Translate this page into:
Electrocardiographic Abnormality in Air warrior: Acute MI
Case Report
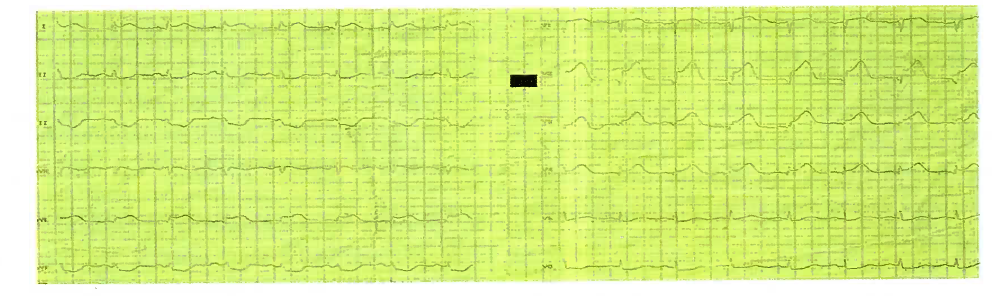
A 54 years old serving male was transferred to our hospital accompanied by a medical officer from a peripheral location, with history of acute onset precordial chest pain of 02 hours duration. The pain was radiating to his left upper arm. There was no history of palpitation, syncope or any other premonitoring symptom. He was not a known case of Diabetes mellitus or hypertension. There was no history suggestive of past ischemic episode. He had no reversible or modifiable cardiovascular risk factors. He was assessed clinically and was found to be hemodynamically stable and normotensive. He was looking anxious and having diaphoresis. On auscultation, the SI & S2 were faint and no 3rd & 4th heart sound or murmur was heard. He was euglycaemic. He admitted being under stress over his sons career prospects and admission to a professional college. During the management of case this ECG was obtained.
Questions:
QI. What does the ECG show?
Q2. What is your diagnosis?
Q3. How is this pathology produced?
Q4. What further investigations will you do?
Q5. What is the aeromedical concern?
Answers:
-
The conventional 12 lead ECG shows:
ST Elevation in lead V2 / V3 / V4,I & AVL
Increased Ventricular Activation Time (VAT)
Normal Axis and Rhythm
Reciprocal changes in Inferior leads i.e.ST/T depression in II, III & AVF.
Tall ‘T’ waves in V2 - V4.
The diagnosis is Hyper Acute ST Elevated Anterior Septal Wall Myocardial Infarction with no evidence of arrhythmia.
-
The hyper acute phase of Myocardial Infarction (MI) before fully evolved phase occurs normally within a few hours of the infarction. The term itself conveys critical connotation of this phase. This phase is characterized by 04 principal ECG manifestations in leads which are oriented to the infarcted surface. These changes are:
Increase VAT - i.e. the time from the beginning of QRS complex to the apex of the R- wave. In MI VAT is delayed beyond 0.45 sec.
Increased Amplitude of the R- wave- The R wave becomes taller than normal due to acute injury. Since this part is not yet necrosed and is therefore still able to conduct the electrical conduction but at a slower rate. This slower conduction time is reflected by ‘! VAT.
Slope ST Elevation Segment - This is the most noticeable and characteristic feature of hyper acute phase of MI. This ST segment may blend with and constitutes the proximal limb of tall and widened T wave.
Tall and widened T Wave - Sometimes it becomes taller than amplitude of the R- wave and its proximal limb constitutes the S-T segment. This may occasionally be the dominant feature of hyper acute phase of MI.
-
A 12 lead ECG forms the basis for the diagnosis. It is important to note that similar ST segment ECG findings can occur in the following conditions;
Coronary Vasospasm.
Organic stenosis of coronaries.
Left Ventricular Aneurysm.
Closed Cardiac Massage / Trauma.
Impaired Left Ventricular Function with old MI.
Left Bundle Branch Block.
Acute Pericarditis.
However in this clinical setting, the ECG is diagnostic itself. In difficult cases a repeat of such ECG after 1-2 hours duration will be of immense help, especially in this setting when patient had presented early. Without wasting further time patient should be treated with Emergency Percutaneous Coronary Intervention (PCI) or thrombolysis. In addition Ecospirin, Clopidogrel, Morphine, Nitrates, Statins, Beta blockers, ACE inhibitors should be promptly exhibited. Even in the peripheral set up such diagnosis should not be missed and timely treatment should be started. However once the patient is stabilized he can be referred to higher center for further evaluation and prognostication. In today’s practice early PCI is the best treatment and ideally be offered within 03 hours of onset. Since PCI requires a bigger set up second best option is thrombolysis by using either TPAor Streptokinase.
Acute MI is the commonest cause of death which can occur at any time without giving any forewarning. Therefore, a high index of suspicion should always be kept. Every medical personnel should be trained to diagnose and handle this disease for saving life. Acute MI Also happens to be an important cause for In-flight incapacitation. The medical personnel 'should be proficient in identifying the signs preceding and during a cardiac event. The management requires skill and practice of dealing such cases. In this case being located in a periphery it was required to shift such cases at the earliest to preferably a cardiac centre where a PCI or thrombolysis could be offered. The time saved is the myocardium saved and probably due to a quick response in shifting this patient resulted in saving a precious life. It normally takes a minimum 06 weeks for the damaged myocardium to recover and for the scar to get healed. Therefore, after an initial rest period, a TMT would help in further risk stratification of such cases. Such patients usually require lifelong medications so reversion to full flying duties would solely be decided on the recovery pattern to fully functional cardiac status.





