Translate this page into:
A unique case of inability to view the Head Up Display (HUD) in a fighter aircraft
Abstract
A 28 year old serving naval aviator was referred to IAM for evaluation as he had difficulty in reading the Head up Display (HUD) in the simulator during his conversion training to a Sea Harrier which necessitated a referral to IAM for evaluation. Despite his refractive correction, the pilot continued to state his inability to read the letters of the HUD in the cockpit. This then set the stage for a comprehensive evaluation at IAM. During evaluation, all the objective tests were normal but the tests which depended on the pilot’s subjective responses were inconsistent and later logically examined to be improbable. The pilot was given a diagnosis of “Subjective Visual Disturbance”. This singular case of the hitherto unreported vague symptom of not being able to read the HUD symbology posed an aero medical predicament. This triggered a cascade of investigations and examinations in which the path of vision from the cornea to the occipital lobe was thoroughly investigated. All the measurable and quantifiable determinants of vision like refraction, visual acuity, colour vision, illumination, contrast sensitivity, visual fields, the visual pathways and the interplay between human vision and the HUD were explored in order to arrive at the appropriate aero medical decision. This case highlights the presence of a psychological overlay always suspected but never proven - a case of ‘will not see’ rather than ‘cannot see’.
Keywords
HUD
Subjective visual disturbance
aero medical predicament
A 28 year old serving naval aviator was referred to IAM for evaluation as he had difficulty in reading the Head up Display (HUD) in the simulator during his conversion training to a Sea Harrier, a Vertical Short Take Off and Landing aircraft (VSTOL). His prior flying experience was 391 Hrs 45 min on the basic piston trainer, the basic jet trainer, a Mig 21 variant and the Chetak helicopter. In his flying career this was his first exposure to a HUD. On evaluation by the ophthalmologist in the field, he was detected to have myopia and therefore in view of his peculiar situation of being a myopic during his conversion training, it further necessitated a referral to IAM for evaluation.
At IAM he was found to have a slightly myopic refraction which improved fully with the prescribed correction. His colour vision, contrast sensitivity and rest of his ophthalmic evaluation was normal. After correcting his myopic refraction, the pilot underwent a field trial at ASTE on a Jaguar aircraft with a similar HUD where the pilot continued to state his inability to read the letters of the HUD in the cockpit. This then set the stage for a comprehensive evaluation at IAM.
The pilot underwent a recheck of his refraction, colour vision and a repeat ophthalmological assessment including a Neuro-Ophthalmological assessment at a tertiary ophthalmic centre. It was noted that while the objective tests performed on the pilot were normal, the subjective tests namely the contrast sensitivity test and the visual fields tests which depended on the pilot’s responses had subnormal results. These inconsistencies in the pilot’s subjective responses prompted the need for psychometric evaluation which was found essentially normal..
The pilot was given a diagnosis of “Subjective Visual Disturbance”; placed in a non-flying medical category for a duration of 12 weeks and was instructed to report back to IAM with a review and opinion by Senior Advisor (Ophthalmology).
The pilot reported back to IAM after duration of 12 weeks of non-flying medical category with the opinion of the Senior Advisor (Ophthalmology) who found the pilot’s ophthalmological assessment normal and recommended that he be upgraded to unrestricted flying status.
During this second review at IAM, the pilot reported a complete resolution of his symptoms as he had continued training on the simulator with executive clearance wherein he stated a definite improvement in his ability to see the symbols and letters on the HUD which he ascribed to the multivitamins he was prescribed by the neuro ophthalmologist. Interestingly, he also came up with a previously unmentioned history of having taken Isotretinoin capsules for a couple of months for acneiform lesions about six months previous to his initial difficulty on the HUD during his conversion training
He again underwent a comprehensive ophthalmic evaluation for his refraction, colour vision, contrast sensitivity and visual fields which were found to be completely normal except for the previously detected myopia which was stable and did not show any progression. The pilot underwent a repeat trial on the HUD at ASTE with his spectacle correction and he was able to correctly identify all the letters and symbols on the HUD. Therefore in view of the normal review report of the Senior Advisor (Ophthalmology), the normal ophthalmological reassessment at IAM and a complete resolution of the pilot’s symptoms, he was upgraded to a full unrestricted flying category.
Analysis of the pilot’s symptoms
The inability of the pilot to see the HUD was a unique symptom not encountered before in the authors’ experience. A review of literature did not reveal any similar case. On objective analysis of the pilot’s symptoms at presentation, prima facie three possible causes that might have been contributory were required to be examined namely the refractive error, the colour vision and lastly the contrast sensitivity.
Evaluation of refractive error as a cause of the pilot’s symptoms
To evaluate the possibility of refractive error, the pilot was taken to a cockpit of an aircraft with a similar HUD in a field trial wherein the height of letters (4mm) on the HUD which the pilot reported he could not see and the distance of the pilot’s eye from the HUD (470 mm) were used to derive the visual angle that those letters subtended on the pilot’s eye [Figure 1, Table 1], The visual angle in this case was 29.2 min arc. For any letter to be seen by the human eye it has to subtend a minimum angle of 5 min arc and in this case the letters which the pilot purported he could not see were in fact subtending a visual angle approximately six times the minimum. The inability to see these letters would have meant that the pilot had a Snellen’s VA of 6/ 36. Objectively, this was not the case because the pilot had a 6/6 vision with his correction for myopia. Therefore the possibility of refractive error contributing to the pilot’s symptoms was ruled out.
Calculation of letter height
|
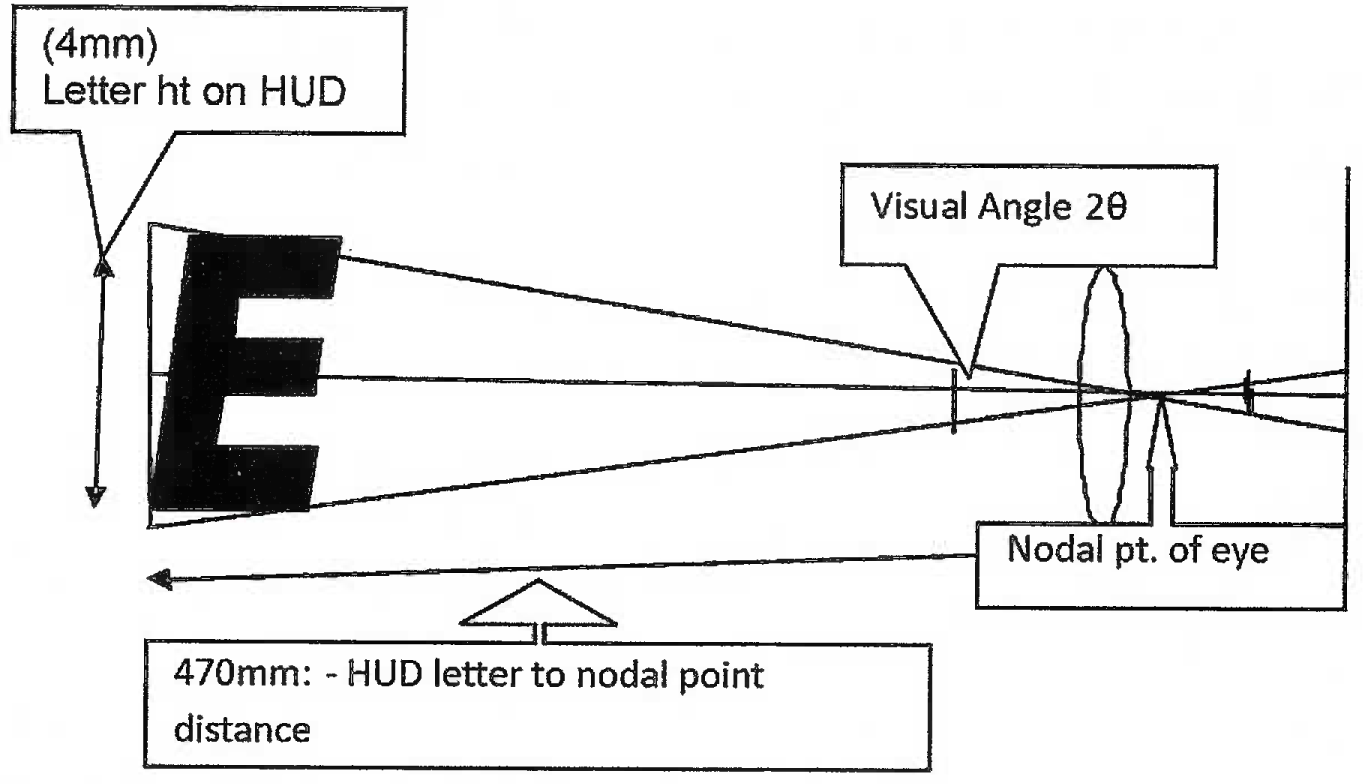
- Schematic representation of calculation of the visual angle subtended by letters of the HUD during the field trials
Evaluation of defect in colour vision as a cause of the pilot’s symptoms
The next possibility evaluated was for a defect in colour vision. The pilot was assessed with the Ishihara’s pseudoisochromatic chart and the Martin Lantern Test (MLT) at IAM which test for congenital red-green blindness. In order to exclude the possibility of blue colour defect the patient was subjected to the Farnsworth Munsell B-15 test at the tertiary care ophthalmology centre. The D-15 test allows detection of red, green and blue colour defects [1]. The test consists of sixteen different colored caps numbered from 0-15 on the reverse, with the first cap being the reference colour placed in a rack following which the other 15 randomly shuffled caps have to be arranged by the patient according to the logical colour sequence. The results thus obtained are plotted on a score sheet which can identify red, green or blue colour defects. In the present case, the colour of the symbols /letters on the HUD were green against the transparent background of the combiner glass of the HUD and were of adequate luminance with adjustability as per standards. The pilot thus being investigated for his colour vision was found to be normal and colour vision defects as a cause of his symptoms were excluded.
Evaluation of defect in contrast sensitivity as a cause of the pilot’s symptoms
Finally the possibility of a problem in the contrast sensitivity function of the pilot was considered. Simply stated, contrast sensitivity refers to the ability to perceive differences between an object and its background. It enables one to perceive two separate regions with different luminosities without distinct borders [2].
Visual acuity measurement in the clinic by the Snellen’s chart uses high contrast optotypes i.e. black letters on a white background. In real life, objects and their surroundings are of varying contrast, therefore visual acuity as tested by the Snellen’s’ opto types only represent one end of the spectrum formed by varying contrast levels i.e. one point on the contrast sensitivity function plot. The clinical testing of the ability to detect contrast across a range of contrast differences and across a range of spatial frequencies allows a more detailed understanding of a person’s visual capabilities [3,4].
Contrast sensitivity gives us a complete quantification of a person’s functional acuity. It is measured by instruments like the CSV -1000 (available at IAM),Pelli Robson Chart, Vistech chart, FACT chart etc (Figure 3).
The contrast sensitivity plot has different spatial frequencies on the x axis and the varying contrast levels on the y axis. The ability of the subject to discern the different grating frequencies in cycles per degree (CPD) across varying contrast levels gives us a plot which should be within the prescribed normogram .
In this case the pilot stated that he could not make out certain letters/symbols on the HUD in the jaguar aircraft used in the trial at ASTE. In order to evaluate contrast sensitivity as a cause of the pilot’s symptoms it was necessary to calculate their spatial frequency value in Cycles Per Degree (CPD) being subtended on the nodal point of the pilot’s eye. The line width of each symbol of the HUD is 1.7 min of an arc as per standards [5]. The HUD symbology’s line width in min arc was converted to Cycles Per Degree (CPD) to obtain their contrast spatial frequency which was 17 CPD as per the calculation depicted (Table 2).
The alleged inability to see the HUD symbology subtending a spatial frequency of 17 CPD meant that the pilot should have had contrast sensitivity plot showing a select deficit at or around 17 CPD on as tested on the CSV-1000 at IAM and the FACT chart at the tertiary ophthalmic centre, which however was not the case.
CALCUATIQN (relating min of arc of Mil Std I to Cycles/deg of contrast)
|
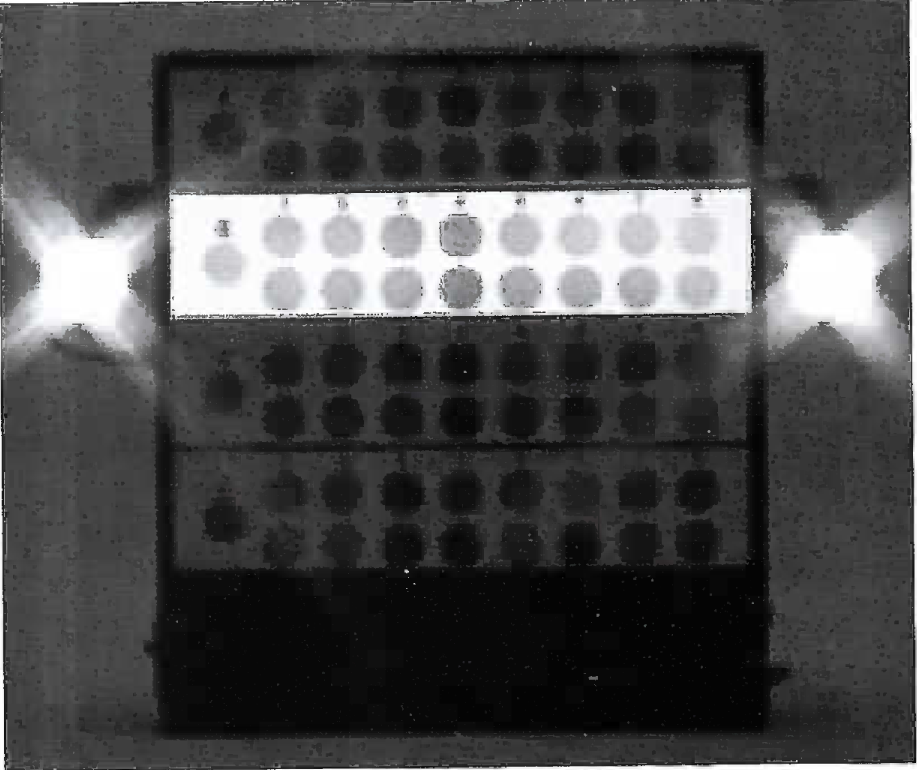
- CSV 1000 equipment for Contrast sensitivity function testing
The pilot’s responses on the CSV -1000 contrast sensitivity tester showed grossly depressed contrast sensitivity across all spatial frequencies instead of a select deficit at or around 17 CPD [Figure 3]. These grossly decreased results across all spatial frequencies did not clinically corroborate with pilot’s normal ophthalmological assessment. His contrast sensitivity results suggested that the pilot should have had a very poor functional visual acuity of 6/24 or worse and/or a pathology in his eye and his visual pathways. Such results implied the pilot should have had significant problems with his activities of daily living on ground, not to mention the prospect of flying, impossible. Moreover these improbable grossly depressed contrast sensitivity results were in contradistinction to those of the pilot tested a fortnight back on his initial presentation at IAM which was within normal limits I Figure 4]. In the final analysis, keeping in mind chat the contrast sensitivity test is primarily a subjective test that depends on the pilot’s responses and the reasons for the improbability of the results in this case as discussed above, it was decided to disregard the results of the contrast sensitivity tests in this particular case.

- Grossly depressed contrast sensitivity function report across γ·1 spadal frequencies.
Evaluation of Neuro-ophthalmological pathways as a cause of the pilot’s symptoms
In order to evaluate the pilot’s inability to view the HUD, a detailed elecirophy Siological assessment of his visual pathways was necessary for which the pilot was referred to a Neuro-Ophthalmologist at a tertiary ophthalmic centre. There his colour vision assessment (Farnsworth Muriseli test D-15), high definition MRI (of orbits and bram delineating the visual pathways), Visual Evoked Potential (VEP) ,Electro RetinoGram (ERG), Multifocal ERG, Contrast sensitivity (Functional Acuity Contrast Tester)and Visual Fields (30-2 static perimetry) were done it was noted that while the objective tests(MRl,VEP,ERC) performed on the pilot were normal ,the subjective tests namely the contrast sensitivity test and the visual fields tests which depended on the pilot’s responses had subnormal results. The visual field results were inconsistent in that a few paracentral scotomas were seen initially in the right eye and then in the left eye on repeat testing. Moreover the contrast sensitivity results done both at the tertiary level ophthalmic centre and when repeated at IAM were grossly subnormal which was very surprising considering the fact that he had a perfectly normal result in the initial test conducted at LAM just a fortnight back. Thus considering the above facts his neuro-ophthalmological status was found normal and was not responsible for his symptoms.
- Normal contrast sensitivity report of pilot on initial presentation at IAM.
Evaluation of Psychological reasons as a cause of the pilot’s symptoms
The vague unreported symptoms and the inconsistencies in the pilot’s subjective responses on evaluation and the non corroboration of the pilot’s symptoms with his normal ophthalmological assessment prompted the need to consider other relevant aspects of the pilot’s history. The unfortunate demise of his instructor on the same Hamer aircraft a fortnight before the pilot’s training commenced might have raised concerns regarding the safety record of the Harrier in the pilot’s mind. Moreover the pilot had a younger sibling undergoing treatment for leukemia. Therefore in order to exclude a functional overlay it was recommended that the pilot undergo psychometric evaluation.
The psychologist opined that the pilot was essentially normal with a good motivation for flying and had no underlying psychological abnormality. The psychologist’s opinion notwithstanding, in view of the lack of clincoinvestigative corroboration for the pilot’s enduring but improbable symptoms, the question that emerged was whether this was a case of ‘cannot see’ or ‘will not see’ . The nature of functional overlay if any could not be ascertained in this case.
Evaluation of isotretinoin capsules ingestion as a cause of the pilot’s symptoms
The pilot on his second review volunteered a previously unmentioned history of having taken Isotretinoin capsules for a couple of months for acneiform lesions about six months previous to his initial difficulty on the HUD during his conversion training. This history however was not furnished on his initial visit to IAM despite being specifically questioned on this aspect. The side effects of isotretinoin ingestion taken for the treatment of keratinization disorders can have varied ophthalmological side effects including conjunctivitis; corneal opacities; cataracts; dry eyes; contact lens intolerance; decreased night vision; visual disturbances including pseudo tumor cerebri or papilledema [6]. The visual disturbances experienced did not show any clinical correlation and no evidence of any anomaly was present on the ophthalmological assessment of the pilot at IAM. The possibility of a transient drug related disturbance in the past with recovery was duly considered but was discounted given the fact the pilot continued to be symptomatic during his first evaluation at IAM which did not reveal any abnormality whatsoever. As there was no objective evidence to support the possibility, it was decided to disregard this history of isotretinoin capsule ingestion as a cause of the pilot’s symptoms.
Aeromedicai decision making-First Review
Keeping the above clinical facts in mind, the aero medical decision making in this case hinged on the following issues:
(a) Could the individual have been considered fit to fly at that stage?
(b) If fit, should he have been cleared for restricted or unrestricted flying? [A1/A3 category respectively].
(c) If unfit for flying-should he have been given temporary or permanent category? [A4 (T)/ A4 (P) respectively].
At that point in time, since the pilot was symptomatic, he could not be cleared for unrestricted flying [Al category].
However the option of restricted flying [A3 category] was seriously considered since the clinical evaluation and investigations had revealed no abnormality and the psychological evaluation was normal. It was felt that an executive report of inflight visual performance would enable a more informed decision in a subsequent review. If the contrast sensitivity abnormality was to be taken at face value, the pilot would have been unfit for aviation duties of any kind. In such a case compatibility with military duties would have needed a complete reassessment keeping in mind his ability to spot targets and perform other military duties.
However, since the supportive opinion of the Senior Advisor (Ophthalmology) was not available and the variable results of the contrast sensitivity continued to influence the aero medical decision making, it was decided to observe the individual in nonflying /ground category A4 (T).
Aeromedicai decision making-Second Review
During the pilot’s second review, in view of his complete symptom resolution, the recommendation to be upgraded by the senior advisor and a completely normal ophthalmological reassessment, the pilot was upgraded to a full unrestricted flying category [Al].
Conclusion
This singular case of the hitherto unreported vague symptom of not being able to read the HUD symbology posed an aero medical predicament. This triggered a cascade of investigations and examinations in which the path of vision from the cornea to the occipital lobe was thoroughly investigated. All the measurable and quantifiable determinants of vision like refraction, visual acuity, colour vision, illumination, contrast sensitivity, visual fields, the visual pathways and the interplay between human vision and the HUD were explored in order to arrive at the appropriate aero medical decision. This case highlights the presence of a psychological overlay always suspected but never proven - a case of ‘will not see’ rather than ‘cannot see’.
The aim of presenting this case was to demonstrate the objective approach which needs to be embarked upon in such circumstances. It sensitises the aero medical fraternity to exercise due caution and diligence on having to evaluate vague and unique symptoms and histories elaborated by an increasingly aware, intelligent and imaginative client population.
References
- Colorvision In: Tasman William, Jaeger Edward A, eds. Duanes Ophthalmology. Ed. Lippincott Williams & Wilkins; 2007. 2007. p. :1470-1484. in:
- [Google Scholar]
- The Contrast Sensitivity Function. Available from: Uri: http://vision.psy.mq.edu.au/~peterw/csf.html
- MIL-STD-1472F23. Aug 1999; Department of Defense, Design Criteria Standard Human Engineering JJSA
- A to Z Drug Facts 2003. Ed. Lippincott Williams & Wilkins; 2003. p. :734.






