Translate this page into:
Coriolis Time Intervals in prediction of outcome of Motion Sickness Desensitization Therapy

*Corresponding author: Dr HS Harshith, MBBS, Resident in Aerospace Medicine, Institute of Aerospace Medicine IAF, Vimanapura, Bengaluru - 560 017, Karnataka, India. harshith.hs@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Harshith HS, Bhattacharya U, Nataraja MS, Agarwal A. Coriolis Time Intervals in prediction of outcome of Motion Sickness Desensitization Therapy. Indian J Aerosp Med 2020;64(1):8-13.
Abstract
Introduction:
Motion sickness is a common problem faced during flying training. Aircrew with persistent motion sickness require motion sickness desensitization. Although many aircrew benefit from the motion sickness desensitization therapy (MSDT), a significant number of individuals fail to complete the desensitization program. Early prediction of desensitization program outcome would identify non-responders and help in increasing the efficiency of MSDT.
Material and Methods:
A retrospective survey of candidates who underwent MSDT at the Institute of Aerospace Medicine between 2009 and 2019 was done. Coriolis time interval (CTI) values of 28 candidates could be retrieved. Mean CTI values of the successful and unsuccessful candidates at 5 rotations per minute (RPM) were compared. Statistical analysis was done using independent t-test, binary logistic regression, and a receiver operator characteristics (ROC) analysis.
Results:
The unsuccessful group candidates (M = 14.3, SD = 8.7 s) had significantly higher mean CTI values at 5 RPM than the successful group candidates (M = 6, SD =2.3 s); t (15.09) = −3.43, P = 0.04. Logistic regression indicated that there was a significant association between the CTI values and MSDT outcome, Chi-square (1, n = 26) =12.73, P ≤ 0.001. ROC analysis revealed a statistically significant curve with a good predictive cutoff value for CTI to identify non-responders.
Conclusion:
Results indicated that CTI values are reliable indicators in predicting the outcome of MSDT. Inclusion of other parameters, both physiological and psychological, that have a good correlation with motion sickness may give us better predictive models. Such predictors will also help in better understanding of the pathophysiology of motion sickness and in formulating improved treatment modalities.
Keywords
Motion sickness desensitization therapy
Coriolis time interval
Predictors
INTRODUCTION
Motion sickness (MS) is common in student pilots and some experienced aircrew undergoing a change of role. It is a major cause for student pilots being unable to complete flying training. The incidence of air sickness (AS) during the first sortie is as high as 30–40%.[1] While most of these individuals gradually adapt to flying in three to four sorties, a significant number of student pilots fail to overcome MS and remain persistently airsick.[2,3] To continue flying, these individuals require intervention in the form of MS desensitization. They are first referred to the No. 2 Aero Medical Training Centre for AS desensitization therapy (ASDT). Candidates who fail two successive trials of ASDT are finally referred to the Institute of Aerospace Medicine (IAM) for MS desensitization therapy (MSDT).
MSDT followed at IAM incorporates a multidisciplinary approach against MS, which has four important components; the first of these is the provocative exercise therapy (PET) or Deshmukh exercises, which comprises three sets of voluntary rotation whole-body vestibular exercises designed to produce cross-coupled stimulation (CCS), under supervision; the second comprises selected yogic exercises for modulating autonomic nervous system (ANS) responses by reducing sympathetic activity; the third is progressive muscle relaxation (PMR) done under the direct guidance of an Aviation Psychologist for helping the candidates to modify their stress and anxiety responses observed during MS; and the fourth is exposure to graded provocative motion stimuli in the disorientation simulator (DISO) from 5 RPM to 25 RPM with gradual increments of 2.5 RPM/day, to allow habituation to MS.[4]
The MSDT program carries a significant failure rate despite the extensive evaluation that each candidate undergoes before commencement of MSDT. MSDT is an exceptionally labor-intensive program, requiring at least 15 days with more than 5 personnel involved.
A physiologically unsuitable candidate may eventually go on to fail MSDT and become a treatment failure, despite nearly 50–100 person working days being invested. In addition to a waste of major effort, this is extremely disheartening for both the student and MSDT trainers, who often end up with a feeling of failure, though they may have had no role in the inability of the student to complete MSDT. This could be avoided if physiologically unsuitable candidates could be identified early and would save man-hours as well as increase the efficiency of MSDT.
Many physiological parameters of the ANS (heart rate, electrodermal activity, and gastric myoelectric activity) and vestibular function (nystagmus) have been investigated to establish a correlation with MS.[5] None of them were found to be effective enough to be used as a reliable parameter to predict the outcome of MSDT in an individual. At present, coriolis time interval (CTI) is one of the parameters used for monitoring the individual’s progress during the DISO runs of MSDT. CTI is the time elapsed from the onset of head movement until the cessation of the tumbling sensation experienced by an upright subject under yaw rotation. The purpose of the present study was to evaluate the role of CTI in predicting MSDT outcome.
MATERIAL AND METHODS
A retrospective study of the physical records that were maintained at the Department of Acceleration Physiology and Spatial Orientation (AP and SO) at IAM, of the candidates who were referred for MSDT, was conducted.
During DISO runs of MSDT, the subject seated in the simulator is rotated passively in the yaw axis and is asked to make head movements in the roll and pitch axis. Eight such head movements would constitute one iteration and eight such iterations constitute one session at a specified RPM. A mean CTI value is then calculated at the end of each such session at that particular RPM.
The mean CTI values of both successful and unsuccessful candidates were collected. Statistical analysis was carried out on the data of the 5 RPM run, as it was the first RPM to which all the candidates were exposed to and it provided maximum sample size possible, as there were eventual treatment failures and dropouts at higher RPMs. In addition, any prediction at this starting RPM would give us the earliest indication of the outcome allowing for early decision-making.
Statistical tests included descriptive analysis, independent t-test to determine if there was a significant difference between the CTI scores of both the groups, binary logistic regression to assess the predictive value of CTI on MSDT outcome and finally a receiver operator characteristics (ROC) analysis to determine the cutoff CTI value to differentiate nonresponders who would eventually fail MSDT and potential responders who would complete MSDT. All statistical tests were performed using the software package SPSS v20.
RESULTS
The data of a total of 28 candidates with their mean CTI values could be retrieved from the available records, of which 14 were successful and 14 were unsuccessful. Mean age was found to be 23 ± 2.9 years with a male: female ratio of 8.3:1. Most of the candidates were student pilots, but the referred cases also included some experienced aircrew, as indicated by the higher age group [Figure 1]. The data of two candidates from the successful group had to be excluded from the analysis as their CTI values at 5 RPM were missing.
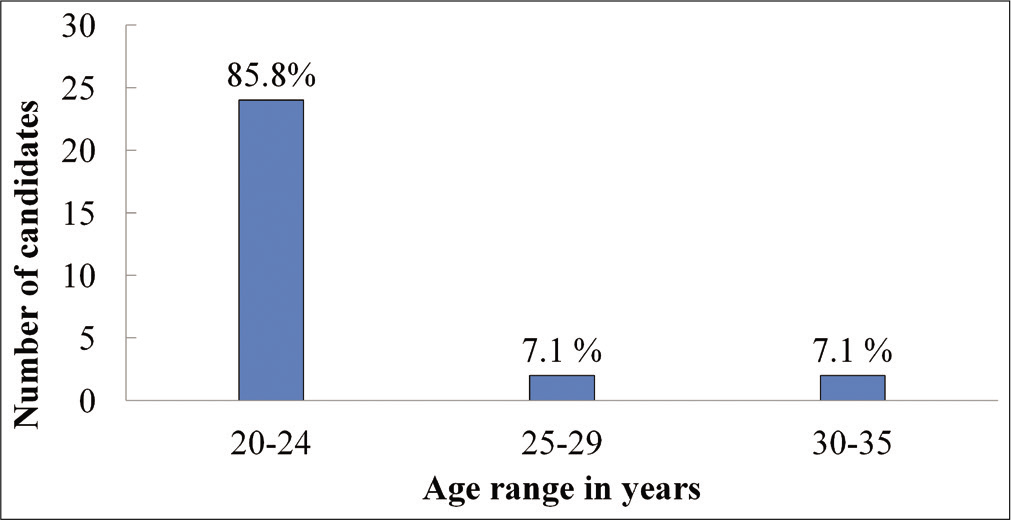
- Age distribution of the candidates.
The mean CTI values of the successful candidates ranged from a minimum value of 3.1 s to a maximum value of 9.6 s, while the mean CTI values of the unsuccessful group candidates ranged from a minimum of 4.1 s to as high as 30.9 s with their corresponding quartiles much higher than the successful group [Figure 2].
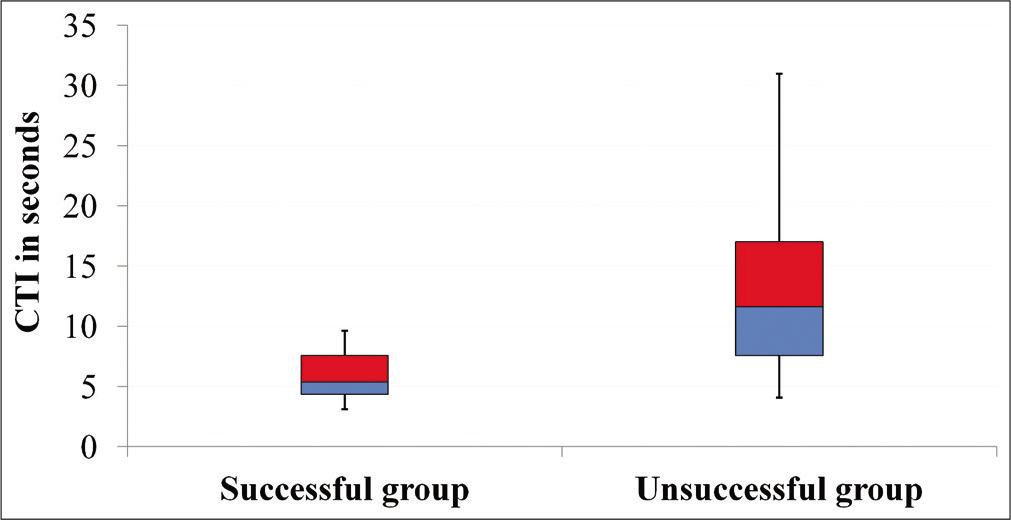
- Distribution of mean coriolis time interval values at 5 RPM of both the groups with interquartile ranges.
An independent t-test was performed to see if there was a statistically significant difference in the mean CTI values between the two groups. The unsuccessful group (M = 14.3, SD = 8.7) had mean CTI values significantly higher than the successful group (M = 6.0, SD = 2.3); t (15.09) = -3.43, P = 0.04 [Figure 3].
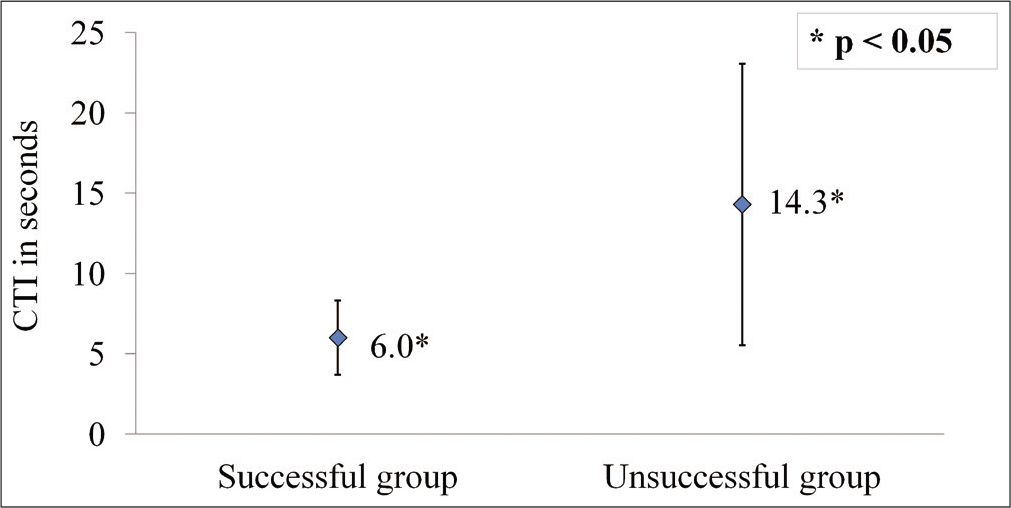
- Mean coriolis time interval values of both the groups at 5 RPM.
A binary logistic regression analysis was done to predict MSDT outcome based on the individuals’ CTI values, with the outcome as the dichotomous (successful or unsuccessful) dependent variable and the CTI values as the continuous independent variable. The results of the logistic regression indicated that there was a significant association between the CTI values and the outcome, Chi-square (1, n = 26) =12.73, P ≤ 0.001. Furthermore, the model revealed that 38.7% (Cox and Snell R squared) and 51.7% (Nagelkerke R squared) of the variability of the outcome were explained by CTI. The model was able to correctly classify 71.4% of those who were unsuccessful and 75% of those who were successful in completing MSDT, giving an overall percentage accuracy in classification of 73.1%. The beta weight for the variable CTI was found to be B = 0.426, SE =0.188, Wald =5.168, P = 0.023. The estimated odds ratio favored an increase of nearly 53% (Exp [B] =1.532, 95% confidence interval [1.061, 2.212]) for failing MSDT for every unit increase in mean CTI at 5 RPM.
A ROC analysis was performed to define a cutoff value for mean CTI at 5 RPM, with a positive test indicating individuals who would eventually fail MSDT [Figure 4]. The curve plots the true positive rate (sensitivity) against the false-positive rate (1-specificity) for each cutoff value observed in the range of the predictor variable (CTI), giving a ROC curve (the curve above the diagonal).
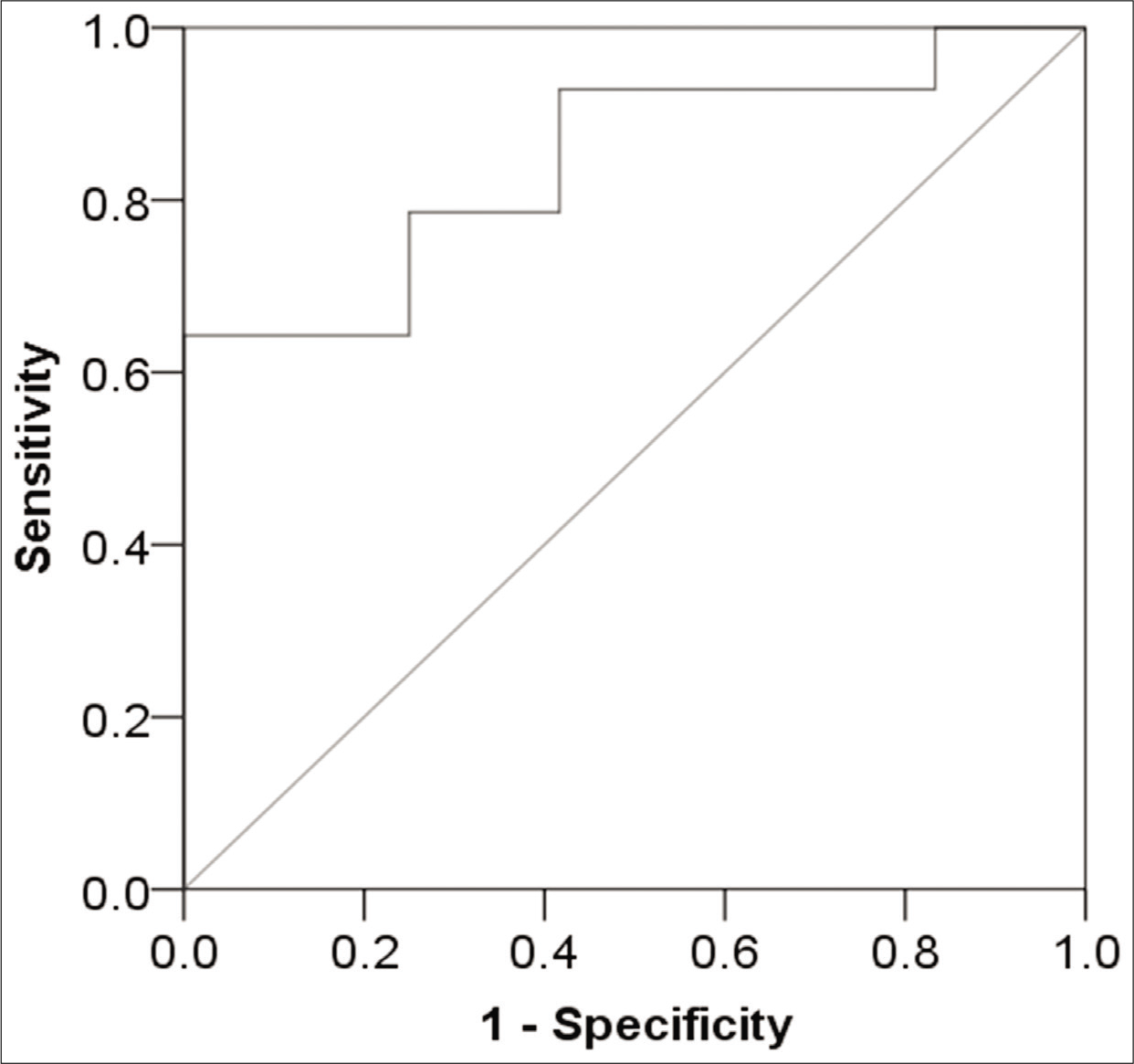
- Receiver operator characteristics curve of the 5 RPM coriolis time interval values.
The analysis revealed a statistically significant ROC curve (P = 0.003), with an area under the curve of 84.5%, indicating a good predictive value of the test. To avoid the false-positive rates, i.e., incorrectly classifying potential responders as eventual treatment failures, a safe cutoff value for the mean CTI at 5 RPM which would give the test 100% specificity was found to be at 10.5 s, with an acceptable sensitivity of 64.3%. Furthermore, this cutoff value had a positive predictive value of 100% and a negative predictive value of 70.5%.
DISCUSSION
The basic mechanism underlying the pathogenesis of MS is given by “the neural mismatch hypothesis.”[6,7] When an individual is subjected to a novel motion environment, there is a conflict between the different sensory inputs received and the expected signals of the neural store/internal model formed from the past experiences of the individual. This leads to a neural mismatch, which leads to MS. Simultaneously, the internal model is updated through necessary sensory rearrangement to allow habituation to accommodate these novel sensory information patterns. This forms the basis of MS desensitization. Through repeated exposure to provocative motion stimuli, the individual is desensitized to MS.
CTI is the subjective time interval between the onset of the head movements (done in pitch and roll axis during angular motion of the body in yaw axis) and the cessation of tumbling sensation experienced by the subject. CCS associated with the head movements during angular acceleration, leads to the simultaneous activation of more than one set of semicircular canals, producing conflicting sensory inputs. These inputs result in tumbling and nausea experienced by the subject. Physiologically, it represents the time taken by the vestibular system to adapt to the CCS and gives a fair indication of the sensitivity and adaptability of the vestibular system. As both these characteristics are important for the eventual desensitization to MS, it is logical that CTI should play an important role in MSDT.
MSDT involves a multidisciplinary approach since the etiology of MS is multifactorial. Hence, the success of MSDT also depends on the effectiveness of other interventions included in the program. PET helps in reducing the sensitivity of the candidate to MS.[1] It is capable of producing vestibular adaptation through CCS and enables the candidate to learn to control the autonomic responses when exposed to provocative stimuli.[8] Most importantly, it introduces the candidates to exercises that they may perform without any additional equipment, in case of recurrence of symptoms. During the PMR therapy, sessions done under the direct guidance of an Aviation Psychologist, the candidates are trained in relaxation and breathing exercises. The candidates are thereafter encouraged to learn to use these techniques to control their autonomic responses to provocative motion and simultaneous induction of relaxation responses to reduce anxiety to overcome MS.[1,8] The psychological state of the candidates is also regularly monitored and necessary psychological support is provided through counseling to alleviate the candidate’s anxieties about flying and their future career.[8] In addition to PET and PMR, the candidates are also subjected to practice yoga. The benefits of yogic exercises observed might be because of its effects on the ANS through the reduction in sympathetic activity. It may also be helpful in reducing the physiological and psychological stresses encountered in flying.[9] Each of the abovementioned interventions contributes to the outcome of MSDT by complementing each other’s benefits. The addition of each modality increases the success rate progressively, with a maximum rate of success achieved when administered in combination.[1,3,8]
Methods inducing CCS are used in many MS desensitization programs across the world because of its highly nauseogenic tendency which can be produced easily in a controlled laboratory environment in graded intensities.[10,11] Due to these reasons, many tests producing CCS and its associated parameters similar to that of CTI have been used in MS desensitization programs of many countries (for example, coriolis sickness sensitivity index used in Royal Air Force and coriolis stress test used in Italian Air Force) for the assessment of subject’s susceptibility to MS, their grading of this susceptibility to calibrate the magnitude of provocative stimuli, monitoring the progress, determining the benefits obtained after treatment, and even as a predictor of the treatment outcome.[10,12]
CTI has been used in MSDT and many previous vestibular studies carried out at this Institute.[5,13,14] The mean CTI values at 5 RPM found in earlier studies were found to be 10.39 ± 3.24 s[13] and 7.81 ± 4.6 s.[15] In the present study, while the CTI of the successful candidates was similar to these values, CTI of most of the unsuccessful candidates was greater. It was also found that the unsuccessful group had mean CTI values significantly higher than the successful group, indicating that they experienced the tumbling sensation/nausea for a greater duration of time, with increasing intensity of symptoms eventually culminating in vomiting and termination of the run. From the analysis, it can be inferred that individuals with mean CTI values >10.5 s in the 5 RPM run are unlikely to complete the MSDT protocol and will eventually remain as treatment failures.
This difference in CTI between the two groups can be attributed to the difference in time constant of velocity storage, a central neural mechanism that prolongs the small time constant response at the peripheral canal afferents to the long-time constant response found at the level of vestibular nuclei.[16] Velocity storage time constant is usually described in terms of the dynamic response of eye movements (vestibulo-ocular reflex) and perception in response to yaw rotations of an upright subject.[17,18] CTI used in MSDT can be considered as the time constant of the central perceptual velocity storage mechanism. Individuals with longer time constants are found to be more prone to MS than those with shorter time constants.[19,20] In fact, it is the reduction in this velocity storage time constant, either pharmacologically or through repetitive exposure to CCS, which has been implicated in the habituation to MS and reduction in MS susceptibility.[21-23]
In summary, candidates for MSDT should be reassessed after the first 5 RPM run in the DISO. If the CTI is above 10.5 s, the candidates have no chance to complete the MSDT and the attempt should be abandoned. If the CTI is below 10.5 s, there is 70% chance of a successful MSDT. These cases should be continued. This would increase the efficiency of the MSDT and prevent wastage of man-hours, unnecessary disheartening, and guilt.
CONCLUSION
The present study suggests that CTI can be used as a reliable indicator in predicting the outcome of MSDT. The cutoff is a CTI 10.5 s, above which there is a high chance of failure. Below this CTI, there is 70% chance of success, as dictated by the ROC curve.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent from the participants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Desensitisation of airsickness in trainee pilots by physical exercise therapy. Aviat Med. 1987;31:7.
- [Google Scholar]
- Airsickness in trainee aircrew of the Indian Air Force. Ind J Aerospace Med. 1995;39:9-19.
- [Google Scholar]
- Air sickness in trainee aircrew of Indian Air Force: Our experience with desensitisation. Ind J Aerospace Med. 2005;49:33-9.
- [Google Scholar]
- Motion sickness desensitiation therapy: An India experience. Ind J Aerospace Med. 2014;58:8-11.
- [Google Scholar]
- To Evaluate Efficacy of Physiological Parameters and Subjective Rating as an Adjunct to Coriolis Time Interval for Assessment of Response to Provocative Motion [Dissertation] Bangalore, Karnataka: Rajiv Gandhi University of Health Sciences; 2010.
- [Google Scholar]
- Motion sickness adaptation: A neural mismatch model. J R Soc Med. 1978;71:819-29.
- [CrossRef] [PubMed] [Google Scholar]
- Motion sickness: A synthesis and evaluation of the sensory conflict theory. Can J Physiol Pharmacol. 1990;68:294-303.
- [CrossRef] [PubMed] [Google Scholar]
- Airsickness desensitization based on physical exercise therapy: Indian Air Force Programme 1983-1993. Ind J Aerospace Med. 1995;39:9-18.
- [Google Scholar]
- Yogic exercise as a prophylaxis to reduce airsickness and morbidity in ab-initio pilot trainees. Ind J Aerospace Med. 1996;40:56-61.
- [Google Scholar]
- The desensitisation of chronically motion sick aircrew in the royal air force. Aviat Space Environ Med. 1985;56:1144-51.
- [Google Scholar]
- The Italian air force rehabilitation programme for air-sickness. Acta Otorhinolaryngol Ital. 2004;24:181-7.
- [Google Scholar]
- Rehabilitation from airsickness in military pilots: Long-term treatment effectiveness. Aviat Space Environ Med. 2013;84:1196-200.
- [CrossRef] [PubMed] [Google Scholar]
- A Study on the Effect of Alcohol on Coriolis Time Interval in IAM “AIR-FOX” SD Simulator [Dissertation] Bangalore, Karnataka: Rajiv Gandhi University of Health Sciences; 2010.
- [Google Scholar]
- Comparision of Coriolis Time Interval with Slow Phase Velocity of Nystagmus by ENG [Dissertation] Bangalore, Karnataka: Rajiv Gandhi University of Health Sciences; 2013.
- [Google Scholar]
- To evaluate the role of Cupular Adaption Time and Coriolis Time Interval in Predicting Susceptibility to Motion Sickness [Dissertation] Bangalore, Karnataka: Rajiv Gandhi University of Health Sciences; 2016.
- [Google Scholar]
- Coding of velocity storage in the vestibular nuclei. Front Neurol. 2017;8:386.
- [CrossRef] [PubMed] [Google Scholar]
- The velocity storage time constant: Balancing between accuracy and precision. Prog Brain Res. 2019;248:269-76.
- [CrossRef] [PubMed] [Google Scholar]
- Velocity storage contribution to vestibular self-motion perception in healthy human subjects. J Neurophysiol. 2011;105:209-23.
- [CrossRef] [PubMed] [Google Scholar]
- Eye movements to yaw, pitch, and roll about vertical and horizontal axes: Adaptation and motion sickness. Aviat Space Environ Med. 2002;73:436-44.
- [Google Scholar]
- Vestibular testing abnormalities in individuals with motion sickness. Otol Neurotol. 2003;24:633-6.
- [CrossRef] [PubMed] [Google Scholar]
- Baclofen, motion sickness susceptibility and the neural basis for velocity storage. Prog Brain Res. 2008;171:543-53.
- [CrossRef] [Google Scholar]
- Effects of cosmonaut vestibular training on vestibular function prior to spaceflight. Eur J Appl Physiol. 2001;85:539-45.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of vestibular training on motion sickness, nystagmus, and subjective vertical. J Vestib Res. 2007;17:227-37.
- [Google Scholar]






