Translate this page into:
Hyperbaric Oxygen Therapy in Management of Mandibular Osteoradionecrosis: A Success Story at Institute of Aerospace Medicine, Bangalore
Abstract
Osteoradionecrosis (ORN) is a known complication in patients who are treated with radiation therapy for head and neck cancer. Over the years, hyperbaric oxygen therapy (HBOT) has been used as an adjunctive treatment for ORN with improved success rates. The following report gives an account of a 55 years old lady, a case of right mandibular ORN managed with 20 sessions of HBOT at the Institute of Aerospace Medicine (IAM). The healing is evident in the form of subjective resolution of symptoms as well as objective i.e. radiological findings.
Introduction
Osteoradionecrosis (ORN) is defined as an area of exposed, devitalized, irradiated bone that fails to heal over a period of 3–6 months in the absence of local neoplastic disease [1,2,3]. It is a dreaded complication of the use of radiation therapy in the treatment of head and neck cancer. Radiation induces tissue hypoxia in normal cells, resulting in an imbalance between cell death and collagen breakdown on one hand and the homeostatic mechanisms of cell replacement and collagen synthesis on the other hand. This results in a non-healing wound, in which the metabolic demands exceed the oxygen and vascular supply.
Clinical manifestations of ORN may include pain, orocutaneous fistula, exposed necrotic bone, pathologic fracture and suppuration [4,5,6]. ORN is more commonly seen in the mandible than in the maxilla due to relatively decreased vascularity and increased bone density of the mandible. In addition, the mandible often receives a greater dose of radiation than the maxilla.
Over the years, ORN has been treated by various methods. Hyperbaric oxygen therapy (HBOT) has been used as an adjunctive treatment for ORN with improved success rates. This treatment modality provides an increased oxygen tension at the tissue level to promote healing, especially in wounds with a compromised vasculature. The following report gives an account of a case of ORN of mandible managed with HBOT, thus strengthening the role of this treatment modality in management of post radiation injuries.
Case Summary
A 55 years old lady, a case of Ca throat was managed with Radiotherapy 05 years back. She underwent extraction of lower molars 03 months back. However, she was diagnosed with Osteoradonecrosis (ORN) of the mandible. The treating Maxillofacial Surgeon planned for surgical debridement under local anesthesia and referred her to Institute of Aerospace Medicine (IAM) Bangalore for Hyperbaric Oxygen Therapy (HBOT). General physical examination and systemic examination of the patient were within normal limits. Local examination revealed swelling and tenderness over the right mandibular region. On intraoral examination, a burrowing endophytic lesion was noted in the lower alveolus. The Orthopantogram showed multiple punctuate radiodense lesions over the right mandible adjacent to the ramus (Fig .1).
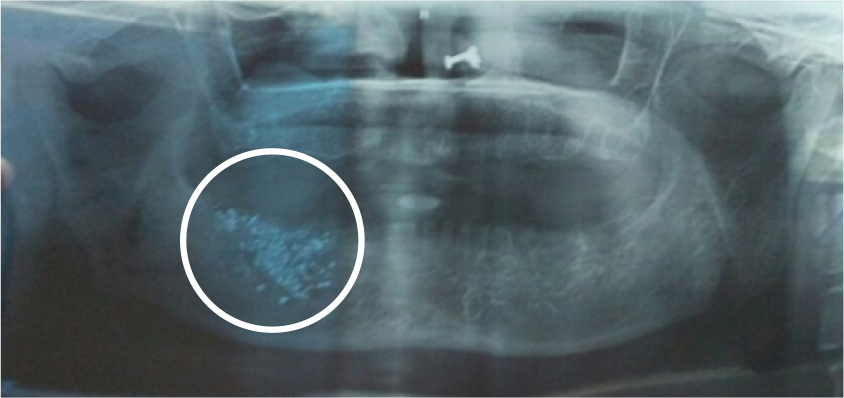
- OPG before administration of HBOT
Since the patient was likely to benefit from HBOT, she was taken up for the therapy and underwent all the mandatory investigations. The sessions were carried out in the Rapid Recompression Chamber (Fig. 2). The treatment profile consisted of 100% O at 2.5 Atmospheres Absolute (ATA) for 90 minutes with ascent and descent rate of 02 feet/minute (Fig. 3).

- Rapid recompression chamber
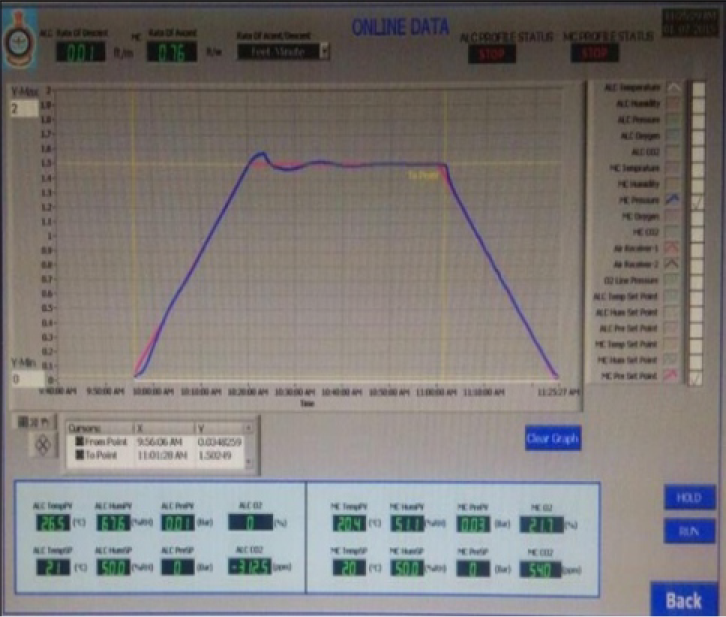
- Treatment profile
After 10 sessions of HBOT, there was a marked improvement in the form of reduced swelling and pain over the mandibular region. Consultation and follow-up with the Maxillofacial Surgeon was carried out and she was recommended to continue HBOT for 20 sessions.
Radiographic comparisons were made before administration of HBOT (Fig. 1) and after completion of 20 sessions of HBOT (Fig. 4). The Orthopantogram after completion of 20 sessions of HBOT revealed a marked increase in radiodensity as well as an increase in density of the trabecular pattern in the right posterior mandible, which was suggestive of healing bony lesion. After completion of the HBOT sessions, she was referred back to her treating Maxillofacial Surgeon where she underwent surgical debridement of the wound.

- OPG after 20 sessions of HBOT
Discussion
The pathophysiology of ORN was explained by the ‘3H’ principle by Marx in 1983 [7]. Radiation leads to formation of Hypocellular, Hypovascular and Hypoxic tissues. This tissue, including bone and soft tissue, loses its ability to repair and heal. In hypoxic, injured tissues, macrophages are not stimulated and fibroblasts fail to lay down new collagen, resulting in chronic non-healing wounds [4]. ORN is, therefore, a problem of impaired and inadequate tissue turnover and wound healing. A Fibroatrophic Theory was also proposed, which implies atrophy of the bone-forming cellular components as well as activation of the fibroblastic lineage which eventually replaces the tissue with abnormal myofibroblasts, resulting in ORN [8].
Clinically there are 3 types of ORN. Type I is trauma-induced ORN which occurs when radiation or surgical wounding are coupled closely together. The most common is Type II, also trauma-induced ORN, which occurs years after radiation therapy. Type III or spontaneous ORN can occur anytime after radiotherapy but commonly occurs 6 months to 2 years following radiotherapy, without any obvious preceding surgical or traumatic event [7,9].
The patient in this case report was detected with ORN following tooth extraction. Extraction before or after irradiation is said to be the most common initiating factor in the development of ORN in irradiated jaws [9,10]. The total incidence of ORN after tooth extraction in irradiated patients was found to be 7% [11].
Hyperbaric Oxygen (HBO) improves tissue healing by increasing the oxygen gradient in irradiated tissues. In normal non-irradiated wounds, there is a central area of tissue injury surrounded by tissue with normal perfusion, setting up a steep oxygen gradient across the wound. Such gradient act as the physical-chemotactic factor and attracts macrophages to the wound [12,13]. Lactate, iron, steep oxygen gradient, angiogenesis factor and macrophage-derived growth factor, these in turn promote capillary budding and collagen synthesis in wounds [12]. However, in wounds with radiation tissue injury (which results in diffuse damage), only shallow oxygen gradients are created. The stimulus for fibroplasia and angiogenesis is therefore lacking. Administration of Hyperbaric Oxygen restores the steep oxygen gradient needed for wound healing [12,13,14]. Several studies have reported on the positive tissue effects of HBOT [9,15,16,17,18]. Oxygen gradients stimulate the macrophage-derived growth factor. At IAM, 118 cases of post radiation injuries were treated with HBOT. Out of which 41 cases were of ORN. Improvement was noted in majority of the cases i.e. 37 cases whereas 4 were not followed up [19].
Conclusion
Head and neck cancers are common and radiation therapy is very effective in these cancers. The presence of teeth in the jaws, as well as the functional and cosmetic importance of the mandible implies that Osteoradionecrosis of the mandible has a major impact on the patient's quality of life. This case report supports the existing literature on potential benefits of HBO as an adjunctive treatment of mandibular ORN and adds another chapter in the success story at Institute of Aerospace Medicine, Bangalore.
References
- Osteoradionecrosis: clinical experience and a proposal for classification. YJOMS. 1987;45:104-110.
- [Google Scholar]
- Osteoradionecrosis of jaws: review and update. Hyperbaric Oxygen Rev. 1984;12(5):78-128.
- [Google Scholar]
- Osteoradionecrosis of the jaws: a retrospective study of the background factors and treatment in 104 cases. J Oral Maxillofac Surg. 1997;55(6):545-6.
- [Google Scholar]
- Hyperbaric oxygen therapy in the management of osteoradionecrosis of the mandible. Adv Otorhinolaryngology. 1998;54:14-32.
- [Google Scholar]
- A modified protocol to treat early osteoradionecrosis of the mandible. Undersea Hyperb Med. 1995;22(2):161-70.
- [Google Scholar]
- Hyperbaric oxygen and postradiation osteonecrosis of the mandible. Eur J Cancer B Oral Oncol. 1993;29B(3):201-7.
- [Google Scholar]
- Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg. 1983;41(5):283-8.
- [Google Scholar]
- The radiation-induced fibroatrophic process: Therapeutic perspective via the antioxidant pathway. Radiother Oncol. 2004;73:119-131.
- [Google Scholar]
- Studies in the radiobiology of osteoradionecrosis and their clinical significance. Oral Surg Oral Med Oral Pathol. 1987;64(4):379-90.
- [Google Scholar]
- Osteoradionecrosis of the jaws: clinical characteristics and relation to the field of irradiation. J Oral Maxillofac Surg. 2000;58:1088-1093. discussion 1093–1085
- [Google Scholar]
- Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: A systematic review. Int. J. Oral Maxillofac. Surg. 2011;40:229-243.
- [Google Scholar]
- Regulation of repair: Hypoxic control of macrophage mediated angiogenesis In: Hunt TK, Heppenstall RB, Pines E, eds. Soft and hard tissue repair. Praeger: New York; 1984. p. :41-9.
- [Google Scholar]
- Cellular microenvironment in healing and nonhealing wounds In: Hunt TK, Heppenstall RB, Pines E, eds. Soft and hard tissue repair. New York: Praeger; 1984. p. :50-66.
- [Google Scholar]
- Problem wounds in oral and maxillofacial surgery: The role of hyperbaric oxygen. In: Davis JC, Hunt TK, eds. Problem wounds — the role of oxygen. Elsevier: New York; 1988. p. :65-123.
- [Google Scholar]
- The effect of hyperbaric oxygen treatment on bone regeneration: an experimental study using the bone harvest chamber in the rabbit. Int J Oral Maxillofac Implants. 1988;3(1):43-8.
- [Google Scholar]
- Histologic study of the effect of hyperbaric oxygen therapy on autogenous free bone grafts. J Oral Maxillofac Surg. 1996;54(8):975-81.
- [Google Scholar]
- The effect of hyperbaric oxygen on irradiated oral tissues: transmucosal oxygen tension measurements. J Oral Maxillofac Surg. 1997;55(10):1103-7.
- [Google Scholar]
- Hyperbaric Oxygen Therapy and Mandibular Osteoradionecrosis: A Retrospective Study and Analysis of Treatment Outcomes. J Can Dent Assoc. 2001;67:384.
- [Google Scholar]
- Hyperbaric Oxygen Therapy–IAM experience a review of past forty years cases. Ind J Aerospace Med. 2013;57(2):38-44.
- [Google Scholar]





