Translate this page into:
Upgradation of aircrew with minor musculoskeletal injuries in the operational bases: Need for a relook

*Corresponding author: Gaurab Ghosh, Department of Space Medicine, IAM IAF, Bengaluru, Karnataka, India. debinibash@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dev R, Ghosh G, Binu Sekhar M, Biswal P, Tripathy NK, Joshi VV. Upgradation of aircrew with minor musculoskeletal injuries in the operational bases: Need for a relook. Indian J Aerosp Med 2023;67:17-21. doi: 10.25259/IJASM_8_2022
Abstract
Objectives:
Musculoskeletal injuries (MSKI) have been one of the most common contributors to disabilities among aircrew. The existing policy mandates all cases of MSKI in aircrew of the Indian Air Force, including minor injuries such as a sprain of small joints and phalangeal fractures to be evaluated at the Institute of Aerospace Medicine (IAM), majority of which do not warrant a complete Human Engineering (HE) assessment. Hence, a need was felt to decentralize evaluation and empower other boarding centers/operational bases with local aerospace medicine specialists to carry out the evaluation.
Material and Method:
A retrospective analysis was carried out of a total of 930 cases of MSKI among serving aircrew who reported to IAM between Jan 2016 and Oct 2020.
Results:
About 27.68% of cases were of lower limb injuries and 16.52% of cases were of upper limb injuries. About 36.77% of cases of upper limb and 52.71% of cases of lower limb injuries were treated surgically while 63.23% upper limb and 47.29% lower limb injuries were managed conservatively. Full functional recovery within 12 weeks was seen in a significant number of conservatively treated distal upper and lower limb injuries not involving joints.
Conclusion:
HE assessment of MSKI at IAM is comprehensive including exposure to simulated aeromedical stressors. However, certain minor musculoskeletal disabilities did not require full HE evaluation and simulator facilities of IAM. Sending aircrew with such minor disabilities from field units to IAM amounts to an administrative obligation that can be avoided by empowering other medical boarding centers and local operational bases which have aerospace medicine specialists. This paper discusses the procedure of conduct and facilitation of aeromedical evaluation of aircrew in the non-flying medical category with certain minor MSKI in the field.
Keywords
Aircrew
Musculoskeletal injury
Functional evaluation
Human engineering
INTRODUCTION
Musculoskeletal injuries (MSKI) remain one of the common sets of disabilities among military aircrew.[1] The common risk factors include motor vehicle accidents, inadvertent slips or falls, and sports-related injuries. Injuries can also occur during aircraft events such as hard or crash landings and ejection. While some of the injuries become an impacting factor in the aviator’s ability to carry out routine activities, most injuries recover completely without any residual functional restriction. Conventionally, evaluation of all aircrew of the Indian Air Force (IAF) having MSKI has been done at the Institute of Aerospace Medicine (IAM) to ensure comprehensive Human Engineering (HE) assessment. Apart from clinical and radiological examinations, HE assessment includes the evaluation of specific kinematics of the injured part of the body while performing various functional tasks and under exposure to simulated aviation stressors. The aircrew may additionally undergo a cockpit evaluation on the ground or during flight, if deemed appropriate, for further assessment of any interruption in controlling the flight because of the disability. Recertification of aircrew to a flying medical category, thus, is based on his performance in the abovementioned tests. Further upgradation of aircrew from a restricted flying category to an unrestricted flying category has been decentralized in the IAF as it does not again require the aircrew to undergo complete functional assessment.[2] They are being carried out in the medical facilities of the operational units based on recommendations of the Squadron Aerospace Physician.
It is felt that some minor MSKI, such as sprain, strain, or simple, and undisplaced limb fractures not involving the joints, may not always require the aircrew to undergo a complete HE assessment at IAM. Hence, the evaluation of such cases can be decentralized and carried out at other IAF boarding centers and operational bases in the field where an Aerospace Medicine Specialist is available. The same is already in practice in other organizations of the Armed Forces. This paper aimed to identify those MSKI which could qualify for evaluation without comprehensive HE assessment at IAM. The paper also attempted to place recommendations for the practice of evaluation of these cases at other medical facilities.
MATERIAL AND METHODS
The medical data of all aircrew with MSKI who reported for HE assessment at IAM during 4 years period from 2016 to 2019 were examined. The radiological findings, opinions of concerned specialists, and results of their HE assessment were scrutinized. Descriptive statistics were applied to analyze the data.
RESULTS
A total of 930 military aircrew cases with MSKI were evaluated at the HE department at IAM. Out of which, 689 (74.08%) of the cases required extended observations in the low medical category followed by repeat evaluations before the award of fitness for flying. The remaining 241 (25.91%) cases were upgraded after their first evaluation at IAM. Of the total cases, 481 (51.72%) underwent evaluation under simulated aviation stressors of vibration and acceleration; and 4 (0.43%) required cockpit evaluation coordinated by IAM and conducted at a nearby flying base. In other cases, those who were required to review with cockpit evaluation after a certain observation period were recommended to undertake the said evaluation at their home bases.
Among all the disabilities, 154 (16.55%) were injuries of the upper limb and 257 (27.63%) were lower limb injuries. Fifty-seven (37.01%) of the upper limb injuries and 135 (52.52%) of lower limb injuries were treated surgically whereas 97 (62.99%) of the upper limb cases and 122 (47.47%) of the lower limb cases underwent conservative management.
While analyzing the upper limb injury cases, it was observed that, out of the cases which were managed conservatively, 7 out of 11 (63.6%) of simple undisplaced fractures of the forearm involving shaft of a single bone, 15 out of 20 (75%) of metacarpal fractures, and 17 out of 21 (80.9%) of fractures involving phalanges were completely healed with proper alignment and the pilots achieved full functional recovery during the first review within 12 weeks itself.
Similarly, among the lower limb injuries managed conservatively, 4 out of 5 (80%) of the hairline/stress fractures of the tibia, 5 out of 7 (71.4%) of isolated fractures of fibula, 19 out of 27 (70.3%) of simple metatarsal fractures and 100% of phalangeal fractures of the foot achieved complete radiological and functional recovery within initial 12 weeks of observation.
DISCUSSION
Although the evaluation of MSKI at IAM has the advantage of having the resources of a variety of evaluation tools for complete functional assessment, it is evident from the above analysis that, assessment for many minor musculoskeletal disabilities of upper and lower limbs does not require the use of simulators for evaluation. Most such cases could be evaluated in their home bases by Flight Surgeons with a comprehensive clinical, radiological, and functional assessment. Referring such cases to IAM for HE evaluation would be an additional administrative and financial burden to the organization which could be avoided.
A decentralized system for evaluation and reflighting an aircrew with MSKI is already in vogue in other organizations of the Armed Forces. If a similar system is to be followed in the IAF, the comparative advantages/disadvantages of conducting the evaluation in the field by Aerospace Medicine Specialists over evaluating other IAF Boarding Centres are discussed below:
-
Evaluation at operational bases/field stations by squadron flight surgeons (Aerospace medicine specialists)
There would be no requirement of referring the aircrew to major evaluation or boarding centers.
Delays in reporting at IAM/other Boarding Centers due to administrative reasons such as getting movement approval, taking appointments from Boarding Centers, making necessary travel arrangements, etc.; or due to operational commitments can be avoided
The Senior Aerospace Physician in the sector/zone can be utilized for professional supervision and vetting of the aeromedical recommendations and disposal
Availability of aircraft and Qualified Flying Instructors would facilitate supervision and conduct of cockpit evaluation, if required, for disposal
The existing policies for medical evaluation already include the involvement of local Aerospace Medicine Specialists for the upgradation of aircrew at the field level from restricted flying category to unrestricted flying category. Further empowerment with adequate equipment and a stipulated procedure would strengthen this evaluation system at field level
The field medical centers would have to be provided with requisite equipment and tools for the necessary functional evaluation and for a refresher training of all Squadron Flight Surgeons posted on protocols and procedures followed at IAM for use of such equipment for functional evaluation.
-
Evaluation at boarding centers other than IAM
It will be easier to provide resources for evaluation centrally to other boarding centers in comparison to field stations
However, the aircrew needs to be referred to the boarding centers for HE evaluation. The purpose of evaluating the aircrew in his/her home base to save traveling time remains unaddressed in that case
The existing guidelines for approval of the medical categorization can be utilized. However, the capability of other boarding centers to deal with this additional workload needs to be worked out
Should the aircrew require cockpit trial, the Qualified Flying Instructors are not available at other boarding centers
The opportunity for supervision/scrutiny of a Senior Advisor (Aerospace Medicine) is not available at other boarding centers.
From the above, it is evident that other IAF boarding centers do not offer an additional advantage over IAM in conducting a functional evaluation of MSKI in aircrew. However, if the evaluation is carried out on the operational bases by field Aerospace Medicine Specialists under the supervision of a Senior Advisor, there is an advantage of testing the aircrew physically in an aircraft in the field. Moreover, boarding centers other than IAM do not have a Senior Aerospace Medicine Specialist available at all times. In view of this, an appropriate procedure for the evaluation of aircrew with MSKI at the operational bases is suggested below:
Major musculoskeletal disabilities, post-operative cases, post-ejection cases, cases requiring spinal evaluation, and cases requiring assessment under simulated aviation stressors can be referred to IAM as being traditionally done.
The decision to recommend HE assessment at IAM for other minor MSKI can be entrusted to local Aerospace Medicine Specialists in the field in consultation with zonal Senior Advisors
If the concerned clinical specialist (Orthopedic Surgeon) has recommended for upgradation to an unrestricted flying category, the field Aerospace Medicine Specialist needs to examine the aircrew and ensure normal soft tissue/bony healing, normal power in the involved muscles, full ranges of motion in the involved, and adjacent joints without any residual deformity. He has to ensure that the disability has achieved full clinical recovery and radiological consolidation. If required, he needs to conduct cockpit evaluation with a qualified instructor pilot on type aircraft.
The opinion of the local Aerospace Medicine Specialist results of functional and cockpit evaluation and the documents of medical board proceedings can be shared with the zonal Senior Advisor for scrutiny and concurrence. The board proceedings can be further sent for perusal by higher authorities.
In flying stations where there are no Aerospace Medicine Specialists available, the cases can be referred to a zonal Senior Advisor to decide whether the cases can be evaluated and upgraded by Senior Advisor himself, based on the recommendations of treating specialists; or sent to IAM for HE evaluation.
For carrying out the functional evaluation, the following equipment which is used at IAM is suggested to be used at the field level also:
IAM-Exercise maneuver protocol (EMP) platform (details given below)
Goniometer
Hand grip dynamometer
Lower limb dynamometer.
IAM-EMP
IAM recently developed and validated a protocol called IAMEMP which can be used on both male and female aircrew between 18 and 45 years of age for their functional assessment post-recovery from an MSKI. Incorporation of the tool with other components of HE assessment is effectively being used for improved functional assessment.[3]
The test protocol involves the use of the IAM-EMP Platform which is a custom-made wooden platform at par with the Functional Movement Screen (FMS®) Testing kit measuring 2 × 6 ft with a thickness of 2 inches (inclusive of 5 mm Styrofoam mat pasted atop). In addition, it has two hollow steel bars measuring 5 ft, used as an indicator stick and hurdle bar. Two steel bars measuring 90 cm with sliding clamps and scale are used to form the hurdle. A standard tape measure to record hand length is used. A 4 feet high wooden platform is used to perform the jump test. The platform enables the aircrew to be evaluated on various physical performance tests, in line with FMS® to assess his overall functional performance.[4,5]
A cutoff score of 18 out of 24 has been statistically deemed to be the limit below which the aircrew is considered functionally restricted.[3] Hence, it is recommended that any aircrew with a score of <18 during evaluation at field level should be referred to IAM for further HE assessment. A workshop is also recommended to be conducted for the training of Aerospace Medicine Specialists at the operational bases on this newly developed protocol. The platform and the exercises involved in the scoring of performance are given in [Figure 1] below.

- Institute of aerospace medicine-exercise maneuver protocol testing.
The guidelines for carrying out a functional assessment of MSKI at the field level are represented below in the form of a flowchart [Figure 2].
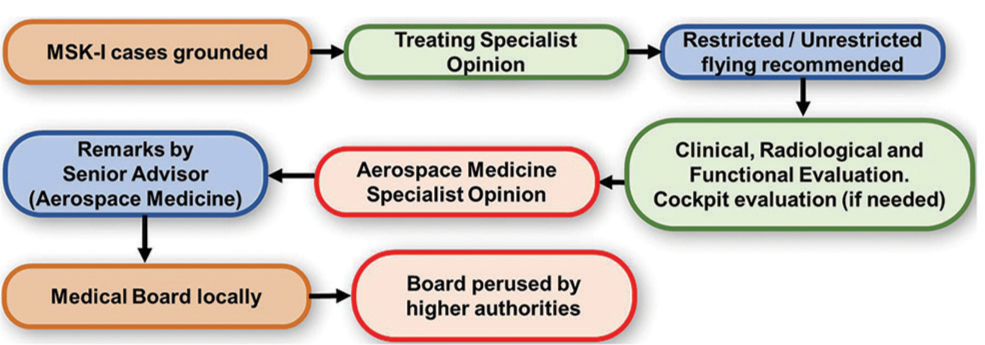
- Flowchart showing proposed procedure of evaluation of musculoskeletal injuries at operational bases.
CONCLUSION
This study highlights that the recovery of minor MSKI among aircrew was smooth and there were no chronic complications that would concern the aviator. Perspectival intimation of the aircrew to come to IAM, from wherever they are in the country for review of these minor injuries, is not only cumbersome but also is a financial expenditure on the organization. Therefore, recommendations have been made that cases of such injuries could be evaluated locally by Aerospace Medicine Specialists of the flying stations and upgraded under the concurrence of the zonal Senior Advisor. For the purpose of uniformity in assessment, a protocol has been laid regarding the procedure of evaluation of these injury cases. This decentralized protocol will evidently reduce the aircrew number needing to come to IAM for HE assessment and strengthen the evaluation process by the empowered Aerospace Medicine Specialists in the operational bases.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- A Retrospective analysis of musculoskeletal disabilities in military and civil aircrew. Ind J Aerosp Med. 2008;52:8-13.
- [Google Scholar]
- Upgradation of Musculoskeletal Injuries in the Operational Bases: Need for a Re-look. In: Paper Presented at 60th Annual Conference of Indian Society of Aerospace Medicine. 2021.
- [Google Scholar]
- Establishment and validation of institute of aerospace medicine-exercise maneuver protocol (IAM-EMP) Ind J Aerosp Med. 2021;65:10-6.
- [CrossRef] [Google Scholar]
- Pre-participation screening: The use of fundamental movements as an assessment of function-Part 1. N Am J Sports Phys Ther. 2006;1:62-72.
- [Google Scholar]
- Pre-participation screening: The use of fundamental movements as an assessment of function-Part 2. N Am J Sports Phys Ther. 2006;1:132-9.
- [Google Scholar]






