Translate this page into:
Approach to a case of Eosinophilia
-
Received: ,
Accepted: ,
A 32 years old asymptomatic aircrew reported for periodic medical examination. The general and systemic examination was within normal limits. The laboratory investigations showed elevated Eosinophils (E), the differential count being E: 10% and the absolute eosinophil count was 750/cmm. The individual denied consumption of any medication and did not have any shortness of breath or wheezing. The primary issue here is the immediate fitness for flying and the secondary issue involved being evaluated for etiology.
What are eosinophils and what role does it have in the body?
Eosinophils are bone marrow-derived leukocytes whose development and terminal differentiation are under the control of several cytokines (IL-3, GM-CSF and IL-5), with IL-5 being the cytokine that is primarily responsible for eosinophilopoiesis. Eosinophils and neutrophils share a common morphology but the eosinophils are a little larger than the neutrophils and measure 12-17 µm in diameter. They usually have two nuclear lobes and the cytoplasm has distinctive spherical orange granules. The underlying cytoplasm which is usually obscured by granules is pale pink.
Eosinophils are predominantly tissue dwelling cells and express a specific chemo-attractant receptor and respond to a specific chemokine, eotaxin. They are moderately effective as a phagocyte for bacteria, yeast and protozoa but less effective than neutrophils [1]. The major function of eosinophil as a cytotoxic cell is against helminthic infections. Eosinophils can kill a wide variety of helminthic worms especially in their larval stages, by depositing cationic proteins on the surface of the parasite [2]. Conventionally eosinophils have been considered as an end-stage cells involved in host protection against parasites. Numerous lines of evidence however have now changed this perspective by showing that eosinophils are pleiotropic multifunctional leukocytes involved in initiation and propagation of diverse inflammatory responses, as well as modulators of innate and adaptive immunity. The circulating life span of eosinophil is 6-12 hrs before it migrates to tissue but unlike the neutrophils it can recirculate and have a much longer life [1].
What is the normal eosinophil count?
The normal eosinophil count is up to 600/cmm, When the levels go beyond the normal the condition is called as eosinophilia. There is considerable diurnal variation in the eosinophil count which may be as much as 100% [3, 4]. The lowest counts are found in the morning (1000h to 1200h) a time at which endogenous steroids are the lowest and the highest in the midnight (0000h to 0400h).
Hypoadrenalism is associated with eosinophilia because of low levels of endogenous glucocorticoids. It is preferable to record the absolute eosinophil count rather than as a percentage because the number depends on the total cell count.
What is eosinophilia?
Although the accepted upper limits of normal for the blood eosinophil numbers vary, a value above 600/cmm is considered abnormal and is called eosinophilia [1]. Though the eosinophils are predominantly found in peripheral tissues particularly in those tissues with a mucosal-environmental interface such as the respiratory, gastrointestinal and lower genitourinary tracts, it is normally measured by sampling peripheral blood. The degree of eosinophilia can be categorized into mild (600-1500 cells/ml), moderate (1500 - 5000 cells/ml) or severe (>5000 cells/ml) [1].
Peripheral eosinophilia can be divided into three broad categories i.e. primary, secondary, and idiopathic eosinophilia.
Primary eosinophilia is diagnosed when there is evidence of clonal xpansion of eosinophils. This usually occurs with hematologic malignancies like chronic myeloid disorders.
Secondary eosinophilia is diagnosed when eosinophilia occurs as an immunological response to an offending agent which may be infectious or non infectious. The examples of secondary eosinophilia includes tissue invasive parasite, allergic disorders, medications, toxins, autoimmune diseases, Hodgkin’s and non-Hodgkin lymphoma and endocrine disorders, like Addison’s disease.
Idiopathic eosinophilia is diagnosed when no primary or secondary cause of eosinophilia can be established despite a thorough evaluation.
Blood eosinophil numbers do not necessarily indicate the extent of eosinophil involvement in affected tissues; this is so because the cells are primarily tissue-dwelling and are several hundredfold more abundant in tissues than in blood.
Are there conditions where there is a reduction in the eosinophil count?
Reduction of eosinophil i.e. eosinopenia is associated with stress, such as acute bacterial infection and after treatment with glucocorticoids, though the mechanism is unclear. Pyogenic inflammation can thus mask the presence of eosinophilia or eosinophil-mediated inflammation. There are no known adverse effects of eosinopenia.
How common is eosinophilia?
Though the exact incidence of eosinophilia amongst aircrew is not known, it is commonly encountered in day to day practice. In our experience about 10-15% of all aircrew reporting to the Institute of Aerospace Medicine have varying degree of eosinophilia. No cases of aircrew with Hyper-eosinophilic syndrome (persistent eosinophilia defined as >1500/ml for 6 months, and organ involvement/dysfunction in which other clinical entities have been excluded) have yet been encountered.
What are the common causes for eosinophila?
The underlying cause for eosinophilia can range from benign (parasitic) to sinister (malignancy) as shown in Table 1. In a tropical country like India, the most common cause is the parasitic infestation [7, 8]. Parasitic infestation especially those with a tissue migration phase in their life cycle very commonly cause eosinophilia as reflected in Table 2. Eosinophils play an important role in mediating the antibody dependent damage to helminthes and modulating Type I hypersensitivity reaction. The eosinophilic response to parasitic infection depends on the duration of exposure with shorter duration of exposure (travelers) having more eosinophilia compared to longer duration (residents of endemic area who no longer have eosinophilia). In most cases, stool examination can provide vital inputs, especially so in cases of ascarid and hook worm infestation (Table 1 & 2)
| Parasitic conditions Allergy/atopy: asthma, urticaria, eczema, allergic rhinitis, angioneurotic oedema Reactive eosinophilia: T-cell lymphoma, B-cell lymphoma, acute lymphoblastic leukemia Eosinophilic leukemia Idiopathic hyper eosinophilic syndrome Atopy & allergic drug reactions: aspirin, penicillin, cephalosporin, nitrofurantoin, sulfonamide, iodides. Collagen vascular diseases: rheumatoid arthritis, eosinophilic fasciitis, allergic angiitis. Sarcoidosis Skin diseases: pemphigus, dermatitis herpetiformis, erythema multiforme |
| Strongyloidiasis: Strongyloides stercoralis Liver fluke: Fasciola hepatica Hydatid disease: Echinococcus granulosus. Filariasis: Wuchereria bancrofti, Onchocerciasis, Brugia malayi, Loa loa. Schistosomiasis: Schistosoma hematobium, S mansoni, S japonicum. |
In developed countries the most common etiology for eosinophilia is seasonal and perennial rhinitis, hay fever, asthma and allergic drug reaction [9]. Most asthmatics, especially those with intrinsic asthma have eosinophilia at some time in their illness [10]. In allergic rhinitis and hay fever, eosinophil count varies with the seasonal exacerbation of the pathology. A variety of drugs have been implicated as a cause for eosinophilia as shown in Table 3. In cases of drug induced eosinophilia, cessation of the offending drug causes termination of the eosinophilia.
| Aspirin Gold compounds Allopurinol Nitrofurantoin Sulfa agents Non steroidal anti inflammatory agents Bleomycin Methotrexate Tolbutamide Semi synthetic penicillins |
Eosinophilia is present in up to 1% of patients with malignancy and is a consequence of IL-5 produced by the tumor cell lines. It is present in 10% of patients with lymphoma, 3% of patients with carcinoma lung and occasional patients with cervical, gastrointestinal, renal and breast cancer. Most are asymptomatic. However, those with marked eosinophilia (> 5000/cmm) can develop shortness of breath and wheezing.
It is pertinent to note that tropical infections like amoebiasis, leishmaniasis, leprosy, enteric fever, malaria, giardiasis and tapeworms other than cysticercosis are not associated with eosinophilia.
What is hyper-eosinophilic syndrome?
Hyper-eosinophilic syndrome (HES) is a group of heterogeneous disorders many of which remain ill-defined and are characterized by persistent eosinophilia (defined as >1500/mL for 6 months) and organ involvement/dysfunction in which other clinical entities have been excluded).
The most dramatic hyper-eosinophilic syndromes (50,000- 1,00,000/cmm) are as follows:-
Tropical pulmonary eosinophilia
Idiopathic hyper eosinophilic syndrome
Loeffler’s syndrome
Loeffler’s endocarditis
Eosinophilic leukemia
Tropical pulmonary eosinophilia is a classic example of occult filiariasis and predominantly affects adult males. The syndrome is characterized by nocturnal, paroxysmal cough, hyper-eosinophilia (AEC 3,000-50,000/cmm) and elevated ESR. The levels of eosinophils are not related to the severity of symptoms. 15% of individuals with this ailment have extra pulmonary manifestations in the form of mild- moderate splenomegaly, lymphadenopathy and hepatomegaly. Chest X-ray shows diffuse miliary lesions or increase in bronchovascular marking and serology shows high titers of filarial antibodies. If untreated the condition may progress to chronic pulmonary fibrosis.
Idiopathic hyper-eosinophilic syndrome is a heterogeneous group of disorders characterized by prolonged idiopathic eosinophilia, tissue infiltration and organ system dysfunction. The bone marrow, heart, central nervous system, gastro intestinal tract, lungs, kidneys and skin may be involved to variable extent. Glucocorticoids, hydroxyurea and interferon-á have been used successfully for the treatment.
Eosinophilic gastroenteritis is characterized by infiltration of any part of the gastrointestinal tract. It affects both the sexes and usually presents in the 3rd to 5th decade. 20% of the patient may not have peripheral eosinophilia. When the disease involves predominantly the mucosa, patients may present with nausea, vomiting, malabsorption, and protein loosing enteropathy. When it predominantly involves the muscle layer, patients present with features of obstruction whereas, when it involves the subserosal layer, the consequence is ascites. Most of the patients respond to steroids and only a few of them require azathioprine.
What are the aeromedical implications of this condition?
In a majority of the aircrew the eosinophilia is mild and the individual asymptomatic; the condition therefore does not pose any significant aviation risk. Eosinophilia however is associated with increased predisposition to bronchoconstriction which manifests as shortness of breath, cough, chest tightness and wheezing. The same is apparent on clinical examination and if required a pulmonary function test can be performed to rule out obstructive lung disease. The presence of obstructive lung disease in aircrew even in a pressurized aircraft has the potential to cause sudden incapacitation and hence it becomes imperative to evaluate and document the absence of this pathology.
Evaluation for end organ damage may be required in cases of persistent moderate to severe eosinophilia or if there is a strong clinical suspicion for the same. At times the presence of eosinophilia may be the first clue to underlying serious pathology.
How do we approach a case of eosinophilia?
The extent of investigation required for patients with mild to moderate eosinophilia remains controversial with some advocating aggressive approach while others a more laid back approach. The suggested evaluation protocol which is being followed at the Institute of Aerospace Medicine includes a comprehensive history, physical examination and goal directed relevant investigations. The dictum while planning investigation is to avoid going on a “fishing expedition” by ordering needless laboratory tests, rather confining to the common etiology first. The evaluation includes -
- Evaluation protocol for aircrew with raised eosinophil counts
History: A comprehensive history directed towards symptoms, if any, and possible underlying etiology is obtained. Past history of eosinophilia, travel, and history of medication and diet (for allergies associated eosinophilia) often provide relevant clues. Use of supplements, herbal preparations, vitamins and steroids in the past is also to be obtained.
General and systemic examination with special attention paid to skin, soft tissue, lungs, liver and spleen.
-
Investigations: The investigations include the following:-
Complete blood count (CBC) and absolute eosinophil count (AEC).
Stool examination: For ova and parasites of Strongyloides, Hookworm, Fasciolopsis buski and Clonorchis sinensis. At times in cases of mild infestation multiple stool examinations may be required.
Serological tests: May be required for aircrew with tissue or blood-dwelling helminthic infections especially when the stool examination is negative. These include Trichinella, Echinococcus, Wuchereria bancrofti, Toxocara canis and Schistosoma.
Urine sedimentation: For suspected Schistosoma haematobium and in the setting of chyluria due to Wuchereria bancrofti.
Sputum analysis: For suspected pulmonary infection with Strongyloides or Paragonimus.
Studies to assess organ function: liver, renal & pulmonary function tests, urinalysis, chest radiograph, and electrocardiogram may be required in a few cases. At times bone marrow aspirates and biopsies may be required to assess fully the nature of the process underlying the high-grade eosinophilia. Assessment of focal defects due to the diverse cause for eosinophilia (Fasciola hepatica can cause focal hepatic lesions, Coccidioidomycosis fungal infection can cause focal lesions in the lung, Hodgkin or non-Hodgkin lymphoma can cause lymphadenopathy in the abdomen) may require CT scan of the lungs, pelvis, abdomen and brain.
Cystoscopy: Aircrew, who frequent Africa and have eosinophilia with haematuria, should have their urine examined for the eggs of Schistosoma haematobium. At times to establish the diagnosis a cystoscopy may be required.
How do we treat such a case?
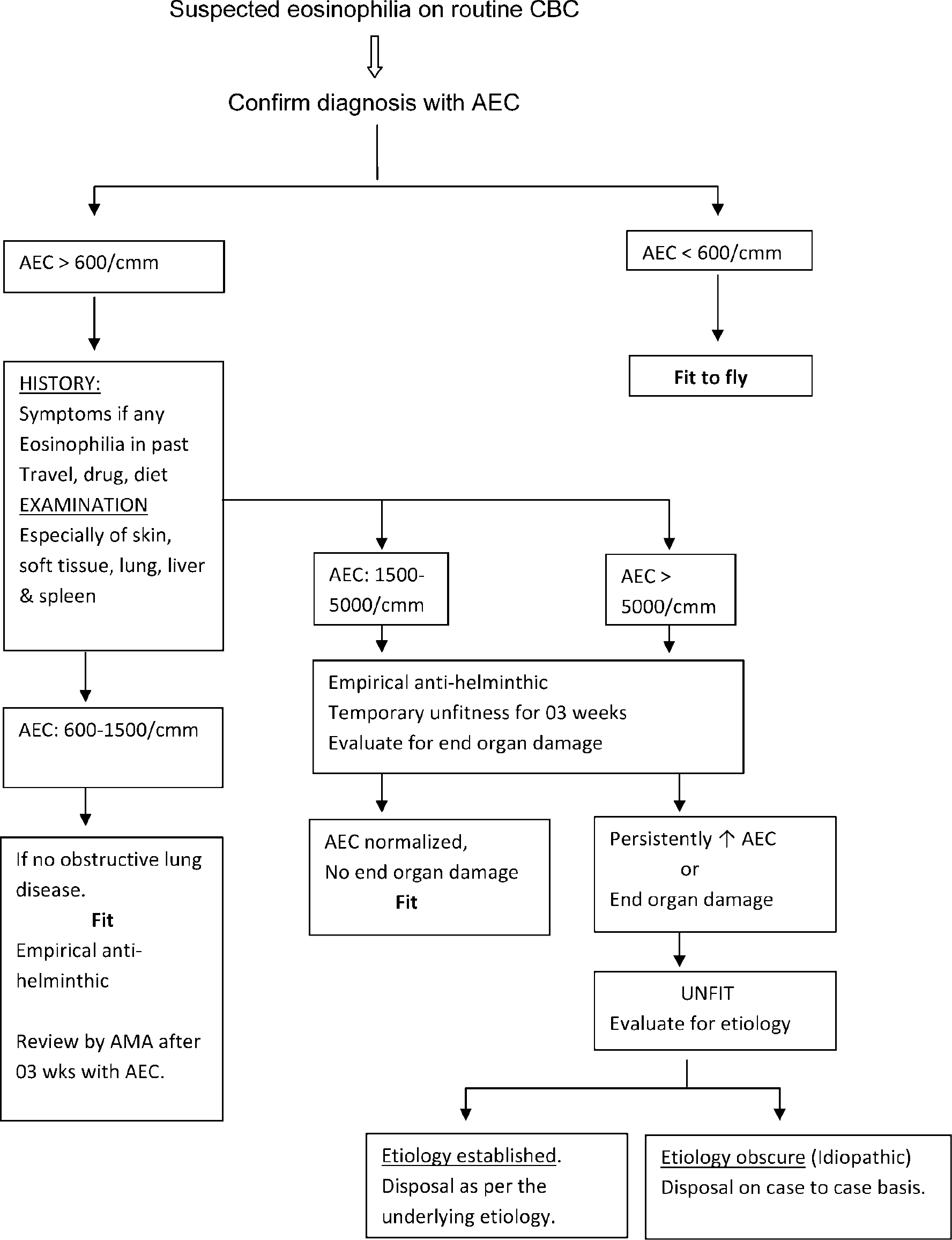
The optimal management of the asymptomatic traveler or immigrant with eosinophilia is still debated. Studies indicate that up to 50 % of patients never have a cause of their eosinophilia identified despite exhaustive evaluation [11]. Others have suggested a strategy of using empiric anti-helminthic therapies on the basis of cost-effectiveness [12]. In the Indian context considering the paucity of time available for evaluation in an aircrew and the hygiene standards we follow empirical anti-helminthic policy. The evaluation and treatment protocol followed at IAM is depicted in Table 4.
References
- Eosinophils in the 1990s: New prespective on their role in health and disease. Postgrad Med J. 1994;70(826):536-52.
- [Google Scholar]
- The number of circulating eosinophils: Normal figures and spontaneous variations. Acta Medica Scandinavica. 1958;160:99-104.
- [Google Scholar]
- Blood eosinophilia: A new paradigm in disease classification, diagnosis, and treatment. Mayo Clin Proc. 2005;80:75.
- [Google Scholar]
- Evaluation of the common conditions associated with eosinophilia. J Clin Pathol. 1985;38(3):305-8.
- [Google Scholar]
- Screening for schistosomiasis, filariasis, and strongyloidiasis among expatriates returning from the tropics. Clin Infect Dis. 1993;17:353.
- [Google Scholar]
- The cost effectiveness of strategies for the treatment of intestinal parasites in immigrants. N Engl J Med. 1999;340:773.
- [Google Scholar]





