Translate this page into:
Fitness for fighter flying in a resolved case of neurocysticercosis: Dilemma in aeromedical disposition

*Corresponding author: Karthikeyan Sankaran, Department of AP and SO, Institute of Aerospace Medicine, IAF, Bengaluru, Karnataka, India. skarthikeyan02@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sankaran K, Bhowmick B, Sarkar R. Fitness for fighter flying in a resolved case of neurocysticercosis: Dilemma in aeromedical disposition. Indian J Aerosp Med 2023;67:59-63. doi: 10.25259/IJASM_10_2023
Abstract
Neurocysticercosis (NCC) is the most common helminthic infection of the human central nervous system, and it’s the leading cause of acquired epilepsy worldwide. The clinical manifestations vary depending on the location, cyst stage, and host immune response. Seizure is the most common clinical presentation, but many patients present with focal deficits, intracranial hypertension, or cognitive decline. Neuroimaging is the mainstay of diagnosis. Cysticidal treatment, along with steroids, has shown increased and faster resolution of lesions. Seizure responds well to a single antiepileptic drug, and its recurrence rate is low with single lesions. Multiple and calcified lesions have recurrent seizures and require AED for a longer duration. Aeromedical concerns of the disease include the occurrence of any neurologic or cognitive symptoms and signs, and AED can have a CNS depressant effect. An in-flight seizure can cause unsustainable aircraft attitude, accidentally altering controls or engaging weapon systems and compromising flight safety. A 33 year old fighter aircrew of IAF with a flying experience of approximately 950 hours had an episode of generalized tonic clonic seizure. His MRI Brain revealed a ring-enhancing lesion in the left inferior temporal gyrus (<20mm) and was diagnosed as a case of Neurocysticercosis (Parenchymal NCC). He was managed conservatively with cysticidal therapy along with steroids and AED. During his follow up after six months, his CECT Brain revealed no residual lesions, and he was advised to stop AED. He has been observed adequately in the non-flying medical category for a period exceeding one year post stoppage of AEDs without seizure recurrence. Now, he was upgraded to the restricted flying category for another one year of observation before considering him for awarding the full flying category. The aeromedical concern in a case of Neurocysticercosis with seizure is a risk of sudden in-flight incapacitation due to seizure. In military/civil flying, the aircrew can be considered for unrestricted flying category for transport and helicopters. In this case, the aircrew had only a single episode of seizure, which was his presenting symptom, and had complete resolution of the brain lesion. However, after careful deliberation and consideration of all aeromedical concerns the decision was taken to reflight the aircrew in fighter flying with restriction.
Keywords
Neurocysticercosis
Seizure
Fighter aircrew
INTRODUCTION
Neurocysticercosis (NCC) is the most common helminthic infection of the human central nervous system, and it is the leading cause of acquired epilepsy worldwide caused by tapeworm Taenia solium.[1-4] It is endemic in Latin America, South East Asia, India, Nepal, China, Africa, and many other developing countries[2,4] [Figure 1]. Due to globalization, NCC is also reported in developed countries such as the USA, UK, and Other European countries.[2] According to the World Health Organization, 30% of all epilepsy in endemic countries and 3% of epileptic cases globally may be due to NCC.
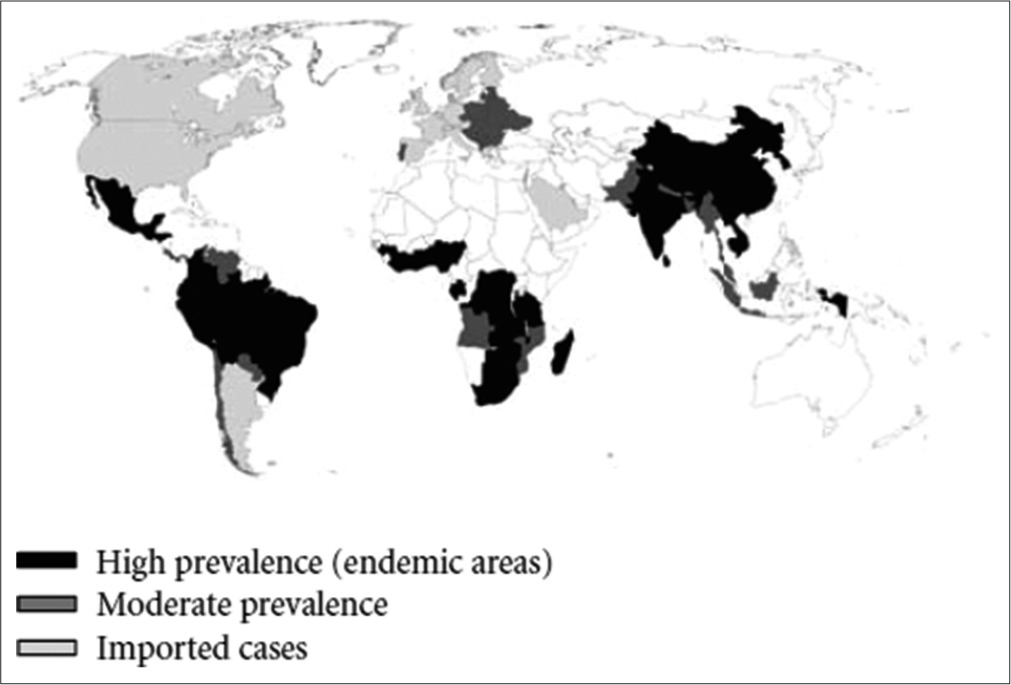
- World map showing neurocysticercosis geographical distribution.
T. solium has a complex life cycle, with pigs acting as the intermediate host and humans acting as the definitive host.[1,5] After consuming taenia eggs, the human can potentially act as an intermediate host [Figure 2]. Taeniasis and cysticercosis are the two clinical manifestations of the illness.
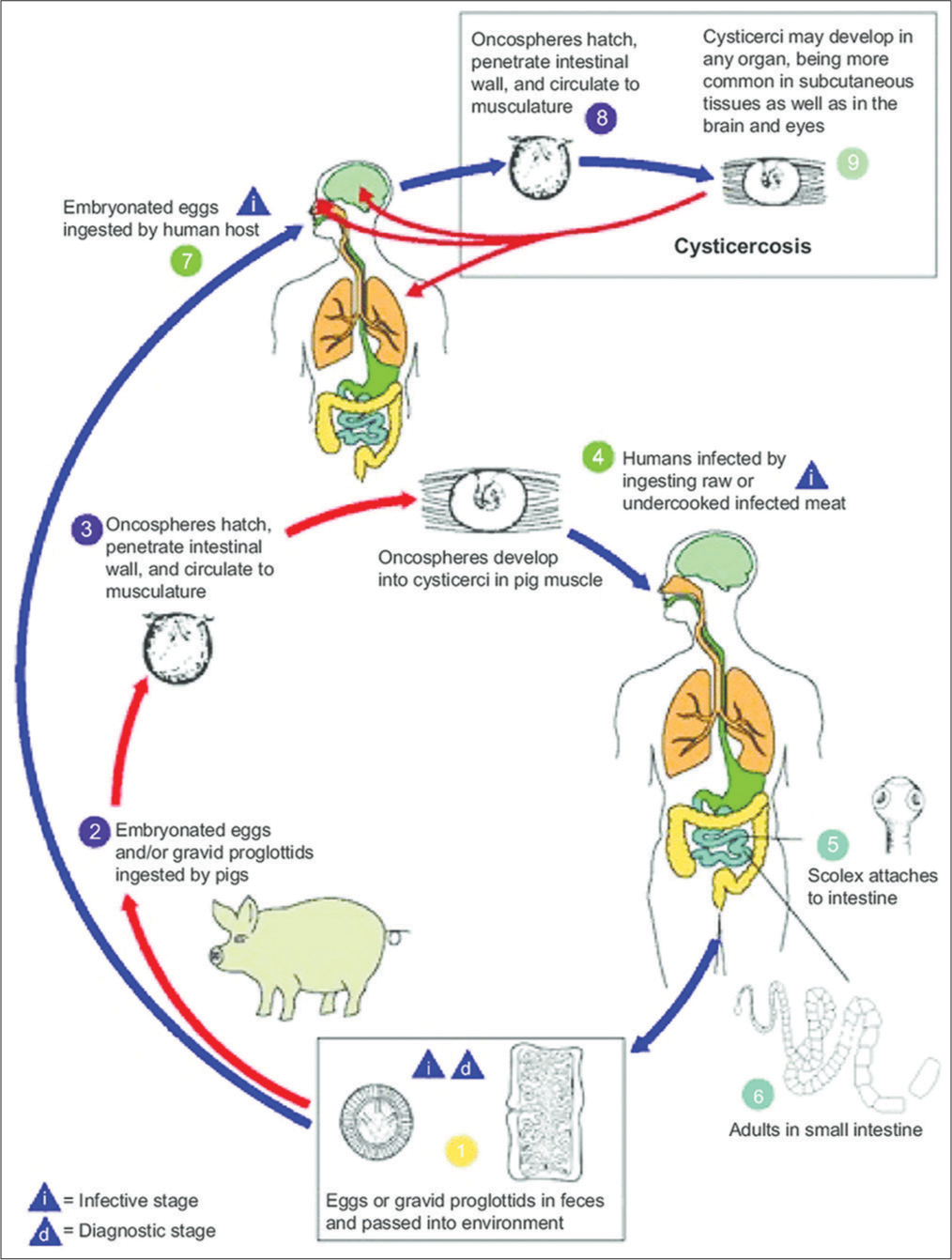
- Life cycle of Taenia solium. Reproduced from the Centers for Disease Control and Prevention. Cysticercosis. Atlanta, GA: Centers for disease control and prevention.
The clinical manifestation of NCC might range from asymptomatic instances to cases with serious neurological problems and even death. The difference in the clinical picture depends on the number, size, localization, and stage of the cysts and the host’s immune response to the parasite.[1-4] Seizure is the most common clinical manifestation in almost 70% of patients with parenchymal NCC.[2,4,6]
The parenchymal larval cyst has four stages of development: Vesicular, colloidal, nodular, and calcified. Seizure occurrence might be due to the inflammatory response elicited by degenerating cysts; however, it can occur at any stage of the cyst.[2] Extraparenchymal NCC causes raised intracranial pressure, focal deficits, hydrocephalus, arachnoiditis, and chronic meningitis. Visual impairments may result from those in the extraocular muscles and the eyes. Unusual presentations such as neurocognitive deficit, dystonia, and behavioral changes have also been reported.[2,3]
Diagnosis is made mainly by neuroimaging. Computed tomography (CT) scan is more commonly used in endemic countries. For the diagnosis of NCC, CT scans show a sensitivity and specificity of 95%.[7,8] However, magnetic resonance imaging (MRI) can more accurately detect the degrees of infection, location, and evolutionary stage of the parasite. Degenerative alterations, perilesional edema, and smaller cysts or cysts found in the ventricles, cerebellum, brain stem, eye, and spine can all be found with this method.[1] The serodiagnostic tests’ sensitivity ranges from 65% to 98%, and their specificity ranges from 67% to 100%, making them of little significance in clinical practice.[9] The enzyme-linked immunoelectrotransfer blot (EITB) assay is a reliable serological test that uses lectin-purified glycoprotein antigens to detect T. solium antibodies in serum. The sensitivity and specificity of EITB are around 98% and 100%, respectively, for patients with two or more live parasites in the nervous system. EITB does not cross-react with heterologous infections. Detection of anti-cysticercal antibodies in the cerebrospinal fluid (CSF) by enzyme-linked immunosorbent assay (ELISA) is 87% sensitive and 95% specific in patients with viable NCC infections and is still used when EITB is not available. Due to its increased specificity, ELISA is more dependable in CSF than in serum and has a sensitivity for subarachnoid NCC that is comparable to the EITB. Positive serum antibodies on EITB are one of the major criteria for diagnosis of NCC.[10]
A combination of symptomatic and cysticidal therapy is used to treat NCC. Praziquantel and albendazole are efficient treatments for NCC. Albendazole outperforms praziquantel in that it eliminates 75–90% of parenchymal cysts and is also effective in treating extraparenchymal cysts. Antiepileptic medications or steroids do not interact with albendazole.[1] Seizure is the most common symptom, occurring in 90% of patients.[11] Albendazole has the added advantage of a significant reduction in seizure recurrence. Seizure is managed with first-line AEDs, which usually result in good seizure control.[1,11] The Duration of treatment with AED is debated, and it is continued until the complete resolution of cysts on neuroimaging. However, parasites that are dormant or have calcified may result in unprovoked seizures. The patient should continue receiving treatment until they are clear of seizures for two years.[1]
The overall recurrence of seizure in parenchymal NCC after the first symptom is 50% in 7 7-year period follow-up, and half of these recurrences occur in the 1st year. The risk factor for recurrence is persistent abnormalities in neuroimaging. Recurrence was found in 56% of cases with persistent cysts, 52% with calcification, and only 22% with no cyst.[11]
The aeromedical dilemma of such cases includes the effects of any residual neurological or cognitive symptoms and signs and any effects of medication on mission safety and effectiveness and future risk of seizure recurrence with resulting inflight incapacitation. This paper discusses the aeromedical decision-making for a completely resolved case of NCC and fighter flying.
CASE REPORT
A 33-year-old military fighter pilot with no history of any medical condition, with approximate flying hours of 950 hours, had an episode of generalized tonic-clonic seizure in September 2020. His contrast-enhanced MRI (CEMRI) brain revealed ring enhancing nodular lesion of 11.5 × 11.5 × 13 mm size in the left inferior temporal gyrus – likely colloidal vesicular stage and was diagnosed as a case of NCC in September 2020 [Figure 3]. He was managed with tablet albendazole along with steroids for two weeks and AED for seizure control. During his follow-up after one month in October 2020, his systemic examination was found to be normal, and his MRI brain showed a moderate reduction in the size of the cyst to 6.5 × 6 × 8.3 mm with a significant reduction in perilesional edema [Figure 4]. He was continued on AED. During his next review in April 21, his fresh contrast-enhanced computed tomography brain did not reveal any residual lesion [Figure 5]. The neurologist advised the stoppage of AED.
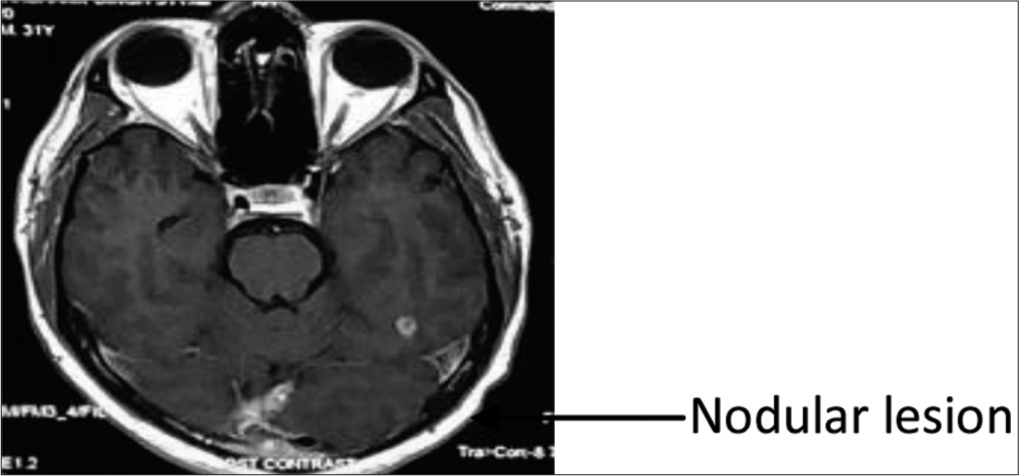
- Magnetic resonance imaging brain September 2020.
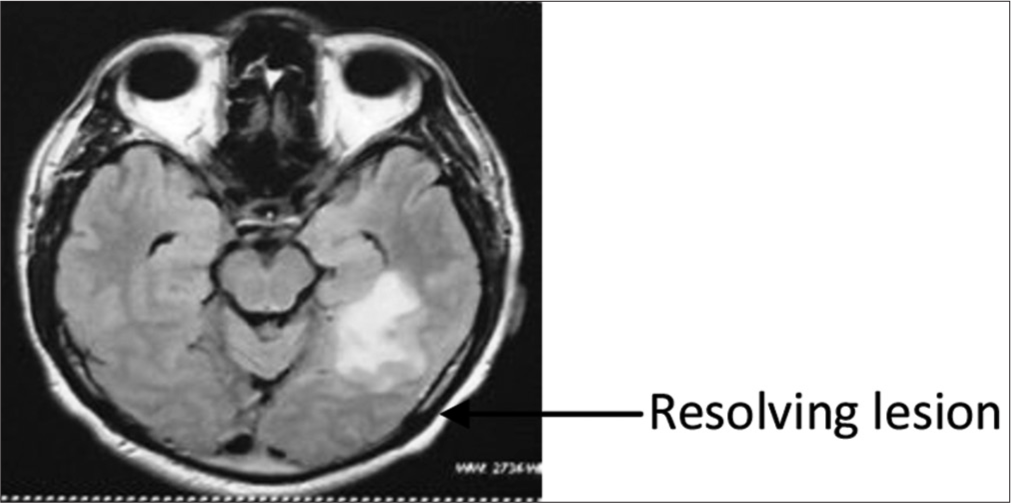
- Magnetic resonance imaging brain October 2020.
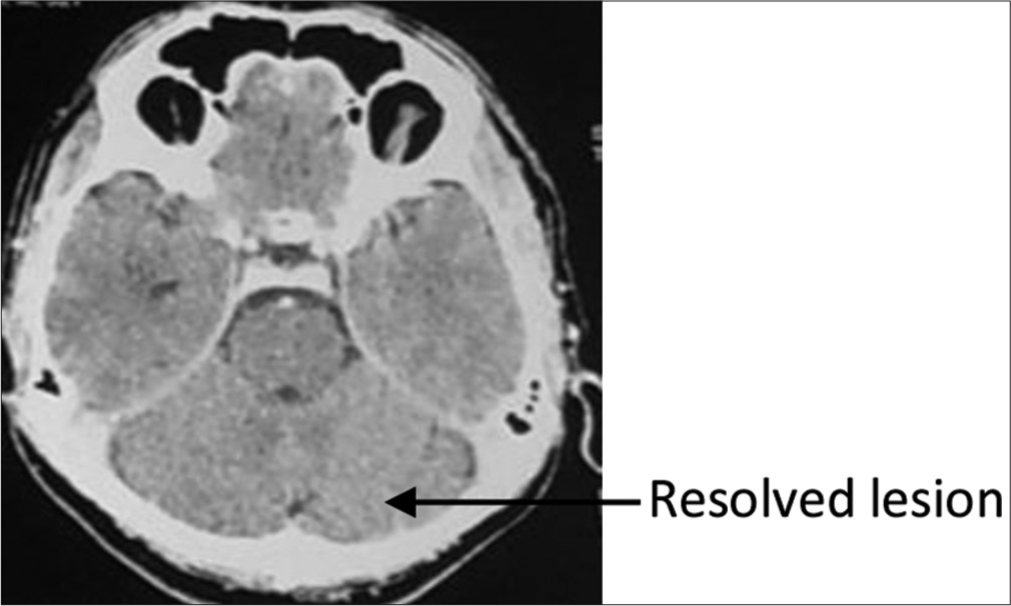
- Contrast-enhanced computed tomography brain April 2021.
During his next follow-up in August 2021, his CEMRI showed no abnormality in the brain parenchyma and EEG was normal. He was recommended to be continued in the non-flying medical category and was advised to be further reviewed at the Indian Air Force (IAF) Boarding Centre only after observation for two years post-AED-free period.
The aircrew reported to IAF Boarding Centre in July 2022 for evaluation. During the evaluation, his MRI brain [Figure 6] revealed no definitive abnormality, and there was a complete regression of infective granuloma in the left temporal lobe and all other blood and biochemical parameters were normal. The neurologist advised him that he was fit for carrying out all duties. The aeromedical dilemma of such cases involves the risk assessment of seizure recurrence and any residual lesion in the brain. The aircrew did not have any residual brain lesion, and except for the presenting symptoms, initially, aircrew had no seizure recurrence with and without AED.
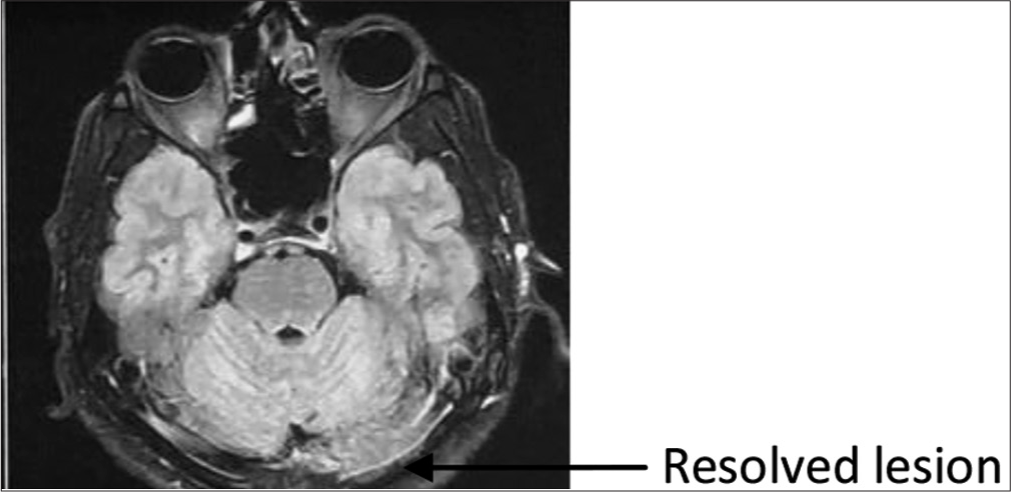
- Magnetic resonance imaging brain July 2022
DISCUSSION
In this case, the aeromedical decision was taken based on the following:
Risk assessment and present state of the case
The aircrew had only suffered a single episode of seizure, which also was the presenting complaint for the current disability
Post initial CEMRI, he was diagnosed with a case of NCC, which was treated adequately with medication (tab albendazole 400 mg BD for 14 days)
He was also put on AED (tab levetiracetam) for one year (till April 2021), which was stopped on the recommendation of the neurologist as there was no residual lesion in the neuroimaging
There was no recurrence of seizure while being on AED or in the past one year (56 weeks) during the AED off-period
The MRI brain of July 2022 had revealed no definitive abnormality. There was a complete regression of infective granuloma in the left temporal lobe as compared to the initial CEMRI
Around 35–50% of individuals with calcified lesions in brain parenchyma have recurrent seizures due to inflammation and perilesional edema. The risk of seizure recurrence in this patient with a single brain lesion and complete resolution in neuroimaging was minimal.[12]
Extant policy for disposal of cases of NCC/seizure
Most of the international waiver consideration is only for seizures and is not specific to NCC. According to the US Air Force and US Navy waiver guide, an aircrew with provoked seizures can be considered for upgradation on an individual basis, but those with unprovoked seizures are not considered for upgradation.
In accordance with Indian Air Force guidelines, NCC presenting with seizure or on AED are disposed as below:
An aircrew can be considered for upgradation to full medical category after completion of seizure-free period while on AED and a minimum of 2-year seizure-free period without AED.
Flying is normally permitted only in Tpt/Heptr.
As per DGAFMS medical memorandum No 188 (Guidelines for management and disposal of cases with seizures/epilepsy in the Armed Forces), individuals with acute symptomatic seizure and with solitary seizure managed with AEDs can be considered for upgradation after 1-year seizure-free period without AED to full medical category.
Based on the above consideration, the present condition aligns more with “Acute symptomatic seizure of transient nature,” and disposal of such cases should be based on the primary medical condition and not on the associated seizure.
Acute symptomatic seizure of transient etiology can be considered fit for fighter flying on a case-to-case basis, subject to waiver by higher medical authority.
Aeromedical decision-making
The aeromedical concern for NCC with seizure includes the effect of any neurologic or cognitive symptoms and signs, medication effects on operation safety and mission effectiveness, and future risk of seizure resulting in sudden in-flight incapacitation.
The prognosis of seizures in patients with a single lesion is good. In more than 60% of patients, the seizure is successfully controlled, and the lesion resolves within six months. Seizure recurrence is common in instances that involve multiple lesions and calcification.[1,2,4,11]
Aeromedical disposition
In the present case, the aircrew had only a single episode of seizure, and post-antihelminthic therapy and AED therapy of about 08 months, there is no radiological evidence of any parenchymal abnormality. Therefore, the risk of sudden and subtle incapacitation in flight has been considerably ruled out, as there is no existing disqualifying defect
After treatment initiation, the seizure relapse rate in patients with single granuloma ranges from 13% to 48%; with calcified lesions, it is 10–34%, and with multiple cysts, it ranges around 54%[12]
Although the primary trigger for seizure is completely resolved, as evident, he has undergone AED therapy for a single episode of seizure of transient etiology; therefore, it will be prudent to observe him for some more time before considering him for assessing fit to fly single cockpit aircraft giving due diligence to flight safety considerations.
The aircrew was upgraded fit-to-fly on the type (fighter aircraft) only in the dual cockpit and may be considered for further upgradation to fly a single cockpit if he remains seizure-free and off AEDs for a period of 2 years after stoppage of AED.
CONCLUSION
The most frequent cause of acquired epilepsy is NCC, which has a good prognosis.[2] In cases with a single lesion, it has been observed that seizures caused by NCC are successfully controlled, but they reoccur in situations with many persistent and lesions that still have residual calcification. After due deliberation and considering all aeromedical concerns, a decision was taken to reflight the aircrew in fighter flying. This is the first instance, as of to our knowledge, that a decision was taken to reflight back a case of NCC with seizure in fighter flying. This decision was taken based on the scientific evidence, neuroimaging, and clinical evaluations. This being an index case, considerable duration with safety has to pass after which it may be considered as a reference case.
Acknowledgment
The author acknowledges the contribution of Gp Capt (Dr) Rahul Pipraiya (Retd) for his guidance and contribution to this aeromedical decision-making.
Disclaimer
The views expressed in this article are those of the author and do not represent the official opinions of the Indian Society of Aerospace Medicine or the Indian Air Force.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neurocysticercosis: A review of current status and management. J Clin Neurosci. 2009;16:867-76.
- [CrossRef] [PubMed] [Google Scholar]
- Neurocysticercosis: An update. Lancet Infect Dis. 2002;2:751-62.
- [CrossRef] [PubMed] [Google Scholar]
- Neurocysticercosis: A review. ScientificWorldJournal. 2012;2012:159821.
- [CrossRef] [PubMed] [Google Scholar]
- Introduction to neurocysticercosis: A worldwide epidemic. Neurosurg Focus. 2008;12:1.
- [CrossRef] [Google Scholar]
- Neurocysticercosos in South-Central America and the Indian subcontinent. A comparative evaluation. Arq Neuropsiquiatr. 1997;55:349-56.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advances in the diagnosis and treatment of cerebral cysticercosis. N Engl J Med. 1984;311:1492-6.
- [CrossRef] [PubMed] [Google Scholar]
- Focal epilepsy in India with special reference to lesions showing ring or disc-like enhancement on contrast computed tomography. J Neurol Neurosurg Psychiatry. 1987;50:1298-301.
- [CrossRef] [PubMed] [Google Scholar]
- An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium) J Infect Dis. 1989;159:50-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic criteria for neurocysticercosis, revisited. Pathog Glob Health. 2012;106:299-304.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis for seizure recurrence in patients with newly diagnosed neurocysticercosis. Neurology. 2002;59:1730-4.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical symptoms, diagnosis, and treatment of neurocysticercosis. Lancet Neurol. 2014;13:1202-15.
- [CrossRef] [PubMed] [Google Scholar]






