Translate this page into:
A case of incidentally detected spina bifida at DV1 level in a fighter pilot: Aeromedical deliberations

*Corresponding author: Neha Arun Rao, Institute of Aerospace Medicine, Indian Air Force, Bengaluru, Karnataka, India. neharao2193@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rao NA, Rathore N, Suryakiran K, Binu Sekhar M, Ghosh G. A case of incidentally detected spina bifida at DV1 level in a fighter pilot: Aeromedical deliberations. Indian J Aerosp Med 2024;68:25-7. doi: 10.25259/IJASM_5_2023
Abstract
A failure of closure neural tube normally results in spina bifida. The lesions may occur anywhere along the spine but are more common in the lumbosacral region (90%) in comparison to the thoracic (6%) or cervical (3%) spines. According to policy guidelines, all cases of spina bifida are unfit for all branches and trades in military flying, except for spina bifida in the sacrum and 5th lumbar vertebra, if completely sacralized. When various congenital defects are considered, spina bifida at the SV1 level is relatively innocuous. However, an anomaly in the upper spinal regions is associated with the narrowing of the spinal canal, which may be accompanied by herniation of meninges. This could be exacerbated and lead to abrupt incapacitation during flight when a spine like this is subjected to high +Gz accelerations or ejection forces. This paper highlights a case of a fighter aircrew who was incidentally detected to have spina bifida at 1st dorsal vertebra level during evaluation for cervical prolapsed intervertebral disc and the aeromedical deliberations for its disposal.
Keywords
Spina bifida
Fighter pilot
Aeromedical disposal
INTRODUCTION
A failure of the closure neural tube normally results in spina bifida. The spinous process may consist of two rudimentary processes that do not fuse along the midline, or it may be entirely absent.[1] There are four types of spina bifida: Occulta, closed neural tube defects, meningocele, and myelomeningocele. According to standard practice guidelines, all cases of spina bifida are unfit for all branches of flying in the armed forces, except spina bifida in the sacrum and 5th lumbar vertebra, if completely sacralized. Lesions may occur anywhere along the spine but are more common in the lumbosacral region (90%) than in the thoracic (6%) or cervical (3%) spines, with the overall incidence being about 17%. However, an anomaly in upper spinal segments is associated with the narrowing of the spinal canal, which may be followed by herniation of the meninges.[2] When such a spine is subjected to high +Gz accelerations, this could be exacerbated and lead to the development of acute symptoms that could incapacitate the pilot during the flight and also increase the propensity of ejection injuries. This paper highlights the aeromedical deliberations in a case of incidentally detected spina bifida for making him fit for flying duties.
CASE REPORT
This is a case of a 33-year-old fighter pilot. He had a total flying experience of around 700 hours, including about 500 hours in fighter aircraft. He initially developed insidious onset of neck pain, which aggravated in the subsequent months. On evaluation, he was detected to have prolapsed intervertebral disc (PIVD) at the 3rd cervical vertebra (CV3)–CV4 to CV6–CV7 levels. He was recommended conservative management and was advised to rest. After a sufficient period of observation, the aircrew was reviewed again. His symptoms had reduced. His functional evaluation revealed no restrictions in the range of movements at the cervical spine region and satisfactory weight-bearing in both upper limbs. The aircrew was also subjected to simulated aviation stresses, and he could tolerate them without any pain or discomfort.
During the review, while evaluation the aircrew was incidentally detected to have spina bifida at 1st dorsal vertebra (DV1) level on X-ray cervical spine [Figure 1]. The aircrew was further evaluated with non-contrast computer tomography cervicothoracic spine, which confirmed that the spina bifida DV1 is an isolated finding without any involvement on the rest of the osseous structures, visualized joint spaces and surrounding soft tissues. X-ray screening of the entire spine confirmed that the spina bifida was present only at a single level. On review by the neurosurgeon, it was observed that the aircrew had no neurological deficit, and there was no neural compression or any other stigmata at the DV1 level. Hence, the aircrew was recommended to be fit for flying. His functional evaluation and exposure to simulated aviation stress tests did not show any restriction which precludes him from the award of fitness for flying duties.
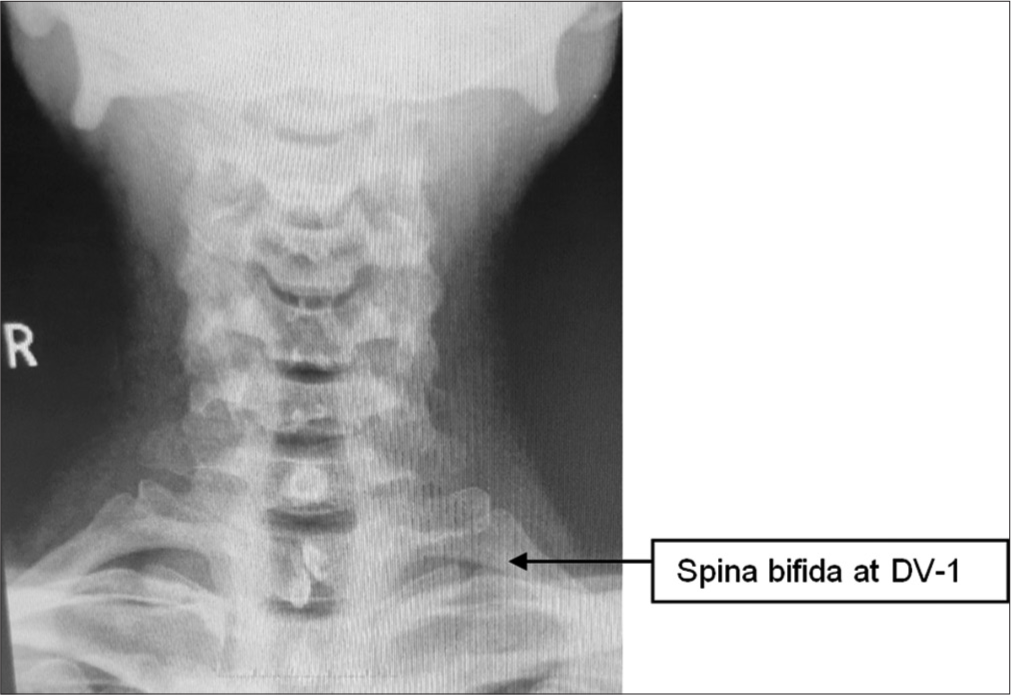
- X-ray cervicodorsal spine.
The current practice guidelines state that spina bifida at the DV1 level is unfit for Air Force duties (both flying and ground) in Initial Medical Evaluation at the entry level.[3] On account of the case being of spina bifida with no neural compromise in the trained workforce and considering the additional risk of spinal injury during ejection and chronic vibration, the aircrew was made fit to fly transport aircraft only. The performance of the aircrew in a transport aircraft was evaluated with an executive report on flying. His executive report with respect to transport aircraft for satisfactory performance during long duration flying duties was complementary.
DISCUSSION
Spina bifida occulta (SBO) is a developmental abnormality that consists of an interruption in the continuity of the posterior arch. The spinous process may be absent or is composed of two rudimentary processes from the laminae meeting but not fused in the midline. The intervening space is occupied by a fibrous membrane. SBO, without cutaneous manifestations, is rarely associated with any clinical consequences.[4] In the present case as well, the aircrew did not present with any cutaneous manifestations or any neurological deficits. He has endured aviation stressors in the form of high G exposures and vibration stress during his flying career and has not reported any clinical features attributable to spina bifida DV1. A literature reference from United States Army Aeromedical Research Laboratory concluded that for low level G exposures of repeated impacts in surface ride motion, normal asymptomatic individuals with SBO at one vertebral level and no cutaneous manifestations are not at increased risk for personal injury.[5] Considering the above, the aircrew was assessed fit for flying duties for spina bifida DV1, but his fitness to sustain ejection forces needs further deliberation.
Ejection spinal loading is of the order of 20 G at the rate of 300 G/s. The injury potential from the force of this order of magnitude has not been estimated for spinal conditions like spina bifida in the available literature. Although, primarily, the ejection forces are transmitted through vertebral bodies under normal ejection posture and with stable spinal column.[6] It is unclear that what amount of axial loading occurs through the lamina and other posterior elements of vertebrae during high force transmissions. The spina bifida, in this case, is at the DV1 level, which is at the junction of the mobile cervical spine and the fixed dorsal spine. Therefore, it is possible that asymmetric force transmission occurs due to the rotational angle of the cervical spine while exposed to catapult and wind blast forces of ejection as well as during parachute opening shock. The addition of helmet-mounted devices such as helmet mounted displays (HMDs) increase the overall helmet weight and thus the force and mass moments. The probability of increased force transmissions to posterior elements of vertebrae as a result of changes in the center of gravity and higher mass moments cannot be ruled out. Therefore, it was considered that the aircrew was unfit for flying ejection seat aircraft for the disability spina bifida DV1. A study by Jelsma and Ploenter states that the disability SBO has been associated with a higher prevalence of backache.[7] In addition, operational flying in helicopters is also associated with the use of heavy head supported loads such as helmets with HMDs and night vision goggles (NVGs). Considering the aircrew being an old case of PIVD C3–C4 to C6–C7 and the higher incidence of backache in helicopter flying, he was considered unfit for flying helicopters as well. Therefore, he was recommended to be restreamed to transport aircraft.[8]
CONCLUSION
In the aviation environment, the human spine is subjected to various stresses during flight and at the time of ejection. Considering all the deliberations above, the aircrew was assessed fit for flying duties but was recommended to be restreamed to transport aircraft. This case report can be used for future aeromedical decision-making to preserve a trained workforce. This case also strengthens the necessity of a detailed medical evaluation to be carried out before accepting a candidate for flying training, as the overall prevalence of SBO in the general population is about 5–10%. During the initial entry medical evaluation, detailed reporting of the X-ray whole spine by the radiologist is recommended.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Orthopedics: Principles and their applications (4th ed). New York: JP Lippincott Company; 1984. p. :1552-5.
- [Google Scholar]
- Congenital abnormalities of spine and flying fitness: Evaluation and disposal. Indian J Aerospace Med. 2001;45:30-6.
- [Google Scholar]
- Textbook of disorders and injuries of the musculoskeletal system (2nd ed). Baltimore: Williams and Wilkins; 1984. p. :133.
- [Google Scholar]
- Injury risk for research subjects with spina bifida occulta in a repeated impact study: A case review. Aviat Space Environ Med. 1996;67:767-9.
- [Google Scholar]
- Spina bifida occulta of S1 is not an innocent finding. Spine (Phila Pa 1976). 1994;19:12-5.
- [CrossRef] [PubMed] [Google Scholar]
- Painful spina bifida occulta with review of literature. J Neurosurg. 1953;10:19-27.
- [CrossRef] [PubMed] [Google Scholar]






