Translate this page into:
A pilot study of bone scintigraphy in the evaluation of spinal injuries in aircraft accidents
Abstract
Earlier studies have shown that 26-30% of successful ejections result in spinal injuries. Currently, the protocol for evaluation of spinal injuries includes immediate X ray of the whole spine followed by CT/MRI within six weeks. This protocol not only fails in dating the trauma - whether recent or old - but also, is not sensitive enough to pick up minor traumas such as contusions of the vertebral bodies. Bone Scan (BS) carried out in such cases provides information concerning both these aspects of bone injury. The present work is based on the evaluation at IAM of 18 ejections in which bone scan was carried out in addition to X-ray and CT/MRI examination. The study revealed that in two cases there were additional injuries, which had evaded detection during earlier examination, and in two other cases the injury detected by CT/MRI was found to be due to previous trauma and not caused by the present ejection. The studies strongly suggest that bone scanning be incorporated as a necessary part of the standard protocol in the evaluation of ejection spinal injury.
Keywords
Ejection Spinal Injuries
Bone Scintigraphy
CT/MRI
Ejection is the only available means of safely abandoning a disabled high-speed aircraft. The abrupt acceleration forces involved commonly lead to abnormal and excessive loading of the spine leading to various patterns of bony and soft tissue injury [1,2]. Approximately 26-30% of all ejected aircrew sustain some kind of spinal injury [3, 4] and as a policy all of them are immediately subjectell to X-Ray of the whole spine and evaluated at IAM with CT/MRI six weeks later. In some of these cases the evaluator faces considerable dilemma in recommending the disposal since the X-ray, and CT/MRI findings are at variance with regard to the type and level of spinal injuries. The situation is further compounded when the X-Ray is negative for bone injury but the CT/MRI shows signs of injury or vice-versa or when the radiological findings are positive for some bony injury of spine but the individual is absolutely asymptomatic, which does occur in about 20% of simple compression fractures. In these cases there is an inescapable need to ascertain whether the radiological findings are chronologically matching the ejection or preexisting due to some previous impacts/injuries. Some of these injuries may have been of a minor nature or even due to high and sudden Gz loads causing bony spinal injuries which has been documented in high-performance fighter aircraft [5]. Bone scan in cases of ejection injuries could provide very useful clues with regard to the probable date of injuries and provide invaluable help for appropriate and more objective disposal of these cases. Bone scan could also help in detecting and ruling out occult injuries of the complete spinal column.
The information revealed by a bone scan in addition to the anatomical information obtained from CT and MRI could therefore help in the realistic evaluation and early reflighting of trained aircrew. This study was undertaken with a view to evaluating the overall clinical utility in detecting, managing and disposing ejection injuries of the spine.
Material and Methods
Pilots reporting to IAM, Bangalore after ejection were the subjects for the study. The group consisted of 18 pilots who reported after six weeks to one year of their ejection for review at the Institute. Details of initial radiological examinations-plain films (Fig 1), MRI (Fig 2) and CT (Fig 3) diagnosis were noted.
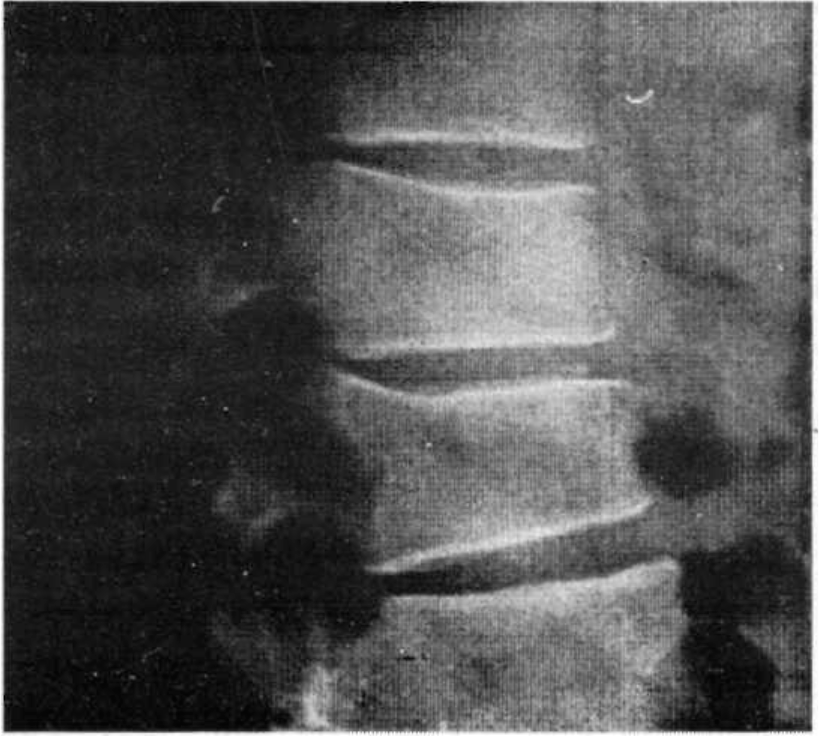
- Plain X-Ray - Fracture DV 12
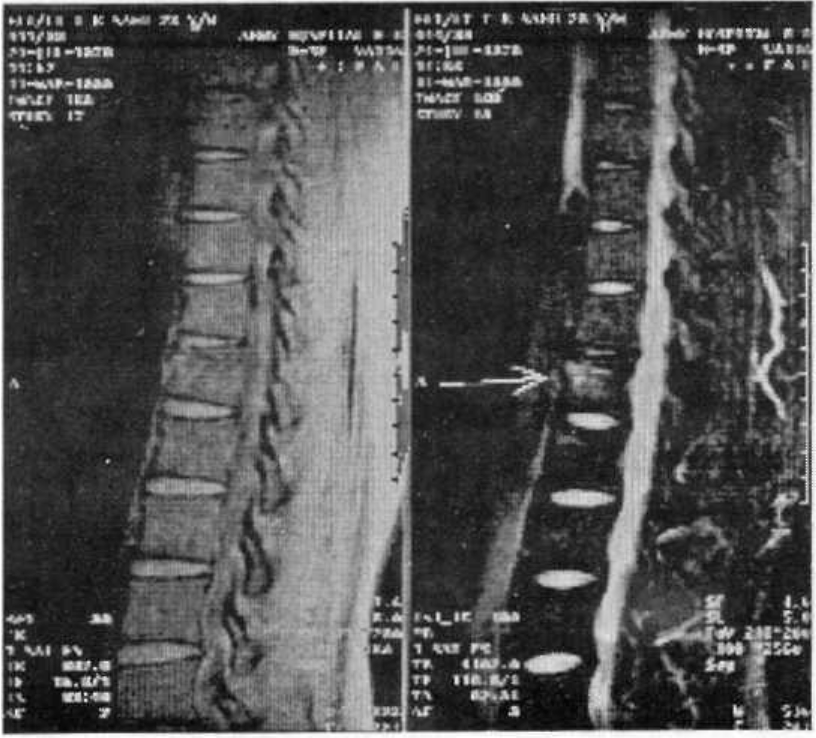
- MRI - Fractures DV 12
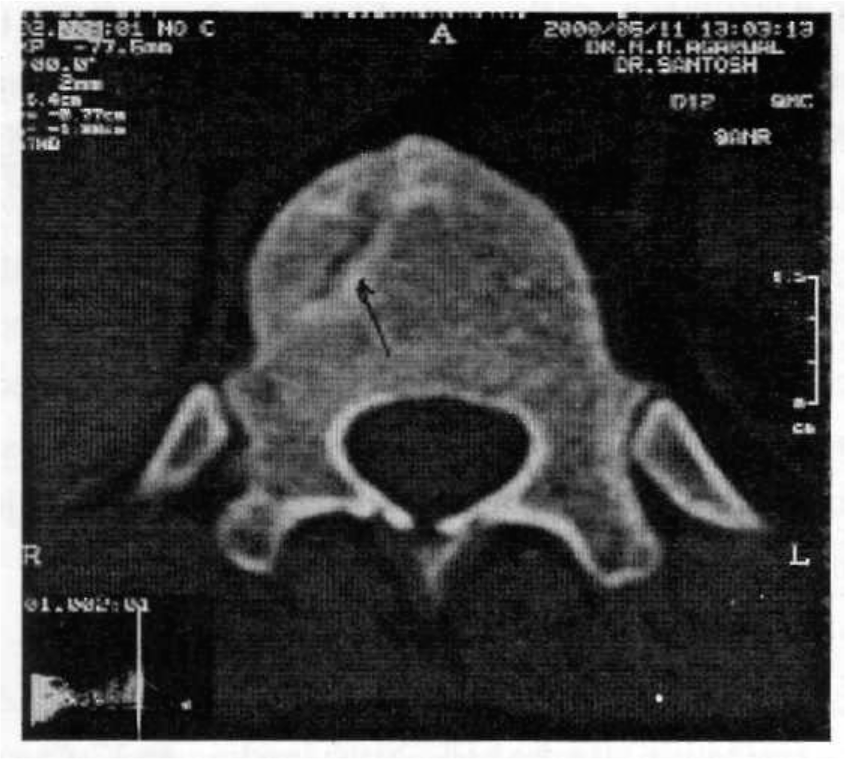
- CT - Fracture DV 12
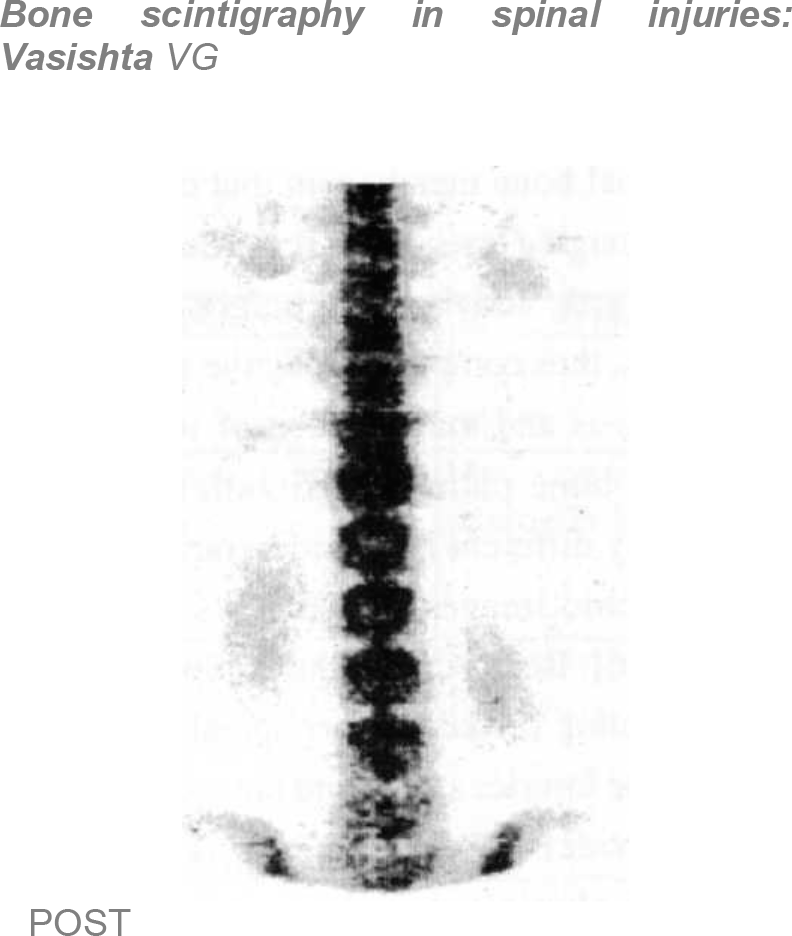
- Bone Scan - Hot Area DV 12
After this the patient was subjected to fresh CT/ Magnetic Resonance Imaging of the whole spine. (Fig 2,3)
This was followed up by Scintigraphic evaluation; 20 millicuries of Technetium 99m were administered IV and uptake determined by imaging with a dual head Gamma Camera 2-3 hours after the injection. The entire skeleton was scanned anteriorly and posteriorly with additional views taken from the side to separate background structures when needed. Fourteen of the scans were done in a private super-specialty hospital while the rest were done in CHAF (B). Bone scintigraphy or Bone Scan provides valuable information about local and regional bone metabolism that cannot be achieved by other imaging tests. Bone scans demonstrate changes in osteoblastic activity long before anatomic imaging modalities, thus complementing the anatomic studies in the diagnosis and management of traumatic and nontraumatic bone pathology. Scintigraphic imaging is remarkably different from radiographic imaging, since Scintigraphic images reflect physiology rather than anatomy [6]. Bone scan of the complete spinal column as a screening modality after spinal trauma can detect occult bone injuries apart from the more obvious ones. It often provides information that is very sensitive to changes in physiology, and thus can act as a useful tool to screen lesions of the spine. The high sensitivity of the nuclear study allows us to rule out bone pathology with a high degree of precision when the bone scan is normal. Additional CT and MR evaluation of the bone scan uptake regions can improve the overall specificity in the final diagnosis [7].
All the injuries to the bony column, intervertebral disc, soft tissue and ligaments and the neural elements (cord and nerve roots) were studied anatomically from CT and MR findings and physiologically as from bone scan results. These findings were then correlated clinically.
Results
18 pilots reported post ejection for evaluation at IAM during the period from Sep 2001 to Dec 2002. The details of their radiological evaluation are given in Table No. 1. The age group of the pilots was from 21 to 39 yrs (Fig 5). Out of these 11 had various patterns of spinal injury and 7 had no clinical or radiological spinal injury. Six of the aircrew who had sustained spinal injury had stable compression fractures of the dorsolumbar region (Fig 6). Six cases had mild to serious disc lesions as detected by MRI and amongst these, two had no associated bony injury. In two cases of injury Bone Scan detected an area of increased uptake at additional levels undetected by other investigations. In two other cases the patient was asymptomatic, Xray, CT/MRI had detected bony injury, but the bone scan was cold, implying that the injury was old. Similarly two cases that were asymptomatic and had normal plain radiographs were detected to have mild disc prolapse in MRI. However these cases had normal bone scan and the lesion was labeled as incidental. Incidental degenerative changes of the lower cervical and lumbar spine (bone scan of the involved region was cold) were also noted in three cases, away from point of injury. Five cases of bony injury came after more than nine months of injury and three out of these had normal bone scan.
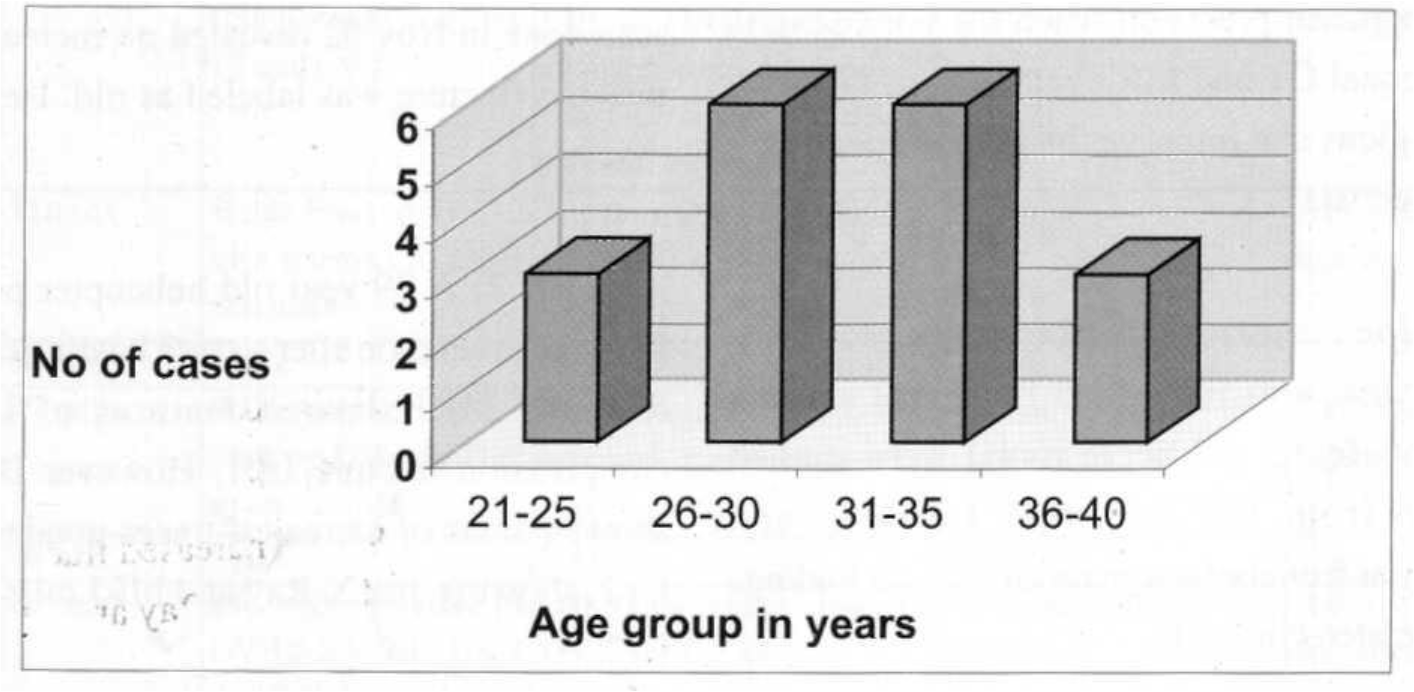
- Age distribution of post ejection cases reporting to IAM between Sep 2000 and Aug 2001
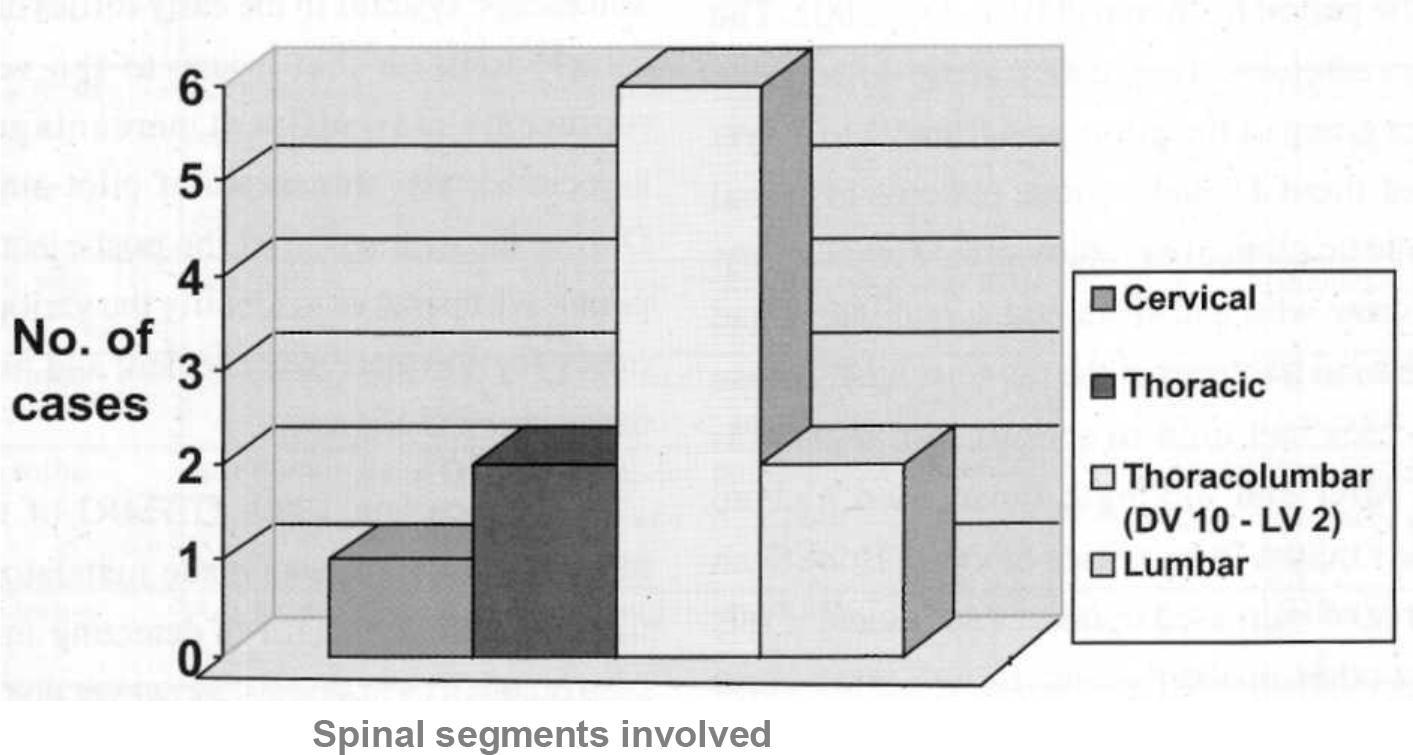
- Distribution of spinal segments injured in the 11 cases of spinal injury
| Case | Age | Time since | Xray | CT/MRI | Bone Scan | Remarks |
|---|---|---|---|---|---|---|
| No. | ejection | |||||
| 1 | 26 | 06 mths | Stable anterior wedging DV 10,11,12/ Sclerosis + | Anterior wedging DV 10,11,12 / no disc lesion | Hot spots from DV10 to LV4 | More extensive injury detected by BS |
| 2 | 21 | 07 mths | Stable Anterior wedging DV 11- LV1 / reduced disc space | Stable fracture of Dens + Old stable fracture DV11 to LV1 / Disc degeneration C 3-4,C4-5,DV10- 11 | Evidence of healing of DV12 | Dens fracture healed, D-12 # not yet healed |
| 3 | 27 | 06 wks | NAD | NAD | NAD | |
| 4 | 29 | 05mths | Stable anterior wedging LV1 | Anterior wedging LV1 | Increased uptake over LV1 andLV2 | More extensive injury detected by BS |
| 5, | 28 | 06 wks | Stable anterior Compression of DV 12 andLV 1 | Compression DV 12 and LV1 + early degenerative changes over L5 and SI with mild neural compression | Normal | Normal BS suggestive of old injury |
| 6 | 39 | 1 Imths | Stable Fracture DV12 with sclerosis of upper end plate | Fracture DV 12 mild disc bulge DV11 and DV 12 / no canal compromise | Normal | BS suggests complete healing |
| 7 | 26 | 06 wks | NAD | NAD | NAD | |
| 8 | 33 | 09 mths | St able Anterior wedging DV6/ IV Disc space normal | Wedge compression DV 6/ no canal compromise | Normal | Old injury or complete healing |
| 9 | 32 | 06 wks | NAD | NAD | NAD | |
| 10 | 38 | 12 mths | Ant wedge fracture of DV 12 > Yi and DV 7 < l/3rd / Disc space normal | Old compression fracture DV7 andDV12 | Mild increase uptake at DV12 | Stable # of DV 7 healed but unstable # DV 12 yet to heal completely |
| 11 | 33 | 11 mths | NAD | NAD | NAD | |
| 12 | 24 | 06 wks | NAD | CT was normal / MRI showed disc protrusion L 3-4, L5 SI indenting thecal sac | Normal | Incidental finding |
| 13 | 33 | 12 mths | Compression DV 8 less than l/3rd . Spondylotic changes CV4-6 | Compression fracture DV8 | Hot spot over DV 8 | Delayed healing DV 8 |
| 14 | 28 | 06 wks | Normal | MRI - disc protrusion CV 5 6 | Normal | Incidental finding |
| 15 | 34 | 9 mths | Compression DV 12 | Old healed fracture DV 12/ spondylotic changes and | Normal | Incidental finding of Schmorls node, |
| 16 | 23 | 3 mths | Ant compression DV-12, with mild reduction in disc space | Minimal Ant compression of body ofDV-12-post traumatic | Normal | Incidental finding probably due to old injury |
| 17 | 33 | 6 mths | Ant compression # DV-4 stable | Mild compression # DV-3, 4,5 | Normal | Healed fracture |
| 18 | 37 | 2 mths | NAD | NAD | Normal |
Case 1: A 23 year old fighter pilot reported to IAM for evaluation after he had a crash landing on 17 Aug 02. X-Ray and MRI showed an anterior compression fracture of DV12. He had no previous history of trauma. Bone scan done in Nov 02 revealed no increased uptake and thus the fracture was labeled as old. He was reflighted thereafter.
Case 2: A 29 year old helicopter pilot reported to IAM for evaluation after a crash landing on 19 Feb 02. X-Ray and MRI showed features of stable anterior compression fracture LV1. However Bone scan done showed areas of increased tracer uptake in LV1 and in LV2, showing that X-Ray and MRI missed the injury to LV2.
Discussion
Data obtained since the advent of aircraft ejection seat escape systems in the early forties of the last century, clearly indicate that injury to the vertebral column represents a significant percentage of morbidity associated with this mode of pilot-aircraft separation. During the evaluation of the post-ejection status of the pilot it is imperative to identify the various kinds of spinal injury for adequate management and further disposal of the concerned aircrew.
Since late 1999, CT/MRI of the whole spine following ejection was made mandatory and has been found extremely useful in detecting minor injuries not seen on plain radiographs. However due to the sensitivity of the investigation a good proportion of spinal bony as well as soft tissue defects were detected adding to the dilemma of the evaluator who had to now factor in these findings in his disposal. As a result observation in a period of non-flying category was the only resort but was an unscientific practice as there was no patho physiological basis for this. Moreover, the cervical spine in asymptomatic aviators of high performance aircraft show a significantly higher proportion of degenerative changes when compared with normal population [8].
The present study incorporates the whole body Technitium bone scan during the evaluation of 18 post ejection pilots. The results clearly show that it was possible to get significant information from these scans, namely: -
Injury to other spinal segments in 2 cases which had not been detected with other imaging modalities.
Date two lesions as old and co-incidental, and hence not caused by the present ejection.
Conclusion
Bone scan in the scenario of spinal injury serves in detecting/ ruling out occult injuries of the complete spinal column and also in estimating the time elapsed since injury [9]. There are other areas of interest, which need further evaluation like utility of the bone scan in the exact dating of the bony injury of the spine as per the uptake density. Therefore, we need the clinical utility of bone scan in detecting, managing and disposing ejection injuries of the spine, by incorporating it in our evaluation schedule of post ejection cases.
Recommendations
The present study has revealed that there are significant advantages in carrying out a whole body bone scan as the first part of the clinical evaluation of all post-ejection aircrew. A normal bone scan would preclude the need of CT/MRI examination of65 - 70% of ejectees and hence they can be inducted back to flying immediately thereafter. Secondly, the cost of CT/MRI examination can be saved in over 65% of ejection cases. CT/MRI would be required only in those cases showing abnormal uptake in bone scan. Thirdly, since whole body technetium bone scan not only reveals the anatomic picture of the injury but also the changing osteoblastic activity and therefore the physiology involved in repair, it helps in the final judgment of the precise line of treatment of the injured aircrew. The sensitivity of the investigation must be balanced by its specificity and screening by bone scan would keep the number of false positives to the barest minimum.
It is evident from the above that the bone scan should be carried out as an integral part of the regimen in the examination of post ejection aircrew since this effectively establishes or rules out occult injuries in the complete spinal column and also affords an important tool in determining with reasonable precision the date of the bone injury and hence the rate of healing. From the data thus obtained it would be possible to assess the time needed for complete recovery of the injured aircrew.
References
- An analysis of spinal injuries after ejection and crash landings in the IAF. Aviation Medicine. 1982;26:29-33.
- [Google Scholar]
- Analysis of ejection spinal injuries in IAF (1980-1987) Ind J Aerospace Med. 1988;32(1):25-31.
- [Google Scholar]
- Radiological Review of Spinal Injuries Sustained during combat flying, heavy landing and ejection (96-98) Ind J of Aerospace Med. 1999;43(1):29-34.
- [Google Scholar]
- Dating of spinal fracture by bone scan-A case report. Ind J Aerospace Med. 1999;43(2):78-81.
- [Google Scholar]
- MRI Cervical Spine Findings in Asymptomatic Fighter Pilots. Aviation Space and Environmental Medicine 70, No 12. :1183-88.
- [Google Scholar]
- Role of computed tomography in spinal trauma. J Indian Med Assoc. 1999;97(12):486-8.
- [Google Scholar]






