to cause G-LOC.[9] However, the threshold of “this insufficient +Gz stress” is not well defined. The analysis of +Gz stress and physiological response in our study revealed that the peak G-level and the rate of onset of G at which ALOC/G-LOC occurred were not different. Further, Cammarota et al. demonstrated that once balance between oxygen supply and demand is disturbed beyond criticality, nothing can prevent subsequent loss of consciousness.[7] This was witnessed during present study as well, where G-LOC was seen in one aircrew after centrifuge had come back to baseline 1.4G. There was no significant difference in the TIPs of ALOC and G-LOC. The physiological response in terms of basal heart rate, peak heart rate and heart rate at onset of ALOC and G-LOC were also not significantly different.
The manifestations of ALOC episodes and G-LOC episodes were similar in nature as documented in the literature.[9,10,13] Dreamlets, so far, have been described as the hallmark of G-LOC. However, in our study, they were reported during two episodes (18%) of ALOC, which is not statistically different (P > 0.05) from the incidence during G-LOC (22%). Sushree has reported a lower incidence of 7% in her study of aircrew with ALOC.[16] The numbers are too small to investigate this “difference” in the incidence of ALOC.
It is our view that ALOC and G-LOC are a part of a continuum, and oftentimes the boundary between the two may be difficult to define, even in the safe and controlled environment of HPHC by an experienced operator. This may be the reason for non-reporting of a single episode of ALOC reported during 1991–2001 despite the fact that over 400 aircrew were trained during this period. Similarly, no ALOC was reported by other authors of that era.[14,17-19] This could be because ALOC had not been defined as a separate entity till then and was treated like a “mini G-LOC” as this distinction is just a matter of semantics for many researchers.[9]
The aeromedical significance of ALOC is similar to G-LOC where the neuro-cognitive symptoms experienced (ALOC) by the aircrew result in loss of situational awareness (LSA) and spatial disorientation (SD). US navy pilots have reported brief and variable episodes of confusion, amnesia, apathy, LSA, weakness, or twitching of the hands during air-combat maneuvers (ACM) which is characterized by rapid onset rates of G-loads, relatively low G levels of short duration and less than 1 G maneuvers.[9] Operational implications of ALOC and G-LOC are also similar in nature as both might result in loss of life and aircraft during similar operational condition, i.e., while pulling high G.
As per the basic principles of classification (why do we classify things?), a phenomenon may be classified as an independent entity when its features are different or cause is different or implications are different. We observed that features (manifestations) of ALOC and G-LOC are similar. The cause of ALOC and G-LOC is the same, i.e., reduction of blood supply to the CNS under high G conditions. As such the Burton’s definition of G-LOC, where he defines G-LOC as “a state of altered perception” not “state of loss of consciousness” leaves no room for any entity like ALOC.[1] Many researchers reported that ALOC may occur at lower G-levels or G-onset rates.[8,12] However, there was no difference between the rate of onset of G and G-level at which ALOC and G-LOC were reported in our study. Operational impact of ALOC and G-LOC is not different as both have potential for aircrew losing the control of the aircraft due to altered state of awareness. The authors propose that the distinction between ALOC and G-LOC may be done away with, and a single all-encompassing term of “G-LOC Syndrome” be used, to obviate confusion.
CONCLUSION
There is ample evidence to suggest that ALOC is a part of the G-LOC syndrome rather than a separate entity. There is no benefit in reporting ALOC as an independent entity and majority of the episodes might have been reported as G-LOC or many G-LOC episodes might have been reported as ALOC. Multiple terminologies such as ALOC and G-LOC have a potential to confuse the pilot as well as aeromedical community. G-LOC Syndrome is sufficient to cover all such manifestations due to the effects of high G.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent from the participants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- G-induced loss of consciousness: Definition, history, current status. Aviat Space Environ Med. 1988;59:2-5.
- [Google Scholar]
- A new look at the loss of consciousness experience within the U.S Naval forces. Aviat Space Environ Med. 1988;59:6-8.
- [Google Scholar]
- A Dynamic Percolation Model of the Central Nervous System Under Acceleration (+Gz) Induced Ischemic/ hypoxic Stress, Ph.D. Thesis Philadelphia, PA: Drexel University; 1994.
- [Google Scholar]
- Acute arrest of the cerebral circulation in man. Arch Neurol Psychiatry. 1943;50:510-28.
- [CrossRef] [Google Scholar]
- Some observations on human tolerance to accelerative stress. Phase IV. Human tolerance to high positive G applied at a rate of 5 to 10 G per second. J Aviat Med. 1954;25:50-66.
- [Google Scholar]
- The point of no return: G-LOC at low G induced by a +GZ pulse. Aviat Space Environ Med. 1997;68:631.
- [Google Scholar]
- Acceleration-induced near-loss of consciousness: The ALOC syndrome. Aviat Space Environ Med. 2003;74:1021-8.
- [Google Scholar]
- ALOC-almost loss of consciousness and it's importance to fighter aviation. Aviat Space Environ Med. 1997;68:632.
- [Google Scholar]
- A new look at the loss of consciousness experience within the U.S. Naval forces. Aviat Space Environ Med. 1988;58:6-8.
- [Google Scholar]
- ALOC: A closer look at its threat in fighter flying. Indian J Aerosp Med. 2004;48:17-21.
- [Google Scholar]
- G-related aircraft accidents in Indian air force. Aviat Space Environ Med. 2003;74:448.
- [Google Scholar]
- Centrifuge training visa-vis G-LOC incidents-an update. Indian J Aerosp Med. 2002;46:42-50.
- [Google Scholar]
- Analysis of G-induced loss of consciousness and almost loss of consciousness incidences in high-performance human centrifuge at Institute of aerospace medicine indian air force. Indian J Aerosp Med. 2019;63:3-10.
- [CrossRef] [Google Scholar]
- Physiological interpretation of almost loss of consciousness. Indian J Aerosp Med. 2019;63:28-32.
- [CrossRef] [Google Scholar]
- Centrifuge training of fighter aircrew. The Indian experience. Indian J Aerosp Med. 1994;38:84-8.
- [Google Scholar]
- G-induced loss of consciousness (G-LOC) in the Indian air force. Indian J Aerosp Med. 1992;36:1-5.
- [Google Scholar]






