Translate this page into:
United Nations mission in Sierra Leone (UNAMSIL): medical deployment and experiences
Abstract
Indian troops participated in the United Nations Mission in Sierra Leone (UNAMSIL), as part of peacekeeping force from Dec 1999 to Feb 2001. The IAF contributed a full-fledged, self-contained contingent consisting of 212 personnel (including 33 aircrew) and 8 helpicopters (4 Chetak, 4 Mi-8 and 3 Mi-35 gunships). An Aviation Medicine specialist accompanied this contingent and gained useful experiences in the medical administration, aircrew care, CASEVAC and policies being followed in such missions. This paper shares some of these issues from the first-hand experience and insight gained during the induction and deployment The contribution and operational deployment of troop from various countries is discussed along with the medical deployment and the levels of medical care as followed in UNAMSIL. The health experiences of the Indian Aviation unit, with specific reference to staffing, health cover provided, medical management, Preventive Medicine etc, are elaborated. The IAF Medicare facility was tasked with additional responsibilities in respect of CASEVAC within the entire mission area. The IAF unit evacuated more than 150 patients and the IAF MI Room personnel gained a rich experience of providing in-flight care for 43 patients (including 15 battle casualties). The paper also discusses the Aeromedical aspects experienced in Peacekeeping operations.
Keywords
UNAMSIL
Aero medical issues
CASEVAC
The United Nations Mission in Sierra Leone (UNAMSIL) was established in Sep 1999 by the UN Security Council sanction with an aim to carry out peacekeeping operations in civil war ravaged Sierra Leene. Troop strength of 6500 personnel was sanctioned initially which was subsequently increased to 10000 in Jan 2000 and then.to 13500 in Aug 2000. Indian troop contribution to the mission commenced in Oct 1999. IAF was approached to provide a contingent of 4 Chetak and 4 Mi-8 helicopters along with supporting personnel. The initial IAF contingent, UNAMSIL, consisting of 148 personnel (including 24 aircrew), was induced in the mission area in Mar 2000 with the author as the Aviation Medicine Specialist accompanying the contingent. Subsequently in Jun 2000, additional 64 personnel with 3 Mi-35 helicopter gun ships were inducted.
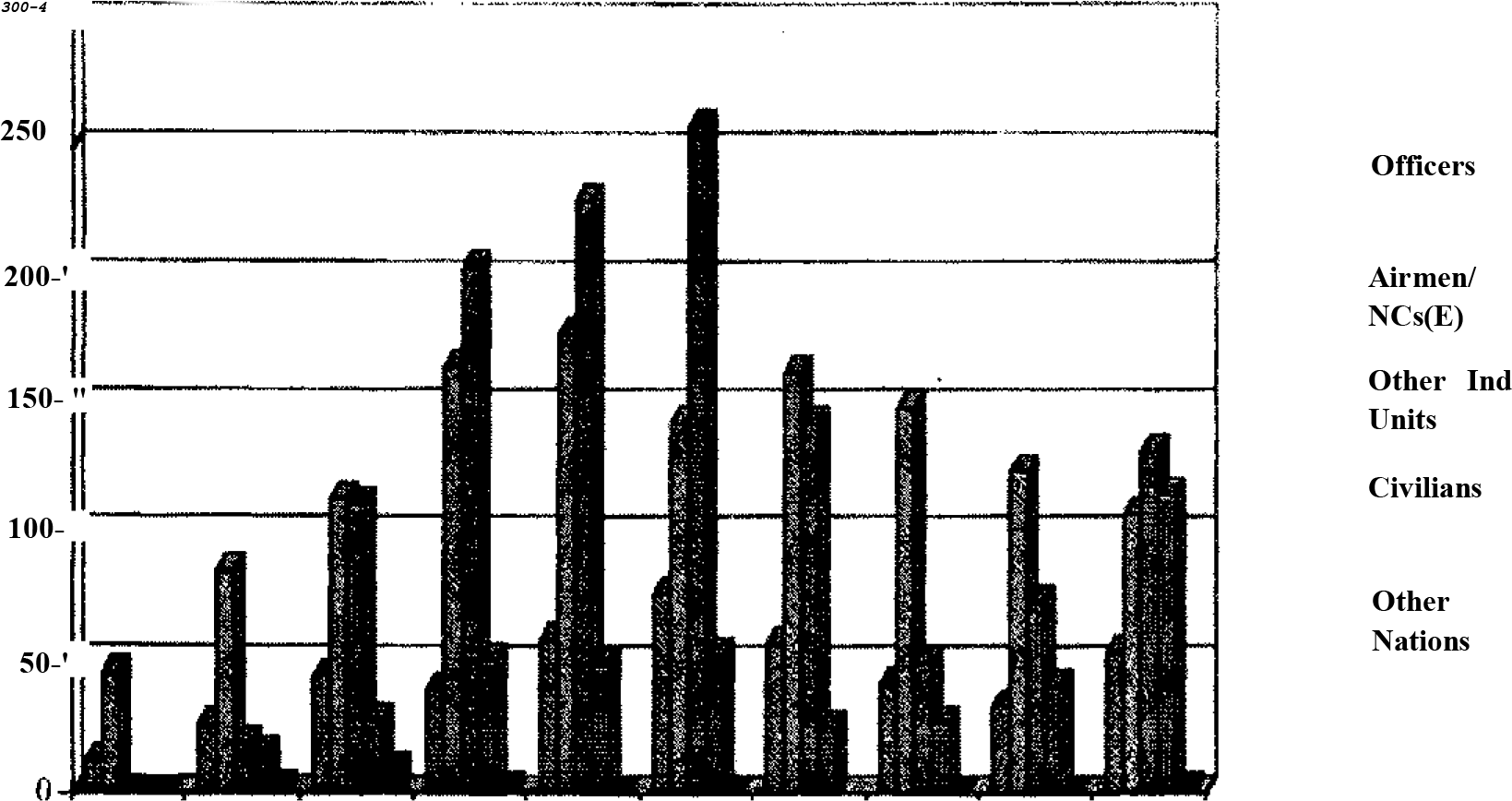
Troop Contribution and Deployment of UNAMSIL Forces [1]
The troop contribution of various member nations of the UN is shown in Table 1. As far as the geographical deployment of UN Peacekeepers in Sierra Leone, Indian troops, which were located at Freetown, KENEMA, Dam, Hastings, Port Loko and Bo-Guince.
| Country | Formation | Troop Strength (Appx) | MOs |
|---|---|---|---|
| Nigeria | 1 Sector HQ + 3 Inf Battalions | 3200 | Each Battalion 2 |
| Jordan | 1 Sector HQ + 2 Inf Battalions + Level II Hosp | 1800 | Each Battalion 4 Section Hospital 6 |
| Ghana | 1 Inf Battalion | 500 | Each Battalion 2 |
| Guinea | 1 Inf Battalion | 500 | Each Battalion 2 |
| Bangladesh | 1 Sector HQ + 2 Inf Battalions (Inducted in Nov-Dec 00) | 2000 | Each Battalion 2 |
| Kenya | 1 Sector HQ + 2 Inf Battalions (Inducted in Nov-Dec 00) | 2000 | ? |
| Russian | Aviation Unit (Inducted in Dec 00) | 150 | 1 |
| Ukraine | Tpt Coy (Inducted in Dec 00) | 450 | 2 |
| India | Ind Batt, Eng Coy, Field Hosp, Fid WkShp, Ind Aviation Unit | 3660 | 20 |
Medical Organisation [2]
The deployment pattern of medical resources was similar to the standard military practices followed in the AMC. The various Medicare levels were designed and based on the troop strength to which the cover was provided, with flexibility provided to the troop contributing nations in respect of manning. According to the level of Medicare, the facilities to be provided were specified. The medical standards and practices followed by various countries were different and the Force HQ had done some degree of standardization in treatment and evacuation protocols. Language barrier also posed its own problems in providing medical care (troops from Guinea, Jordan, Ukraine and Russia were non-English speaking)
Levels of Medicare. The various Levels of Medical Care, which form the medical infrastructure in any UN Peacekeeping operations, is summarized at Table 2. The IAF contingent MI room was planned as a limited second line facility. It was a static facility and was roughly equivalent to the independent, isolated MI rooms in the AMC or small SMCs in the IAF. All the infantry battalions in the mission area including both the Indbatts were also having limited second line facilities.
| Type | Description | Aim | Examples |
|---|---|---|---|
| Basic | Individual level first aid service and personal medical and hygiene supplies | • To provide basic medical kit carried by each soldier on person. | Individual Battalions |
| First Line | • Medical cover to company and company minus | • To provide specially trained medical personnel for resuscitation, stabilization and triage of seriously injured personnel. | All company |
| (Level 1) | deployments of the troops | deployments | |
| Limited | • The limited second line | • To provide advanced specialist combat medic & medical cover to | • Battalion HQ |
| Second | facility. | stabilize seriously injured personnel for transport to second or third | • IAF Contingent |
| Line | • The battalion level care provided with the help of medical officers and the medical assistants. | line medical facility. • To conduct emergency medical / surgical procedures (e.g. suturing, splinting and casting) • To perform basic diagnostic tests (e.g. cultures, infectious disease identification) • To have capability to evaluate, observe or isolate patients for 48 hours. • To maintain a sterlisation capability. • To maintain a limited pharmaceutical capability (e.g. intravenous fluids, analgesics and serums) • To perform definitive treatment against a wide variety of naturally occurring disease. |
|
| Second | • Sector level cover | • To provide holding and stabilization facility for seriously ill / injured patients for initial specialist management | • Banbatt at Lungi |
| Line | • Referred to as 'level | • lorbatt at Kenema | |
| (Level ID | II hospitals' • Correspond to peacetime section hospitals |
• To provide peripheral Surgical and anaesthetic care, physician support, nursing care and dental cover. • To augment the medical cover to the local battalion / other formations as and when required. • To hold casualties till evacuation is feasible. |
|
| Level III | • Referred to as 'level 3 hospital' • Corresponds to 99-bedded hospitals in AMC with capabilities to augment the beds. The highest level of medical care available within the mission area. |
• To provide specialist cover in Surgery, Medicine, Anesthesialogy, Ophthalmology, Otolaryngology, Radiology, Psychiatry, Dermatology, Laboratory and Preventive Medicine. • To provide specialist nursing care. • To provide medical cover to Force HQ staff including the civilian staff. • To augment peripheral medical staff as and when required. • To provide blood and blood products for the entire mission area. • To provide specialist dental cover. |
Indian Field Hospital at Freetown |
The Indian Field Hospital. This was a level 3 facility with 11 medical officers (including 1 specialist each in Surgery, Medicine, Anesthesiology, Ophthalmology, Preventive Medicine and Radiology), 5 nursing officers and 1 dental officer with the supporting staff. The hospital was located about 40 Km from IAF MI Room in Freetown. The hospital also provided Dental cover, specialised lab services and Blood.
Force HQ. The Force HQ medical administrative staff included a Force Medical Officer (FMO - Lt Col) reporting to the Force Commander for operational matters and to the Chief Administrative Officer for Adm matters. He was responsible for the health policies in the mission area A Force Medical Supply Officer, a Mecfical Officer conducting the Force HQs clinic and nursing and clerical staff supported him.
Peripheral Staffing. The recommended number of Medical Officers is one doctor per about 450-500 troops [2]. However, the contingents are allowed to bring in as many doctors as they consider necessary depending on their country's policies. Two Indian battalions and the Indian Aviation Unit had one doctor each, which was lesser than the other countries. (Nigeria, Bangladesh, Ghana, Guince: Two each, Jordan: Four with one Dental Officer) The number of medical assistance and trained battlefield nursing assistants to be carried with each contingent are not specified and individual contingents could choose the number considered appropriate by them. Provision of medical cover at each of the battalion deployments was however mandatory and was to be arranged by the contingents themselves, i.e. the contingent could not depend on level II or level III hospitals for primary medical cover. The Nigerian battalions had lady Nursing officers on their strength.
MI Room Activities : Indian Aviation Unit [3,4]
Staffing. One Specialist in Aviation Medicine and three medical assistants (Warrant Officer - Gen Duties, Cpl - Physiotherapist, Cpl - Health Assistant) were part of the initial 148 personnel contingent. In addition, the helicopter gunship contingent inducted in Jun 2000 carried one general duty medical assistant. Perhaps, the ideal composition of the medical assistants would have been one health assistant, OT ORA, Lab technician and Physiotherapist each.
Preinduction Medical Activities. The medical planning and activities commenced before the arrival of the selected members of the contingent to New Delhi. Following activities were undertaken in the period prior to the induction:
Medical Examination. The Contingent doctor, in accordance with the form specified by the UN, carried out a detailed medical evaluation of inductees at AF Station New Delhi. This medical examination was more elaborate than the annual medical examination in the IAF. The investigations required included all routine examinations, complete biochemistry, X Ray Chest (PA), ECG (R), VDRL, HIV and certain other investigations like Erythrocyte counts. The completed form and the investigation reports were forwarded to the Department of Peace Keeping Operations (DPKO), UN HQ, New York (These forms are referenced by the UN in settlement of various medical compensation claims if they arise in the mission area).
Immunization. Immunization against Yellow fever was mandatory and was carried out at Armed Forces Clinic, New Delhi. Immunization for Typhoid and Tetanus was updated at the time of preinduction medical examination. Immunization against Cholera was optional and was not carried out in case of the Indian contingents, as there were no specific inputs of Cholera epidemic from the mission area.
Anti Malaria Measures. Sierra Leone was reported endemic zone for Chloroquine resistant Falciparum Malaria by the UN. Deltramethrin impregnation of mosquito nets was done prior to issue in India itself and recommended Chemical Prophylaxis with Tab Mefloquin. (Started 1 week prior to induction in to the mission area, @ one per week).
Medical Stores and Equipment. The Contingent was required to be self-sufficient in medical stores and equipment for one year. (Estimated period of deployment before replacement) There was no existing MMF to work on. Liaison was done with the Medical Officer of the Indian Army contingent to procure their MMF figures that were based on the AMC experience in different missions. Drug requirements for IAF contingent was calculated and demands placed with SMC, Air Force Station New Delhi (AFND). The drugs and non-expendable stores available readily in the Medical stores were provided from AFND and those not available were local purchased.
Contingent Education. The health education of the troops prior to induction in the mission area was an important responsibility. The UN did not organize any health education. Health inputs from various sources such as WHO bulletins, Internet, Indian Army recee reports etc. indicated the presence of communicable diseases (MT Malaria, Lassa fever, HIV) and infestation of typical snakes (spitting cobra) and peculiar insects (Tumbu Fly, Acid Fly) Moreover, health education was necessary for Psychological preparation of the contingent to tackle the fear of the unknown and to make them combat ready. A totals of 26 lectures were conducted and covered those on disease prevention and demonstrations on basic first aid.
Immediate Activities in the Mission Area. A functional MI Room was set up at the temporary camp in a tent within 48 hours of arrival in Sierra Leone on 16 Mar 2000. Health and sanitation measures such as water purification, setting up of hygienic kitchen, sewage disposal pits etc. for the camp was primary activities apart from routine and emergency sick call. The first CASEVAC was done and in-flight medical cover provided on 07 April. The MI Room was shifted to the permanent location at Hastings in its permanent location in mid April. The photographs of the MI Room are shown at Fig. 1-3.
- MI Room, IAF Contingent UNAMSIL - External View
- MI Room, IAF Contingent UNAMSIL - Treatment Room Enclosure
- MI Room, IAF Contingent UNAMSIL - Medical Store Enclosure
Cover Provided. The medical staff, in addition to 212 members of the aviation contingent, provided limited Level II medical cover to about average 750 troops at Hastings, the deployment location. These included the Indian Army's Transport Coy, Quick Reaction Coy and Engineering Coy. In addition, the inmates of the UN transit camp, civilian staff and Military Observers at Hastings, Hastings airfield staff and locally employed civilians were also given medical care.
Data (17 Mar 2000 to 31 Jan 2001)
Sick Report. The sickness data for the period Apr 2000 to Jan 2001 showed an average daily sick report of 13.0 (total sick report -3743) The month-wise sick report is shown at Fig 4. The system-wise distribution of the disease in shown in Fig. 5.
Excused Duties / Sick in Quarters. A total of 153 man-days were lost due to EDs and SIQs from Mar 2000 to 31 Jan 2001 during the whole period of deployment (0.25%).
Hospital Admissions. 37 IAF personnel were admitted to the Indian Field Hospital for a total period of 290 days (Loss of man-days -0.47%).
- Monthly Sickness Rate

- System-wise Sickness Distribution Pie (in %)
Preventable Diseases
Various preventable diseases encountered by the IAF contingent are shown at Table 3. All the six MT Malaria cases occurred because Mefloquin Prophylaxis was either absent (3 cases immediately on induction from the Mi-35 contingent inducted in Jan 2000) or temporarily discontinued by the patient for personal reasons. Lassa fever was not endemic to Western Sierra Leone where the contingent was deployed and consequently the contingent did not have any case. We did however evaluate a suspected case of Lassa fever, an Army officer, who later died in the Indian Field Hospital.
During the initial settling phase, Scorpion bites and Tumbu Fly infestations were common. Snakes were commonly found but the contingent personnel followed strict anti-rodent and anti-snake measures, thereby causing no snakebites. Tumbu fly lays egg on drying clothes. The eggs pierce the skin when clothes are worm and develop into larvae, in subcutaneous space, in 8-9 days and clinically present as a furuncle like eruption. The treatment is by applying a coat of Vaseline over the furuncle to starve the larvae of Oxygen when it crawls out of the skin through its breathing pore. [5] The contingent in the initial settling days had 5 cases of Tumbu Fly infestation, which was subsequently prevented. One of the co-located Army soldier had massive infestation and 11 larvae were extruded from his body over 2 days at the IAF MI room.
Acid Fly was a type of fly that on skin contact caused severe local allergic reaction akin to Hymenoptera stings. [5] Painful blisters followed the initial allergic response over the area of contact and took 2-3 weeks to heel. Immediate washing with Sodium Bicarbonate solution was found to reduce allergic response and was advised to all personnel.
| Disease | No. of Cases |
|---|---|
| Chloroquine resistant Falciparum Malaria | 06 |
| Enteric (Typhoid) fever | 02 |
| Tumbu Fly infestation | 05 |
| Acid Fly Dermatitis | 03 |
| Scorpion bite | 13 |
| HIV / AIDS | Nil |
| Lassa fever | Nil |
| Snake bite | Nil |
Other Activities. Some of the other activities carried out by the MI Room were as follows:
-
Physical Fitness Program. The contingent personnel were motivated to pursue a graduated exercise program with following aims in mind:
Obesity control in the light of high caloric UN ration diet (@ 5800 cal/person/day)
As a Psychological alternative to prevent loneliness in the absence of families.
As a projection of Indian Armed forces' emphasis on discipline and physical fitness in the International arena.
Humanitarian Aid. A 3-day free health camp, inaugurated by the Vice President of Sierra Leone, was organized at the contingent's location in Hastings in Jan 2001 and was attended by about 7800 patients. The clinical specialists from the Indian Field Hospital aided in the conduct of the camp.
Family Planning Activities. After cessation of flying just prior to de-induction, Vasectomies were organized at the Indian Field Hospital and three of contingent aircrew benefited from this.
Aero Medical .Issues. The various Aero Medical issues of importance, concerning the operational preparedness of the aircrew are as follows:
Aircrew Fitness. The monthly data on the aircrew fitness rates is shown in Fig. 6. An average fitness rate of 96.6% was achieved between Apr 2000 to Jan 2001 (Range -94.8% in Sep to 98.9% in Nov) Preflight medical examination was meticulously conducted as part of morning briefing. Annual medical examination of the aircrew was not carried out in the light of the detailed examination carried out prior to induction.
-
MefloquinProphylaxisandFlying. Mefloquin has known side effects such as nausea, vomiting, diarrhea, abdominal pain, dizziness or vertigo, loss of balance, and Neuro- Psychiatric events such as headache, somnolence, and sleep disorders (insomnia, abnormal dreams). These are usually mild and may decrease despite continued use. [6] The IAF aircrews also were required to take the tablet on a weekly basis, thereby bringing in the issue of flying fitness with the drug. In our experience, nausea and dyspepsia were the most common side effect observed. In the initial 2-3 weeks, some of the aircrew did report headache and sleep disturbances on the day of Mefloquin intake but the symptoms subsided on their own in later weeks. The following steps were taken to minimize the side effects:
The aircrew were observed for side effects on ground for a period of at least 3 weeks (1 week prior induction and 2 weeks after induction when the aircraft were being assembled and readied).
Tuesday and Wednesday were fixed as days of Mefloquin parade with roughly half the aircrew taking Mefloquin on either of the days.
' Liquor and Non-vegetarian food were avoided on Tuesday to avoid Gastritis with Mefloquin.
A tablet of Multivitamin or Iron was given as an incentive for the Mefloquin parade.
The pilots returned to the cockpit duties only after 24 hours of Mefloquin intake.
In case of unexpected increase in flying task, correct pairing of the aircrew was ensured so that at least one of the two pilots was drug-free for at least 24 hours.
-
Spatial Disorientation (SD). There were no incidents or accidents on account of SD due to onboard GPS systems, high efficiency of aircrew and repeated indoctrination on the subject. Spatial and Geographical disorientation was however a distinct Aero Medical problem because of the following reasons:
Unknown terrain and unprepared helipads.
Tropical weather (frequent thunderstorms and treetop level clouds).
Unsatisfactory ATC and RT support because of multilingual operators (Russians, Ukrainians and local African pronunciations)
Psycho-Social Issues. Stresses of isolation from families, combat flying and alien environment were as evident in the aircrew as in other contingent members. Close liaison was required to detect the early signs. Crew paring was done carefully to preserve the ideal cockpit gradient. Physical fitness regimes and unit entertainment gatherings were organized. Emotional stability was preserved at all costs. Motivating factors such as satellite telephone facility, TV, movies carried from India also played their role.
-
CASEVAC / MEDEVAC
UN Policy. All the CASEVAC/ MEDEVAC within the mission area were done by Helicopters due to poor roads and rebel threat. Early and comfortable air evacuation of the casualty upholds the high value accorded to the human life by the UN. All the casualties, as a rule were, evacuated to level 3 hospital in Freetown. There was no system of staged evacuation. Further evacuation to specialised centers outside the mission area (level 4 and 5 Medicare), if required, was done by fixed-wing aircraft, (commercial airlines or UN aircraft if available). The casualties recommended for repatriation to the home country were transported by commercial airline flights at UN expense.
One of the primary roles of the Indian Aviation unit was CASEVAC and the unit evacuated over 150 casualties from the field between Apr to Nov 2000. In the mission area, the IAF MI room was tasked with providing in-flight medical cover, on as and when required basis. This reduced the time taken to reach the casualty (helicopter could directly head » to site of casualty) and avoided the return trip for the medical attendants of dispatching units, thereby saving significant UN resources. A total of 30 CASEVAC stories (43 patients) were provided in-flight cover, which also included 15 battle casualties picked up directly from the battlefield. The monthly distribution of CASEVAC done is shown in figure 7. Two special CASEVAC kits were devised, one for medical assistant and one for Medical Officer, for this purpose.
-
Lessons Learnt
Vibration and noise in both Mi-8 and Chetak do not permit even recording of pulse let alone Blood Pressure. Hence these are not ideal platforms for any in-flight care.
Any manipulation (IV / Splints etc) needs to be done on ground prior to take off, as the same is extremely difficult in air.
Mi-8 has strong FOL smell in the cockpit and this can cause nausea and respiratory discomfort to certain patients. To minimize the discomfort, Oxygen inhalation was started for sensitive patients on ground and continued onboard.
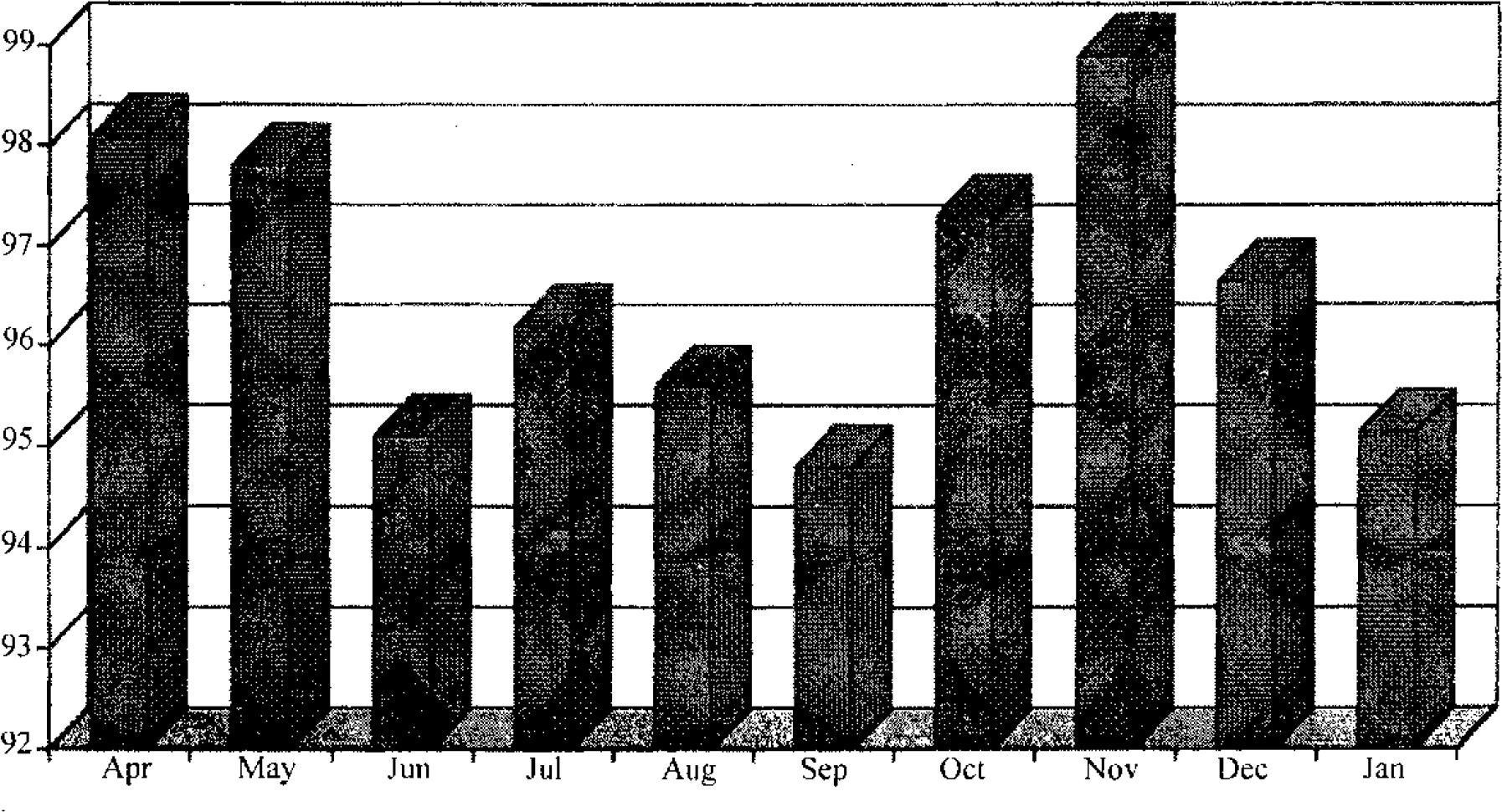
- Monthly Aircrew Medical Fitness %
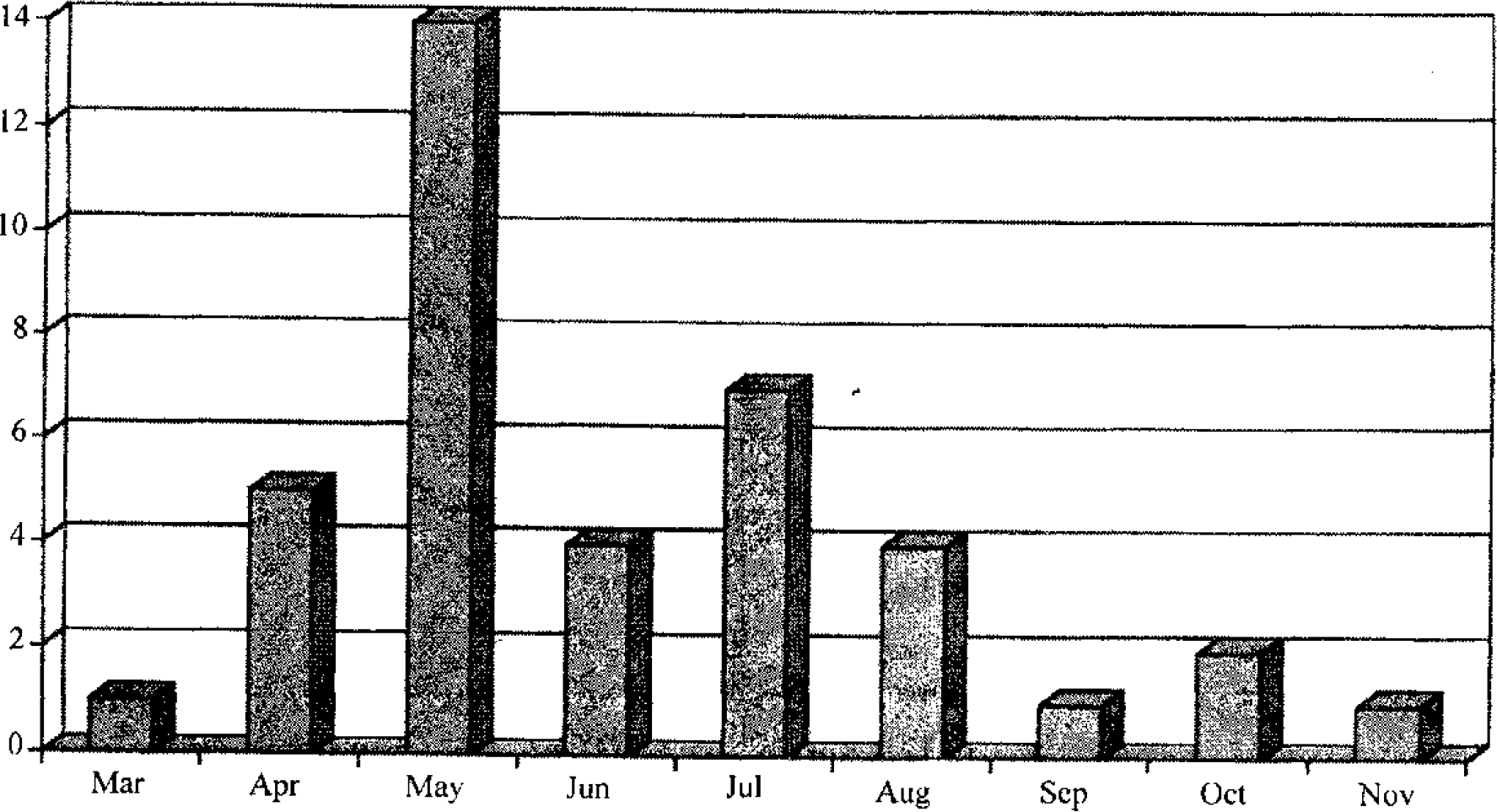
- Monthly Task In-Flight Cover for CASEVAC
Post Deinduction Medical Issues
The UN does not specify any post-de-induction medical formalities but in accordance with the IAF rules, the contingent personnel were medically examined on AFMSF-3 on de-induction.
HIV testing was repeated immediately on de-induction and advice was given for a follow up test after 6 months. All the medical storey (nonconsumable and drugs left over) were returned to SMC, AF Station New Delhi.
-
A low. borderline Haemoglobin count was detected in almost all the personnel on de-induction, which showed rapid recovery on administration of oral Iron. Following reasons are postulated for this observation:
Nutritional. Long-term consumption of frozen foods.
Infective. Effect of Sub Clinical MT Malaria infection that did not manifest clinically due to the Mefloquin chemical prophylaxis.
Conclusions
The role of Senior Medical Officer, IAF contingent, UNAMSIL was a unique experience of International peacekeeping operations due to the diversity of troops treated and relative unfamiliarity with the prevalent health hazards. The medical deployment doctrines followed in the UN peacekeeping operations were found to be similar to those followed in AMC with subtle differences in manning and CASEVAC policies. The IAF MI Room provided holistic disease curative and preventive services to all the troops in Hastings. The disease prevention activities yielded satisfactory results for the IAF contingent, as shown by the low overall sickness rate, insignificant loss of man-hours on account of sickness / hospitalization, high aircrew fitness rates and low incidence of preventable diseases. CASEVAC experience enriched significantly. Aircrew health was well preserved despite the operational combat duties in alien environment.
References
- Internet Reference http//www/UN.Org Accessed on 30 Dec 2000
- Department of Peace-Keeping Operations - Field Administration and Logistics Division New York: UN HQ; 1996. p. 3-A-4, 3-B-7, 9-A-29-C-1, 9-D-2, 9-E-6
- [Google Scholar]
- Interim Report on MI Room - Indian Aviation Unit UNAMSIL. Report submitted to Air HQ (Med Directorate).
- [Google Scholar]
- Concluding Report on MI Room - Indian Aviation Unit UNAMSIL. Report submitted to Air HQ (Med Directorate).
- [Google Scholar]
- Ectoparasite Infestation and Arthropod Bites and Stings In: Harrison's Principles of Internal Medicine [book on CD-ROM] (14th ed). New York: McGraw Hill; 1998.
- [Google Scholar]
- LARCAMW Safety fnformati'oa. Sited at web page (http://f.www.lariam.com/about_lariam.asp#safety_info Accessed on 02 May 2003
- [Google Scholar]






