Translate this page into:
Electrocardiographic Abnormality in Aircrew Apical Hypertropic Cardiomyopathy
-
Received: ,
Accepted: ,
A 22 years old candidate reported for his class I civil medical examination. He had no complaints to offer and denied history of shortness of breath, loss of consciousness, effort intolerance or chest discomfort. There was no family history of any cardiovascular ailment or sudden cardiac death. The general and systemic examination was normal. As a part of mandatory examination protocol a 12 lead electrocardiogram was taken (Figure 1).
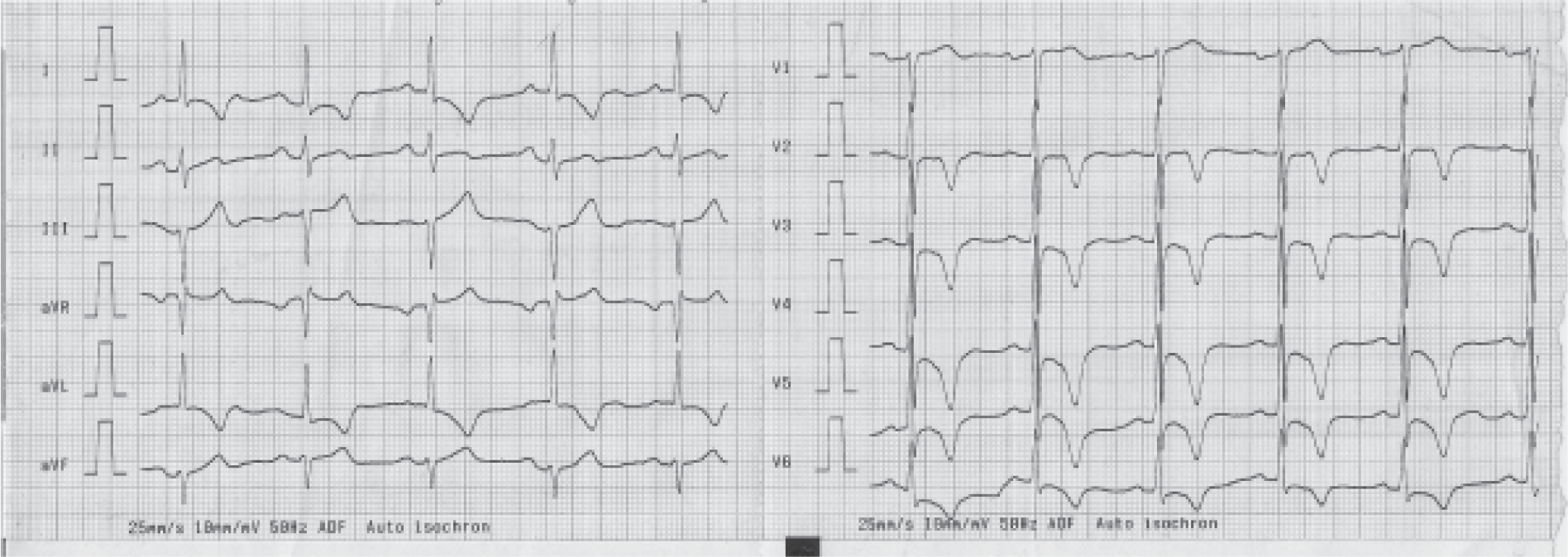
- An ECG of an candidate for civil aircrew duties
Questions:
What does the ECG show?
Describe the normal T wave? What are the common causes for T wave inversion?
How will you investigate this candidate?
What is hypertropic cardiomyopathy?
What are the aeromedical concerns in this candidate?
What is the aeromedical disposal of this candidate? What counseling will you give to this candidate?
Answer 1. The 12 lead electrocardiogram shows the following:-
The P wave and the PR interval is normal
The frontal plane QRS axis is directed to -45 degree (left axis deviation)
There is counter-clockwise electrical rotation (the transition zone is situated at lead V2)
Tall R waves in lead V4 and V5.
No ECG evidence of left ventricular hypertrophy or strain.
Symmetrical, sharp, pointed, and inverted T waves in lead I, aVL, V2 to V6.
Answer 2
The normal T wave is an asymmetrical wave with a shallow proximal limb, blunt apex and a steep distal limb. T waves do not usually normally exceed 0.5 mV in any limb lead or 1.5 mV in any precordial lead. With age there is a tendency for the T wave amplitude to diminish. It is usually inscribed in the same direction as the QRS complex. Just as not all ST segment elevation reflects ischemia, not all T wave inversion is abnormal. For example T wave inversion may be seen normally in lead with negative QRS complex (aVR). In adults the T wave may be normally negative in lead V1 and some times also in lead V2. Non-specific T wave abnormality may also be seen under circumstances like anxiety, fear and in response to hyperventilation and orthostatic changes.
Some common etiology for the T wave inversion are as follows:-
Persistent juvenile pattern: It is a normal variant and denotes persistence of inverted T waves in lead V1 to V3 (V4) of infancy in to adulthood.
Coronary heart disease
Sub-acute or old pericarditis
Myocarditis
Cardiomyopathy
Intracranial hemorrhage
Myocardial contusion
Acute pulmonary embolism
Electrolyte disturbances (hypocalcemia)
Drug toxicity (digoxin, quinidine and phenothiazide toxicity)
Answer 3
This young candidate with pathological electrocardiographic changes needs evaluation directed towards assessment of structural and functional aspect of his heart. He also needs reassessment for modifiable coronary risk factors. The candidate was thus subjected to additional tests. The assessment of the structural component was done using echocardiography, which revealed localized wall thickening confined to the distal left ventricular chamber (apical hypertropic cardiomyopathy). There was no structural abnormality of the mitral valve apparatus and the left ventricular outflow tract did not showed any obstructive pathology. Tissue Doppler interrogation did not revealed any evidence of diastolic dysfunction. The stress test for the candidate was normal and there were no modifiable coronary risk factors. He was thus diagnosed as a case of non obstructive hypertropic cardiomyopathy.
Answer 4
Hypertropic cardiomyopathy is the most common genetic cardiovascular disease with a reported prevalence of 0.2% in general population. It results from a multitude of mutation in gene encoding proteins of cardiac sarcomere. The diagnosis depends on demonstration of left ventricular hypertrophy with out the cavity dilatation, in the absence of any cardiac or systemic disease. The main pathophysiological feature of hypertropic cardiomyopathy is diastolic dysfunction which is a consequence of impaired relaxation and distensibility. The systolic function is often normal.
The ventricular hypertrophy in hypertropic cardiomyopathy may affect one or more of the following regions:-
Interventricular septum.
Left ventricular free wall
Apical and paraseptal region
Right ventricle
ECG is abnormal in almost 85% cases of hypertropic cardiomyopathy and often provides the first clue to the probable presence of underlying disease in an apparently asymptomatic individual. The ECG manifestations of septal hypertrophy includes increased magnitude of septal vector manifesting as prominent deep and narrow Q waves in the infero-lateral leads; left ventricular free wall hypertrophy manifests as classic left ventricular hypertrophy with systolic strain pattern, while apical and paraseptal ventricular hypertrophy reflects on ECG as tall R wave with deep T wave inversion in the mid precordial lead (V2 to V4). There is often an associated counter-clockwise electrical rotation with shifting of transition zone to the right precordial lead.
Answer 5
The aeromedical concerns in cases of hypertropic cardiomyopathy are on account of the disease itself and the unpredictable and variable natural history of the condition. The patient may remain stable over a long period of time and may manifest symptom during any phase of life from infancy to old age. The main aeromedical concerns are
Sudden cardiac death
Risk of atrial fibrillation and its complications (embolic stroke and heart failure)
Progressive heart failure.
Sudden cardiac death commonly occurs during adolescence and young adulthood and is often the initial manifestation in an otherwise asymptomatic individual. It thus poses significant risk to the flight safety. Thought it is not possible to quantify the absolute risk of sudden cardiac death in a case of hypertropic cardiomyopathy, the risk increases in presence of any of the following factors:-
Prior cardiac arrest or sustained ventricular tachycardia
Family history of one or more premature hypertropic cardiomyopathy related death.
Syncope, especially in young and related to exertion
Hypotensive blood pressure response to exercise
Multiple, repetitive or prolonged non sustained ventricular tachycardia on serial Holter monitoring.
Massive left ventricular hypertrophy (wall thickness of more than 30mm)
Answer 6
Candidates with underlying structural heart diseases are unfit for flying duties. Though not mandatory, the best medical practice dictates that the individual though unfit, be counseled about his condition. The candidate needs to be explained the nature of his disease and its implication. He also need to be explained the genetic nature of the disease and the need for prospective screening of all the family members for hypertropic cardiomyopathy. The prospective screening of the family members is carried out by 12 lead electrocardiogram, echocardiography and DNA analysis. Serial echocardiography on yearly basis, starting from the age of 12 years till the age of 18-21 years is advised for all first degree relatives. After the age of 21 years, though not mandatory it is desirable that screening echocardiography be continues at five yearly interval.





