Translate this page into:
A Preliminary Study of 24 Hour Ambulatory BP Monitoring in Clinically Normotensive IAF Personnel with Simple Obesity
Abstract
Obese personnel (BMI > 30kg/m2) in the Indian Air Force are evaluated and monitored for co-morbidities like Dyslipidemia, IGT and Diabetes Mellitus based on established biochemical and metabolic parameters. Whereas Hypertension, another known co-morbidity amongst the obese, is largely taken as absent based on a normal clinical BP recording. It is known that obese individuals have prevalence of higher nocturnal BP and a greater frequency of blunted nocturnal BP fall (‘non-dipping pattern’), which is linked to worse cardiovascular prognosis. Ambulatory blood pressure measurement (ABPM) is shown to be superior to clinical BP measurement in various clinical settings. Therefore this preliminary study was carried out with the aim to assess the utility of ABPM as an early warning tool for presence of hypertension among obese IAF personnel who are otherwise clinically normotensive. 24-hour ABPM of 14 subjects and 11 controls was analysed on various parameters. Our results highlight the presence of higher 24 hour BP load in about half (43%) of the subjects. Other parameters were beyond threshold in only 20% of them. The paper discusses the results of present study in light of ABPM diagnostic criteria of American heart association and Australian ambulatory blood pressure monitoring consensus committee. The findings and statistical analysis indicates that there is a significant effect of the BMI being less or more than 30 on the MAP. The analysis also indicates that a study with larger sample is required to establish the utility of ABPM in assessment of obese personnel.
Keywords
Obesity
Hypertension
Ambulatory blood pressure monitoring
Nondipping status
BP load
Introduction
Obesity is a modifiable risk factor for hypertension, which in turn is a major cause of cardiovascular morbidity and mortality globally. Obese individuals not only display higher BP levels than non-obese in the normotensive range but also exhibit higher levels of office as well as ambulatory blood pressure (ABPM). In IAF obese personnel are maintained under medical surveillance and monitored in low medical category. They are periodically screened for comorbidities like Dyslipidemia, IGT, Diabetes Mellitus, Hypertension. The absence of hypertension in these obese cases is determined by a normal clinical recording at the time of medical examination/ medical board. There is evidence that prevalence of hypertension in obese personnel is higher than in the normal population. It is possible that a single clinical BP reading may or may not be able to establish the pre-hypertensive / hypertensive status in a given obese case. It was hence postulated that markers of hypertension on 24 hr ABPM may be a better assessment tool than a single clinical reading of BP. If that be proven, 24 hr ABPM could prove to be a better standard assessment tool for obese personnel.
Review of Literature
In IAF, obesity is defined based on four physical parameters viz. deviation from Ideal body weight, Body Mass Index (BMI), Waist Hip Ratio (WHR) and Waist Circumference. The highest values of any of these parameters determine the grade of obesity [1]. Cases with BMI of > 30 Kg/ m2 and / or weight deviation of more than 3 Standard deviation values from the ideal mean for age and sex are placed in low medical category.
The risk estimates from the Framingham Heart Study suggest that about 75% cases of hypertension in men and about 65% in women are directly attributable to obesity [2]. The association between obesity and hypertension has been reported by many investigators using cross-sectional and longitudinal study designs, though the strength of this association varies among different racial and ethnic groups [3]. Nonetheless, it is important to emphasize that any elevation in BP above optimal levels will increase an individual’s risk of developing cardiovascular diseases (CVD) [4]. Starting at 115/75 mmHg, the CVD risk doubles with each increment of 20/10 mm Hg throughout the BP range [5].
The combination of obesity, Hypertension and other cardiovascular risk factors significantly increases the probability of adverse cardiovascular outcomes, and raises considerations for aggressive treatment strategies [6]. Another important issue in obese subjects is an increase in nocturnal BP and a greater frequency of a blunted nocturnal fall in BP (a non-dipping pattern) [7]. This is even more important in terms of cardiovascular prognosis as it has been demonstrated that both nocturnal hypertension and a blunted nocturnal BP fall are linked to a worse cardiovascular prognosis [8, 9]. Obese patients are found to have increased ambulatory blood pressures (ABPM) and increased prevalence of isolated office hypertension and non-dipping status, which emphasizes the importance of ABPM in them [10, 11]. The target organ damage (TOD) associated with hypertension is more strongly correlated with ABPM than with clinic blood pressure measurements. There is a stronger relationship between left ventricular hypertrophy (LVH) and 24-hour ambulatory systolic blood pressure than clinic or casual systolic blood pressure [12]. Despite this data the newer NICE guidelines have brought out that there is a paucity of studies comparing utility of clinical single BP recording vis-a-vis ABPM recordings and have recommended a need for ABPM based research to determine the efficacy of ABPM over single clinical reading. [13]
Deciding what constitutes normal versus abnormal ABPM is controversial, but commonly accepted normal values for ABPM in adults are less than 135/85 mmHg during the day [5,14,15,16], less than120/75 mmHg during the night [5,14,16], and less than 130/80mmHg for 24 hours [15,16]. The American heart association (AHA) considers a value of less than120/70 mmHg as normal mean night time BP [15]. The Australian ABPM Committee, in addition, recommends that in normotensive individuals the daytime and night time BP load should not exceed 20%, which implies that not more than 20% of ABPM values should be above threshold values. The Australian recommendations also specify that mean night time versus daytime ABPM measurements (nocturnal dip) should not be less than 10% [16].
Aims and Objectives
Based on the above literature a preliminary study was planned with the aim to study if 24 hr ABPM is a better tool to assess presence of concomitant Hypertension in obese personnel (with BMI > 30 Kg/m2 and / or weight > 3SD) than a single clinical BP reading. The objective of the study was to examine if introduction in the IAF of 24 hr ABPM would increase the sensitivity of detecting Hypertension in obese personnel and should be added as a standard testing protocol. A supplementary aim of the study was to assess the efficacy of the additional Australian criteria of diagnosing hypertension vis-a-vis the US criteria viz. > 20% abnormal readings and < 10% nocturnal dip.
Materials and Methods
Age matched healthy male normotensive IAF ground personnel of an operational airbase were enrolled for this study on voluntary basis. They were identified as normotensive based on two separate BP measurements of less than 135/85 mmHg with a calibrated mercury sphygmomanometer after a 5- minute rest in a sitting position.
They were divided into 2 categories, ‘Subjects’ and ‘Controls’. The ‘Subjects’ were obese IAF personnel with BMI ≥ 30Kg/m2. Those with BMI ≤ 25Kg/m2 were designated as ‘Controls’.
A 24 hr ABPM was obtained using ‘Oscar2 AccuWinPro’, an automated noninvasive oscillometric device manufactured by Sun Tech Medical Instruments, Inc, US. The ‘AccuWinPro’ software was used to upload study protocol and to download ABPM data. It was programmed to register BP at 30-minute intervals during awake hours (kept as period from 0600hrs to 2200hrs) and at 45 min interval during asleep hours (period from 2200hrs to 0600hrs). Thus for every subject and control maximum of 32 readings in the day and 10 readings at night. All the subjects were instructed to maintain their usual activities between 0600 hrs to 2200 hrs and to rest and sleep between 2200 hrs to 0600 hrs. They were also instructed to minimize movements at the time of BP recording.
At the end of 24 hr recording, a report was generated by computer interface with the device. The report was considered valid when at least 32 of 42 (76% or more) BP recordings were successful and at least one BP measurement occurred per hour.The report so generated included the following 5 values:-
Mean 24 hour BP (threshold kept at BP 130/ 80 mmHg)
Mean daytime BP (threshold kept at BP 135/85 mmHg)
Mean night time BP (threshold kept at BP 120/75 mmHg)
% SBP load (percentage of values above threshold Systolic BP)
% DBP load (percentage of values above threshold Diastolic BP).
From the values mentioned at (a), (b) and (c) above, the Mean Arterial pressures (MAPs) for 24 hr, daytime and night time were calculated. % Nocturnal dip in SBP, i.e. a variation in mean awake & asleep SBP was also calculated.
Data Filtering: A single spiky reading above threshold that did not fit in with the overall trend was considered as an aberrant reading. Such occasional aberrant readings are a known problem with ABPM and occur because of excessive arm position related pressure on the cuff, motion by the subject during recording etc. Such aberrant readings were identified and filtered out.
Statistical Analysis: The filtered data from the subjects and the controls was analysed for statistically significant differences using the unpaired ‘t’ test in respect of % SBP load, % DBP load, MAP - 24 hr, MAP – Daytime, MAP – Night time and % Nocturnal dip. A correlation analysis was also carried out for the subjects’ data between their BMI with % Nocturnal dip, % SBP load and % DBP load. Effect of waking status (sleeping vs awake) and the BMI (<30 Kg/m2 vs >30 Kg/m2) on the MAP was studied using a two way ANOVA.
Results
A total of 29 normotensive IAF ground duty personnel participated in the study. Among them 14 subjects and 11 controls completed the study protocol. Therefore for the purpose of analysis 14 subjects and 11 age-matched controls were considered. The mean age of ‘subjects’ was 40.4 ± 4.38 yrs (range 35 yrs –51 yrs) and their mean BMI was 31.9 ± 2.4 Kg/m2 (range 30.1 Kg/m2– 36.5 Kg/m2). The mean age of ‘controls’ was 39.4 ± 4.7 yrs (range 34 yrs – 49 yrs) and their mean BMI was 24.6 ± 1.6 Kg/m2 (range 23.2 Kg/m2 – 24.7 Kg/m2).
The mean 24 hr BP, mean daytime (awake) BP and mean night time (asleep) BP were within threshold limits in all the subjects.
About 43% (n = 6) subjects had 24 hr BP load (both systolic and diastolic) higher than the threshold value in 20% of the readings. Among them about 36% (n = 5) subjects had 24 hr BP load higher than the threshold value in 30% of the readings. Independently, 57% (n = 8) subjects had SBP load and DBP load more than the threshold values. [fig 1 & 2 refers]. A reduced nocturnal dip, that is less than 10% fall in systolic BP during sleep, was noted in about 20% subjects (n=3), [fig 3 refers].
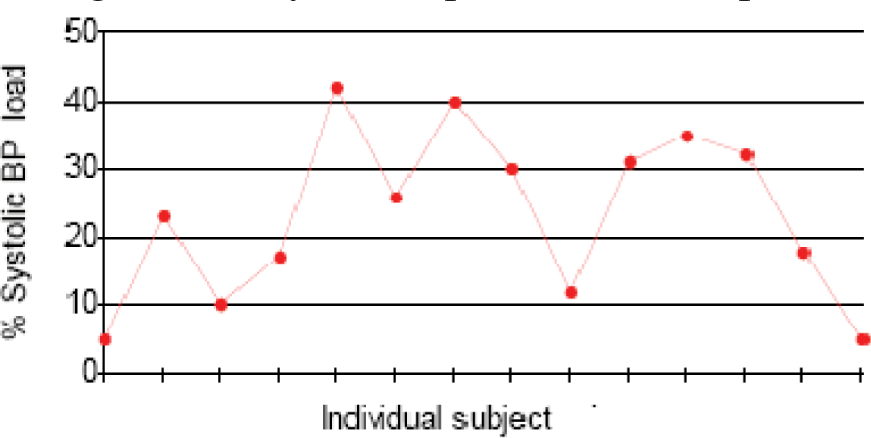
- % of Readings in individual subjects with Systolic BP Values above Threshold
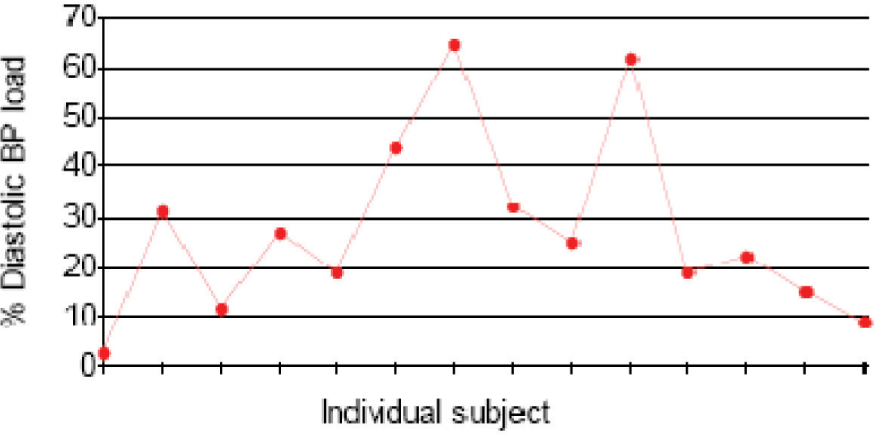
- % of Readings in individual subjects with Diastolic BP Values above Threshold
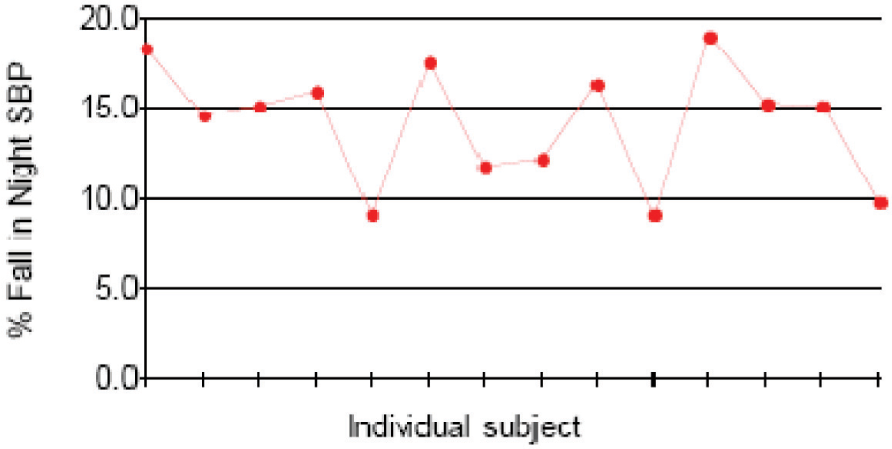
- Nocturnal Dip (in SBP) % in individual Subjects
The observed differences between % nocturnal dip, %SBP loads and %DBP loads between the subjects and controls were statistically not significant by the unpaired ‘t’ test. (p values 0.34, 0.45 and 0.20 respectively). The observed differences between MAP - 24 hr, MAP – Daytime, MAP – Night time were also found to be statistically insignificant. (p values 0.28 , 0.17 and 0.23 respectively)% Nocturnal dip showed highly significant negative correlation with BMI (coefficient of Correlation of -0.75, p=0.002).
A Two way ANOVA for the effect of waking status (sleeping vs awake) and the BMI (<30 Kg/ m2 vis-a-vis >30 Kg/m2) on the MAP was carried out. It yielded F= 152.9, p = 0.0001 and F=3.67. p=0.0011 respectively indicating that both wakefulness status and BMI affect MAP significantly. The residual error or interaction effect is very low.
Discussion
As per WHO ‘World Health Statistics 2012’, more than 2.8 million people die each year as a result of obesity and its related co-morbidities, and raised blood pressure is responsible for about 12.8% of all global deaths [17, 18]. Because obesity is a major risk factor for essential hypertension, rising BP and its associated co-morbidities will continue to impact human health and have economic consequences. Obesity and hypertension are thus important public health challenges which underline the need for effective preventive, diagnostic, therapeutic and monitoring strategies for various population groups and subgroups.
For evaluation of elevated blood pressure, the use of 24-hour ABPM in clinical setting has been gaining acceptance for a number of reasons. First, clinic blood pressure measurements often overestimate a patient’s baseline blood pressure value in up to 32% of patients. Second, 24 hour ABPM provides a means of delineating circadian variations in blood pressure. An additional benefit of ABPM is in determining what percentage of the day blood pressure is elevated above predefined normotensive values (i.e. blood pressure load). Therefore, a patient’s overall blood pressure status can be assessed more comprehensively with 24-hour ABPM than with clinic blood pressure measurements. Role of 24 hour ABPM is well established in variety of conditions like evaluation of White Coat Hypertension, suspected isolated office hypertension, autonomic dysfunction, drug-induced orthostatic hypotension, episodic hypertension, or resistant hypertension but its usefulness in the evaluation of BP status among obese for early detection of hypertension is not clearly documented.
In our study all the subjects had mean 24 hr BP, mean daytime (awake) BP and mean night time (asleep) BP within widely accepted threshold limits. In at least 6 subjects more than 20% readings were above the threshold, in 8 subjects more than 30% readings were above threshold and in 3 subjects there was reduced nocturnal dip. All these subjects hence could be labelled as Hypertensive according to Australian recommendations.
In this study, the variance within groups was found to be high especially in the control group. Considering a physiological phenomenon like blood pressure, affected by a variety of short and long term regulatory effects, the natural variation in the population is high. The small sample size in this study was therefore a drawback in being unable to show statistically significant effects when considering obesity status or awake sleep status alone.
The highly significant (p=0.001) negative correlation (coefficient of Correlation = -0.75) between % Nocturnal dip and the BMI implies that, as the BMI increases, the % nocturnal dip decreases, a fact which is widely reported and also found in our sample population. This aspect is not brought about in the‘t’ test between controls and subjects for nocturnal dip. Therefore though the study is limited by its sample size, it can be concluded from the above that individuals with higher BMI would have a lesser nocturnal dip till a critical range where the Australian criteria for <10% Nocturnal Dip would be met. The lack of correlation for average 24 hr MAP, average awake MAP or average asleep MAP is indicative that single office readings may not be a good screening tool for identifying hypertension in the obese.
The two way ANOVA shows that the status of wakefulness has a significant effect on the MAP. This is a well established fact. It was also found that there is a significant effect of the BMI being less or more than 30 on the MAP. There seems to be minimal interaction effect of BMI on difference between waking and asleep MAP. This means that if BMI of the individual has the same effect on MAP, irrespective of whether he is awake or asleep.
When assessed purely as per AHA guidelines (threshold of 120/70 mm Hg for the average ABPM during day, night and 24 hrs) all the subjects in the study were found to be normal. They would thus be labelled as ‘Simple Obesity’. However on applying additional Australian criteria (< less than 10% nocturnal dip in SBP and > 20% SBP or DBP readings above threshold of 120/75 mmHg) a few subjects were found to be hypertensive. Based on this the Australian ABPM committee criteria appear more robust for identifying obese, early hypertensive patients although this study could not categorically bring out this aspect statistically.
The findings of the study strongly suggest that the ambulatory BP rather than single office/ clinic readings is likely to be more sensitive in identifying obese individuals with early hypertensive status. This study is however unable to comment upon the specificity of such 24-hour ABPM
Since obese personnel in IAF are monitored monthly for their body weight, so, in light of the finding of higher BP loads among them in this study, it is prudent to include clinical BP recording at each such monthly review till the time results from a large sample based ABPM studies among clinically normotensive obese are available. The decision regarding the usefulness of 24 hr ABPM as a screening tool in monitoring of obese personnel in IAF needs further study.
With this it can be concluded that people with higher BMI need to be evaluated for hypertensive status since higher BP loads is known to correlate with end organ damage. The sample size of this study is not enough to comment upon the extent of the effect and thus a larger trial with greater power needs to be conducted to quantify such effects.
Limitations of the study
This was a preliminary exploratory study and the data collection had to be completed within 1 month. It was conducted in the field at an operational flying base with limited number of available obese subjects. It hence could study only a small sample. The gender based inferences could not be drawn since all subjects, serving IAF air warriors, were males. The mean daytime and mean night-time BP was determined from ABPM recordings in the predefined period. Although the subjects were advised to avoid any excessively strenuous activity and stick to routine duties the uniformity of activity among subjects could not be tightly controlled. Being a field study, some of the other variables affecting BP such as diet (salt intake), weather effects, duty schedules etc. could not be controlled.
Conclusions and Recommendations
The study reveals evidence that in obese patients ABPM, rather than a single office/ clinic BP reading, is likely to be more sensitive in identifying early hypertensive status, although a larger sample needs to be studied before making any conclusive and statistically backed recommendations. A multi centric research project is recommended to be conducted based on the trends seen in this study. The Australian recommendations for interpreting abnormal ABPM appear to be more sensitive.
References
- Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987;16:235-251.
- [Google Scholar]
- Does Waist-Hip Ratio Matter? A Study in Rural India. WHO Regional Health Forum. 2005;9(2):28-35.
- [Google Scholar]
- Obesity and hypertension: two epidemics or one? Am J PhysiolRegulIntegr Comp Physiol. ;286:R803-R813.
- [Google Scholar]
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (2003) NIH Publication No. 03- 5233 Dec: 3. Accessed on 30 Mar 13 at http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf
- [Google Scholar]
- The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2007;25:1105-1187.
- [Google Scholar]
- Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466-72.
- [Google Scholar]
- Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156-61.
- [Google Scholar]
- Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183-9.
- [Google Scholar]
- Impact of Obesity on 24-Hour Ambulatory Blood Pressure and Hypertension. Hypertension. 2005;45:602-607.
- [Google Scholar]
- Blood Pressure Monitoring, Task force III. Target organ damage, morbidity and mortality In: Blood Press Monit. Vol 4. 1999. p. :303-317.
- [Google Scholar]
- Hypertension. Clinical management of primary hypertension in adults NICE clinical guideline 127 Aug 2011 Pp 34. Accessed on 30 Mar 13 at http://www.nice.org.uk/nicemedia/live/13561/56008/56008.pdf
- [Google Scholar]
- ‘Vascular Hypertension’. Chapter 10 pg 1553 in 2nd vol, in Harrison’s principles of Internal Medicine. (17th ed). Published by McGraw Hill;
- [Google Scholar]
- American heart association recommendation for the upper limit of normal ambulatory blood pressure in adults, Table 1. Hypertension. 2008;52:433-451.
- [Google Scholar]
- Ambulatory blood pressure monitoring, position statement. 2002. MJA. 176:588-592. Accessed on 30 Mar 13 at http://www.heartfoundation.org.au/SiteCollectionDocuments/Hypertensionguidelinesambulartory-blood-presure-monitoring-Position-statement.pdf
- [Google Scholar]
- World Health Statistics 2012. 2012. World Health Organisation publication. Accessed on 30 Mar 13 at http://www.who.int/gho/publications/world_health_statistics/EN_WHS2012_Full.pdf
- [Google Scholar]
- World Health Statistics 2012: One in six adults obese, one in three hypertensive,one in 10 diabetic. Accessed on 30 Mar 13 at http://health.india.com/news/world-health-statistics-2012-one-in-sixadultsobese-one-in-three-hypertensiveone-in-10-diabetic/.
- [Google Scholar]






