Translate this page into:
Analysis of major ocular conditions leading to rejection in the Air Force aspirational candidates and change in our practice pattern for future

*Corresponding author: Vikas Sharma, Department of Ophthalmology, 5 Air Force Hospital, Jorhat, Assam, India.vikas.sharmadr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh AK, Sharma V, Malik R, Reddy S. Analysis of major ocular conditions leading to rejection in the Air Force aspirational candidates and change in our practice pattern for future. Indian J Aerosp Med 2023;67:41-5. doi: 10.25259/IJASM_30_2022
Abstract
Objectives:
The Armed Forces offer a great career opportunity to the aspirants. It is a matter of pride to serve the nation. Unfortunately, a significant number of Air Force aspirants fail to clear their medical examinations. The ophthalmological examination remains one of the leading causes of rejection of these candidates. In this article, we have tried to find out the major ocular conditions that have led to the rejection of these candidates.
Material and Methods:
This retrospective study was done from the examination records of the Department of Ophthalmology at the boarding center of the Air Force from January 01, 2020, to March 31, 2022. These records consisted of the personal particulars of the candidates, their registration number, the stream that the individual has applied for, the findings of the ophthalmologists, and his remarks (highlighted in bold) regarding the fitness and signature with date. The data were then tabulated and analyzed.
Results:
Out of 2003 candidates, 251 candidates (12.5%) were declared unfit due to various ophthalmic conditions. Substandard vision remains the leading cause of rejection. Defective color perception, lattice degeneration, and Post LASIK criteria not meeting the laid down standards are other major causes of rejection.
Conclusion:
The young generation is the backbone of a nation, and their motivation leads to shaping of the country’s future. Armed Forces being one of the most lucrative career options a considerable majority of them lose confidence and become demotivated on being unfit due to pre-existing ocular conditions. They would have chosen an alternative stream if they had known about their ocular condition beforehand, the authors suggest that every individual must be thoroughly ophthalmologically examined at around 14–16 years of age equating to 10–12 standard during their studies. This will help them to choose their career in the armed forces or civil stream.
Keywords
Substandard vision
Kerato-refractive surgery
Color vision deficiency
Air Force
INTRODUCTION
The Armed Forces offer a great career opportunity to the aspirants. Almost everybody aspires to join various streams of Armed Forces as it gives them a chance to serve the nation as well as it is considered a reputed job among peers. Despite various hardships, joining the Armed Forces is considered a matter of pride in society across the country; moreover, it also ensures job security for individuals. Thus, aspirants put their hearts and soul together and devote their precious time to get through the process of selection for the Armed Forces. As armed forces personnel are destined to work in various extreme weather situations, be it land, water, or air, they must possess high levels of physical and medical standards. These standards are well laid down in all three forces.[1] Among the medical examinations, the ophthalmological examination is very important for most of the branches of the Armed Forces, especially the aviation, air traffic controller etc.
In this article, we are presenting our 2 years of data wherein reflecting the major causes of rejection during the ocular examination. Since most individuals come from different parts of India, they are a reflection of the prevalence of various ocular conditions across the country.
MATERIAL AND METHODS
The retrospective analysis was done from the examination records of the Department of Ophthalmology at the boarding center of the Air Force from January 01, 2020, to March 31, 2022. Detailed ophthalmological examination was done for all the candidates and findings were recorded. These records consist of personal particulars of the candidates, their registration number, the stream/branch of the Air Force (the individual has applied for), the findings of the ophthalmologists, his remarks (highlighted in bold) regarding the fitness, and signature with date. The data were then tabulated and analyzed.
RESULTS
The data of a total of 2003 candidates were analyzed [Figure 1]. All the candidates were more than 17 years of age. Out of 2003 individuals, 1677 (83.7%) were male and 326 (16.3%) were females. Out of 2003 individuals, 1752 (87.5%) individuals were declared fit and 251 (12.5%) were made unfit after ophthalmological evaluation [Figure 2] as per records. A list of ocular conditions leading to rejection is enumerated in Table 1 and Figure 3.
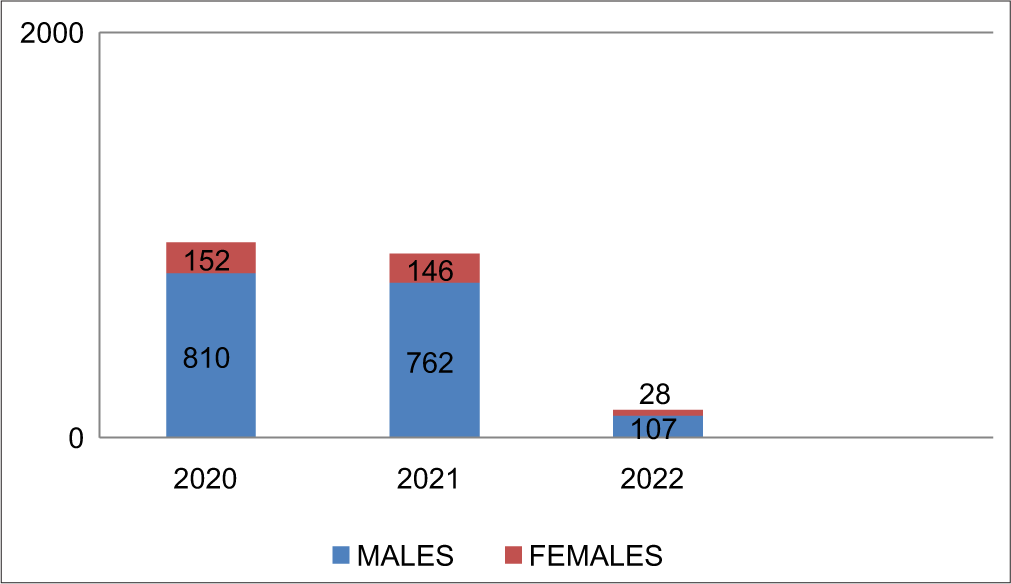
- Total number of candidates (of either sex) examined year wise.
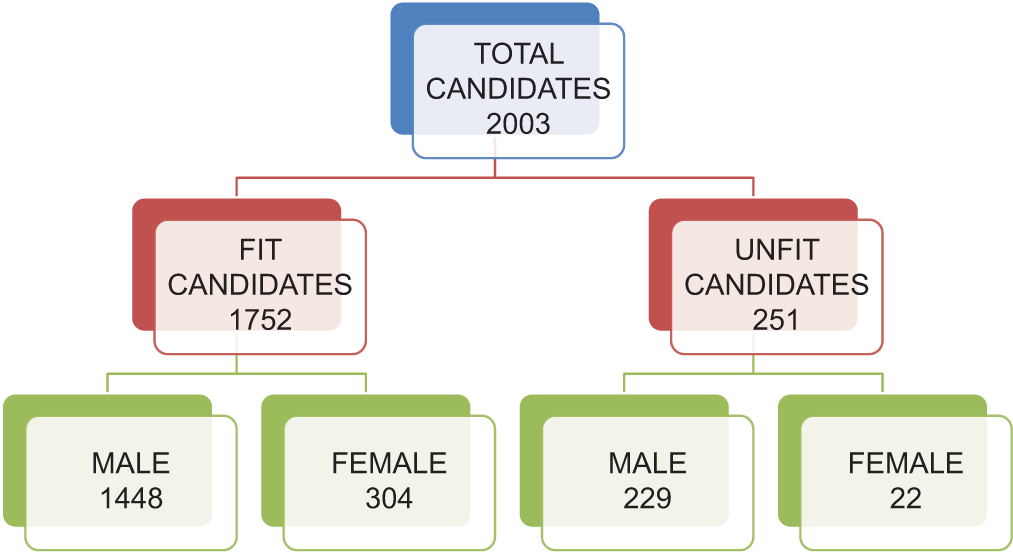
- Distribution of fit and unfit candidates.
| Parameters | Total no of candidates and overall unfit percentage (out of 2003 candidates) n (%) |
Percentage of unfit (out of 251 unfit candidates) n (%) |
|---|---|---|
| Substandard vision/refractive error | 128 (6.39) | 51 |
| Lattice degeneration | 37 (1.85) | 14.74 |
| Defective color perception | 25 (1.25) | 9.96 |
| Post-kerato-refractive surgery | 21 (1.05) | 8.37 |
| Cataract | 11 (0.55) | 4.38 |
| Squint | 6 (0.3) | 2.39 |
| Other causes | 23 (1.15) | 9.16 |
| Total unfit | 251 |
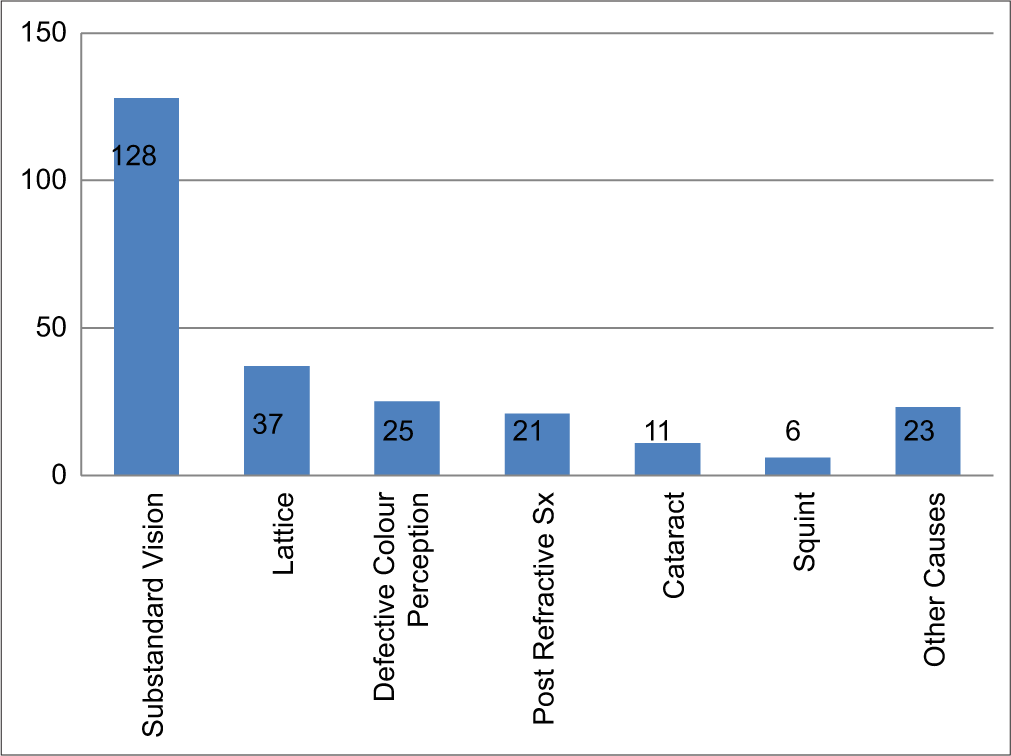
- Number of unfit candidates in various ocular conditions.
Substandard vision
Substandard vision was the most common cause of rejection in the candidates. As many as 128 candidates out of 251 were rejected due to not meeting the prevailing standards of various branches of the Air Force accounting for 51% of the unfit candidates (half of unfit candidates). These candidates had applied for various branches of the Air Force. If we look at the overall prevalence in this small group of aspiring candidates, it is 6.39%. A breakdown of myopia errors is given in Table 2. A large data from 59 quality-assessed studies, covering nearly 1,66,000 urban and 1,20,000 rural children showed the overall crude prevalence of myopia over the last four decades is 7.5% (95% confidence interval, 6.5–8.5%) in the 5–15-year age group.[2] Our study has shown a slightly decreased prevalence as in some streams myopia <3.50D is allowed for initial entry to the Air Force, also the age of the candidates included in the study was more than 17 years.
| Myopia | Total unfit myopic candidates (n=128) |
|---|---|
| Till-2.0D | 107 |
| -2.0D to-3.50D | 14 |
| More than-3.50D | 02 |
| Hypermetropia | 02 |
Lattice degeneration
About 37 (1.85%) candidates were detected to have lattice degeneration with high-risk factors (more than 3 clock h, multiple lattices, lattice with hole, and myopia or history of myopia). Lattice degeneration is present in 6–8% of the general population.[3,4] In our study, we have included only those candidates who have lattice degeneration with high-risk factors and are associated with retinal holes. This might be the cause of the low incidence of lattice degeneration in our study.
Defective color perception (CP)
About 25 (1.25%) candidates were found to have defective CP according to their chosen stream of Armed Forces. Color vision was done as per the standard laid down procedure.[1] Martin Lantern test was used to define CP 1. CP II was quantified using Ishihara charts (38 plates), and again the Martin Lantern test was used to differentiate between CP III and CP IV. In India, the prevalence of color vision deficiency (CVD) is found to be 2.76–4.06%.[5,6] However, in these studies,[5,6] authors have used Dalton pseudo isochromatic plates as the primary screening method followed by confirmation by Ishihara plates. It is further noted that a normal trichromat person might miss a few plates at the first reading,[7] so these tests are also not error-free. None of the female candidates were found to have color vision deficits leading to their rejection.
Post-kerato-refractive surgery
Candidates who undergo refractive surgeries (SMILE/LASIK/PRK) except Radial keratotomy are been permitted in various branches of the Air Force including the flying branch, However, they need to fulfill some laid down criteria.[1] Twenty-one candidates with post-refractive surgery were declared unfit due to not fitting in one or more laid down criteria (axial length >26 mm, corneal thickness more than 450 μm, 1-year post-procedure, pre-operative myopia more than 6D) amounting to 1.05% of the total candidates. It also needs to be noted that most individuals underwent kerato-refractive surgeries just to clear medical examinations. Unfortunately, some candidates were not aware of the fitness criteria following refractive surgeries.
Cataract
Eleven candidates were detected to have significant cataracts affecting the visual axis accounting for 0.55% of the total candidates. These cataracts were affecting the best corrected visual acuity. Out of 11 cataracts, three had some history of blunt trauma in the past leading to visually significant cataracts. Trauma is one of the important factors associated with the development of cataracts.[8] Candidates with congenital lenticular opacities (e.g., blue dot cataracts) not affecting the central vision/central field were made fit as per guidelines.
Squint
Six candidates (0.3% of total candidates) were found to have significant squint as examined by the cover, alternate cover, cover-uncover, Maddox rod, and Prism bar cover test. Individuals found to have tropics (esotropia or exotropia) were made unfit. Cases with uniocular suppression, and hypo/hyperphoria more than 2D were made unfit. Similarly, exophoria with more than 6 PD at 6 m and more than 16 PD at 33 cm, and esophoria greater than 6 PD at 33 cm and 6 m were made unfit. One case of congenital superior oblique palsy was also detected.
Other causes of rejection
Keratoconus, corneal opacities affecting the central vision, disc suspect, and abnormal retinal pathology were other important factors for rejection [Table 3].
| Other causes | Number |
|---|---|
| Keratoconus | 04 |
| Corneal opacities affecting central vision | 03 |
| Juvenile glaucoma | 01 |
| Retinal periphlebitis | 01 |
| Fundus coloboma | 02 |
| Anisocoria | 02 |
| Ptosis | 03 |
| Nystagmus | 01 |
| Familial dominant drusen | 01 |
| Cranial nerve palsies | 01 |
| Multifocal choroiditis | 01 |
| Total | 23 |
DISCUSSION
Aspiring for a career in the Armed Forces and putting dedicated efforts later converting into rejection during the medical examination can be the cause of despair and concern to the desirous aspirant. Ophthalmic conditions are the leading cause of rejection in the entry to the Armed Forces. Substandard vision remains the leading cause of rejection into the Armed Forces. We have seen myopia becoming one of the major concerns in the post-COVID era.[9,10] Authors are skeptical of getting candidates with unaided vision 6/6 in the future for flying branches. One of the commonly ignored methods is color vision testing in school-aged children. To determine the prevalence of this disability in India, the largest study on CVD in children is being done and it shows significant CVD in boys and further emphasizes the early screening of CP.[5,11] Trauma to the eyes is another area of concern. Candidates who suffered minor blunt trauma in childhood and had never been examined by an ophthalmologist, either due to normal visual acuity of other eyes, lack of awareness, or non-availability of periodic screening protocols at school were found to have ill effects of trauma which were detected in the detailed workup during the medical examination.[12] An early ocular examination at the stage of choosing career options can prevent a majority of these people from applying for such career options, where strict medical standards can lead to rejection in medical examinations. These individuals can either opt for different career options beforehand or get treated for ocular conditions resulting in saving their efforts and achieving excellence in those streams. Technological advancement and ease of learning through digital screens have also increased the prevalence of myopia among children,[13] especially during COVID-19 times, its long-term effects will be seen at least after 8–12 years. Policymakers should accordingly modify the ophthalmic standards for ease of the selection process.
CONCLUSION
The authors suggest that every individual must undergo a thorough medical examination at around 14–16 years of age equating to 10–12 standard during their school time. Ideally, it should be made mandatory to submit a detailed medical examination including one comprehensive report on eye examination before they go for their secondary/senior secondary board examinations at the center as well as state level. This could be of great help to the individuals as it can lead to optimum career selection and thus fruitful results. It would also save man-hours in recruitment centers or referral centers in terms of time involved in the examination of these candidates according to branch-specific medical standards of armed forces or civil aviation. If they had known beforehand that their condition might later be a cause of rejection/non-selection in armed forces or aviation, their efforts could have been aligned to a different stream altogether or alternate career options. We could not find any such study with a large sample size on the analysis of major ocular conditions leading to rejection in the Air Force aspirational candidates in the Indian subcontinent.
As a way forward authors also tied up with local school authorities to increase awareness about common ophthalmic pathologies and periodic ocular screening, especially for children from class 9th–12th (which are most crucial for future prospects) along with the early screening of color vision defects.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient consent was not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Manual of medical examination and medical boards In: IAP 4303 (5th edition). New Delhi: Air HQ; 2020.
- [Google Scholar]
- Prevalence of myopia in Indian school children: Meta-analysis of last four decades. PLoS One. 2020;15:e0240750.
- [CrossRef] [PubMed] [Google Scholar]
- Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachment. Cochrane Database Syst Rev. 2014;2014:CD003170.
- [CrossRef] [Google Scholar]
- Posterior vitreous detachment, retinal breaks, and lattice degeneration preferred practice pattern®. Ophthalmology. 2020;127:P146-81.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of color vision deficiency among school-going boys in South India. Indian J Ophthalmol. 2021;69:2021-5.
- [CrossRef] [PubMed] [Google Scholar]
- Red-green color vision deficiency and lack of awareness among rural school students in India. Iran J Public Health. 2015;44:1018-20.
- [Google Scholar]
- Efficiency of the Ishihara test for identifying red-green colour deficiency. Ophthalmic Physiol Opt. 1997;17:403-8.
- [CrossRef] [PubMed] [Google Scholar]
- Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139:293-300.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of myopic progression before, during, and after COVID-19 Lockdown. Ophthalmology. 2021;128:1655-7.
- [CrossRef] [PubMed] [Google Scholar]
- Revisiting color vision standards and testing methods in various occupational groups. Indian J Ophthalmol. 2022;70:329-31.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior segment consequences of blunt ocular injury. Br J Ophthalmol. 1982;66:549-55.
- [CrossRef] [PubMed] [Google Scholar]
- Association between digital smart device use and myopia: A systematic review and meta-analysis. Lancet Digit Health. 2021;3:e806-18.
- [CrossRef] [PubMed] [Google Scholar]







