Translate this page into:
Surgical Correction of Mandibular Prognathism in an Aviator
Abstract
Mandibular prognathism is a term coined in case of the mandible over-riding the maxilla with a cross bite of the dental occlusion element also termed as Skeletal Class III relation and Dental Class III Malocclusion. A 24 year old serving apparently healthy Air force MIG 21 fighter pilot in A1G1 medical fitness reported to AFIDS while on planned annual leave with chief complaints of difficulty in chewing and abnormally protruding lower jaw leading to unsightly aesthetics, difficulty in mastication, altered speech and low morale. Aeromedical issues revolved around altered concave facial profile with accentuated negative nasionmenton angle compromising face mask fit as also speech alteration for effective communication. Asper norms for ideal dental fitness for armed forces, he was unfit since none of his anterior teeth came to approximation and posterior teeth were in complete cross bite. After obtaining written consent, he was operated under general anaesthesia for bilateral intra oral sagittal split osteotomy and posterior setback with rigid internal fixation. Post operative profile improved drastically, phonation improved especially the linguo- palatal sounds and the total mandibular Class III cross bite was corrected to normalcy with Class I harmonious occlusal scheme both dental and skeletal. The subject was placed out of flying category for three months for satisfactory healing of surgical bony wound subsequent to which he was evaluated and since bone healing was adequate, masticatory and phonetic functions had improved he was reverted back to his flying category.
Keywords
Mandibular prognathism
Bilateral sagittal split osteotomy
Introduction
The human face is a complex architecture of soft tissue muscular envelope over the underlying intricate bony foundation. The facial harmony for function and aesthetics is determined by the positive alignment of the jaw bones in three dimensions - transverse, antero-posterior and supero-inferior. as well as the approximation of the masticatory dental unit in occlusion.[1] A severe mismatch of the maxilla and mandible in the antero posterior dimension leads to malocclusion and compromises aesthetics, function and phonation.[2] Mandibular prognathism is a term coined in case of the mandible over-riding the maxilla with a cross bite of the dental occlusion element also termed as Skeletal Class III relation and Dental Class III Malocclusion. Facial anomalies may negatively affect body image and self-concept & confidence. This paper deals with the peculiarities and challenges in the management of a case of mandibular prognathism in an air crew and the outcome for fitness for retention in flying category.
Case Report
A 25 year old serving apparently healthy Air force MIG 21 fighter pilot with more than 500 hours of flying in the type aircraft, in A1G1 medical fitness reported to AFIDS while on planned annual leave with chief complaints of difficulty in chewing and abnormally protruding lower jaw leading to unsightly aesthetics, altered speech, difficulty in mastication and low morale. History revealed the subject to be otherwise physically fit with no genetic, hormonal or developmental anomalies and a pass-out of National Defence Academy and noticed the complaints four years ago insidiously and had gradually reached the present state. Clinical examination revealed a concave facial profile, an increased lower third facial height, abnormally extruding mental protuberance and an extensively flared out mandibular gonial angle. Intra orally there was total cross bite of the mandibular teeth over riding the maxillary dentition by one molar width with cheek bite of the maxillary third molars. Standard cephalometric analysis of digital lateral cephalogram was carried out and the measurements pointed towards almost a centimetre horizontal discrepancy and a working diagnosis of mandibular prognathism was arrived at.
Aero-medical concerns revolved around the concave facial profile with an accentuated negative nasion menton angle which could have potentially affected effective adequate fit of the face mask. However the subject did not experience any major hindrance due to the condition. Another issue was related to the prognathic override of the mandible, altering the tongue posture during speech leading to variation in effective communication especially the linguopalatal consonants sounding like linguo dental sounds. Due to the slow and insidious growth of the mandible the subject had adapted to a compromise in speech. The overall morale and confidence of the subject due to the functional and aesthetic compromise attributable to the deformity was in jeopardy as also altering his social interaction (like acceptance among peers, opposite sex) forcing him to report for options for correction.
As per norms for ideal dental fitness he was unfit since none of his anterior teeth came to approximation and posterior teeth were in complete cross bite. Since the condition was more of a skeletal deformity and due to the long protracted repeated review appointments involved, fixed orthodontic therapeutic correction was beyond the purview. Study models and mock surgical templates were created using cephalometric tracings and a bilateral intra oral sagital split setback procedure was planned. Patient was counselled of his condition and was explained of the surgical option for correction of his skeletal anomaly along with risk, complications, benefits and the need for placement in temporary non flying category, subsequent to concurrence of which he was evaluated for pre anaesthetic fitness and accepted in ASA grade I. After obtaining written consent, he was operated under general anaesthesia for bilateral intra oral sagittal split osteotomy and posterior setback with rigid internal fixation.
Surgical Procedure
The subject was laid supine and general anaesthesia was administered through nasal tube with intermittent positive pressure ventilation. Buccal sulcus retromolar trigone incision was given bilaterally to expose the posterior and ascending ramus medially towards the lingual and mandibular sulcus where the inferior alveolar neurovascular bundle was identified and separated medially and a horizontal cut was given with the rotary saw just to enter into the cortex. The bony cut was continued forward to cross over to the lateral mandible along the external oblique ridge to reach the first molar region. Here a vertical bony cut was continued till the lower border where the cut completed the lingual cortex with gentle taps and malleting with a sharp osteotome. The vertical ascending ramus was thus separated from the horizontal body. All the four third molars were removed and after carrying out a similar bony separation on the contra lateral side, the mandible was mobilised by gentle pressure and taps with a sharp osteotome. Maxillo mandibular fixation was undertaken using arch bars and tie wires in the planned posterior setback occlusal scheme with maximum occlusal masticatory approximation. Four hole titanium miniplate with 9 mm screws were used for rigid internal fixation bilaterally. Tie wires were released to check condylar position, passive occlusion and skeletal correction. Wound was sutured after hemostasis and patient was nursed in in patient care and administered antibiotics and anti inflammatory intra venous drugs. After one week sutures were removed and the subject was placed on semi solid diet for four weeks and sent on sick leave. On uneventful satisfactory recovery after sick leave post op ceph logram and orthopantomograph were obtained and cephlometric analysis was done. He was placed in temporary non flying category for three months for convalescence and complete recovery. Post operative profile improved drastically, phonation improved especially the linguo- palatal sounds and lire total mandibular Class ITI cross bite was corrected to normalcy with Class I harmonious occlusal scheme both dental & skeletal. (Fig 1-4. Table 1).
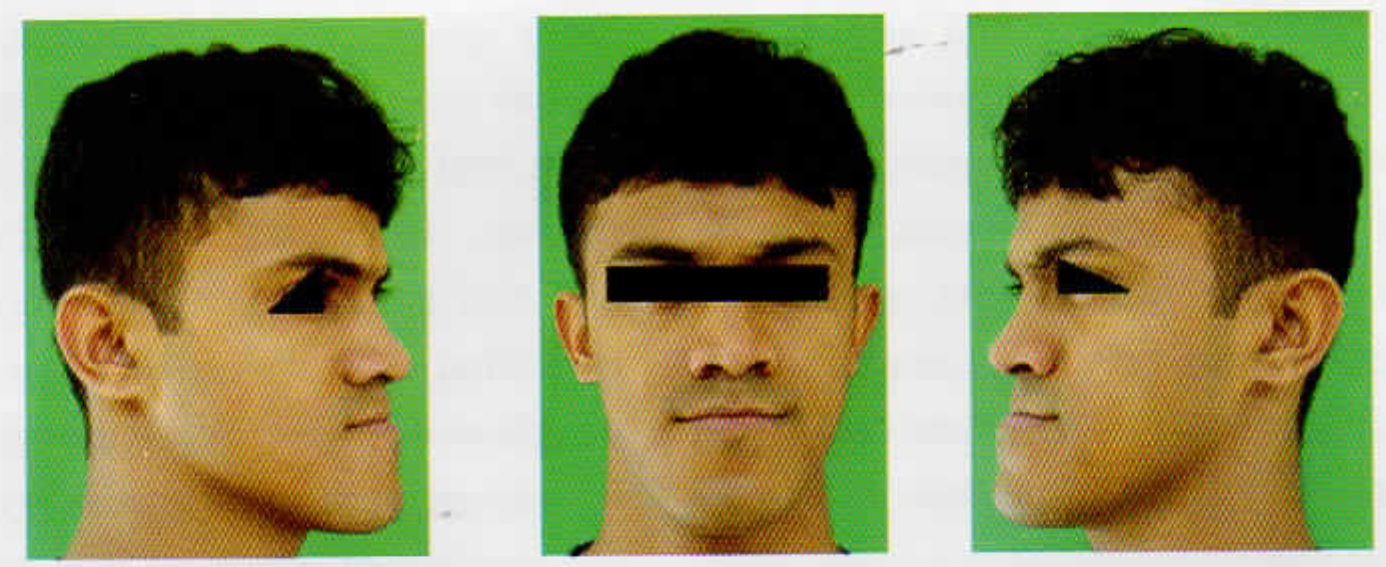
- Pre-Operative Photographs
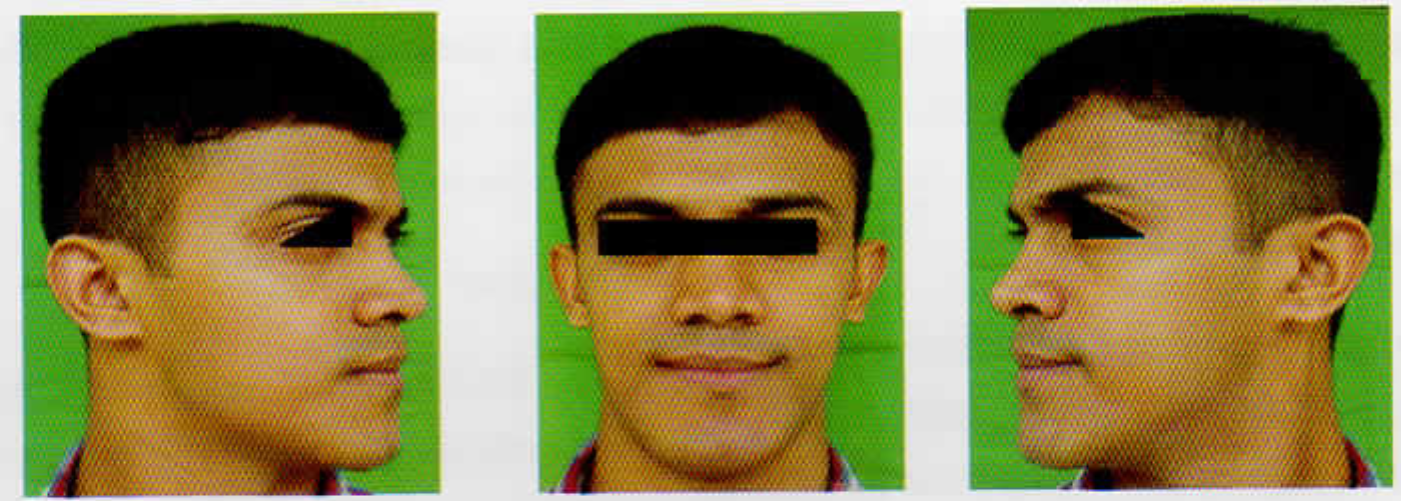
- Post-Operative Photographs
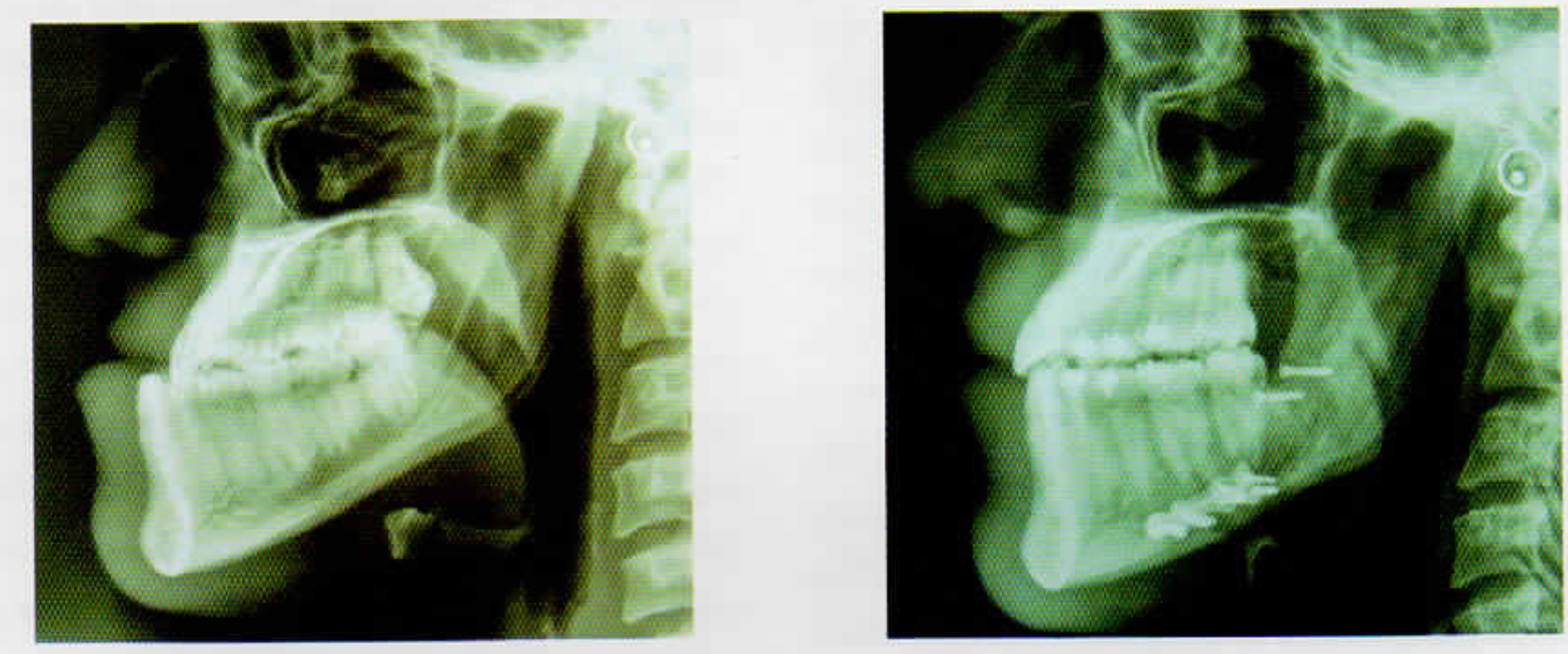
- Pre & Post-Operative Cephalogram
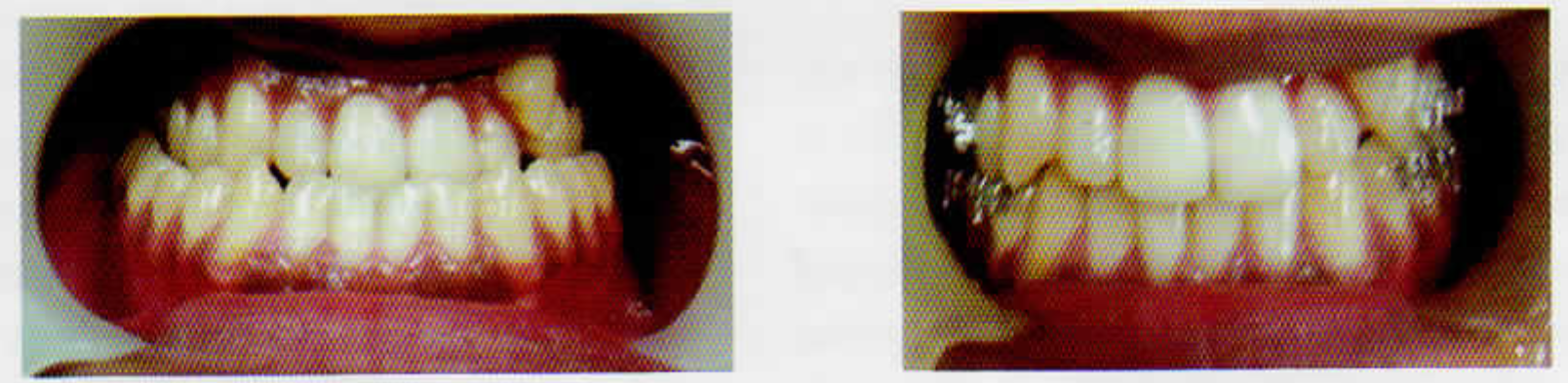
- Pre & Post-Operative Intra Oral Occlusion
| Parameter | Normal | Pre Op | Post Op |
|---|---|---|---|
| NA° | 82+/- 28686 | 86 | 86 |
| SNB° | 80+/- 29688 | 96 | 88 |
| ANB° | 2 | -10 | -2 |
| 1-NA° | 22 | 30 | 30 |
| mm | 4mm | 11mm | 11mm |
| 1-NB° | 25 deg | 10 deg | 10 deg |
| mm | 4mm | 2mm | 2mm |
| 1-1° | 131 | 155 | 136 |
| Occ- SN° | 14 | 5 | 12 |
| NSAr° | 123 +/- 6 | 114 | 114 |
| S Ar Go° | 143+/-6 | 140 | 140 |
| Ar Go Me° | 128+/-7 | 134 | 130 |
Discussion
The human face can tell a lot about personal attributes, the sex, race, age. physical fitness, as well as changes in emotion and his or her self-concept and confidence. Dentofacial defects are extremely prominent and unlike other physical handicaps, cannot be easily disguised. Facial anomalies may negatively affect body image and self-concept & confidence. Correction of dentofacial deformities often requires surgical intervention in order to achieve optimal functional, aesthetic and psychosocial results. A clinician’s effectiveness in providing the human side of treatment depends on understanding a variety of personal factors, such as personal history, family and cultural background, values, bias, attitudes, emotional responses and most importantly occupation. The clinical protocol involves prediction of both the surgical movements and soft tissue profile. [3] Prediction should be accurate in order to assess treatment feasibility, optimize case management and increase patient understanding and acceptance of the recommended treatment.
Mandibular prognathism is assumed to be a polygenic trait in the vast majority of cases. In a few families, this phenotype and perhaps a syndrome with a broader spectrum of facial anomalies seems to be determined by a single dominant gene of very low frequency. The phenotype is known to have occurred independently in several ethnic families across the subcontinent. The subject of this report was a solitary case with no familial or syndromic traits and was apparently healthy with growth and development within the horizon of physiologic range of variables. During his initial entry into National Defence Academy perhaps the growth was not yet fully established and was within the parameters laid for fitness. However with passage of time the unrestrained growth of the mandibular condyle without the horizontal stop of anterior incisal lock paved way for a prognathic mandible and the masticatory effort though compromised was compensated with deviated occlusal patterns for maximum intercuspation.
The following dental standard is followed for fitness in flying branch:- Candidate must have 14 dental points and the following teeth must be present in tire upper jaw in good functional opposition with the corresponding teeth in the lower jaw, and these must be sound or repairable:-
Any four of the six anteriors, and
Any six of the ten posteriors
They should be balancing on both sides. Unilateral mastication is not allowed.
Any removable or wired prosthesis are not permitted.
The recognition of this entity at entry level especially if the complete mandibular growth is not yet established becomes difficult more so when the subject is in his/her early twenties but a regular dental check up can only ascertain the presence of the condition. Literature recommends correction of the condition by orthognathic and orthodontic procedures due to the high predilection for severe Temporomandibular dysfunction, trauma from occlusion and malocclusion. Since when the subject was inducted to flying at around 20 years of age, the deformity was not compromising efficient function and occupation. He had not reported till as late as twenty five years of age when aesthetics and phonetics as well as mastication was affected due to the progressive nature of the mandibular growth which became protracted and established. Bilateral sagittal split osteotomy (BSSO) and vertical ramus osteotomy (VRO) are common techniques used for the correction of mandibular prognathism. [4,5,6] Both techniques have benefits and drawbacks, as well as pros and cons. Gonial angle is the anatomic angle formed between the ascending vertical ramus and the horizontal body. The gonial angle plays an important role in ensuring a harmonious facial profile and is evidently jeopardised in mandibular prognathism. Changes in this angle is an aesthetic concern for both the patient and the surgeon and the long term stability after surgical intervention with drastic profile change is best achieved by bilateral sagital split osteotomy.[7] Negative emotions due to violate facial appearance resulting from dentofacial disharmony may affect psychological status and general life adjustment of the patient. This is the origin of clinicians’ great responsibility for satisfying result of surgical treatment in patients with mandibular prognathism. As per the facial soft tissue and hard tissue cephalometric analyses, surgical correction was the best option and aimed at set back of the mandibular body by separating the body from the ramus. [8] In this regards, the final outcome in achieving the pre operative preparation prediction mock surgery has been fairly successful with the subject recuperating without much post operative complications and quick return to duty fit in Hying category.
References
- Modem Practice in Orthognathic and Reconstructive Surgery Vol 3. Philadelphia, Pa: WB Saunders; 1992. p. :2110-70.
- [Google Scholar]
- Prahl-Anderson B. Relationships between the orientation and movement of the human jaw muscles and normal craniofacial morphology. Eur.l Orthod. 1997;19:313-8.
- [Google Scholar]
- Trends in surgical treatment of Class III skeletal relationships. International Journal of Adult Orthodontics and Orthognathic Surgery. 1995;10:108-118.
- [Google Scholar]
- Stability and effect on the soft tissue profile of mandibular setback with sagittal split osteotomy and rigid internal fixation. International Journal of Adult Orthodontics and Orthognathic Surgery. 1995;10:15-25.
- [Google Scholar]
- Stability of hard and soft tissue profile after mandibular advancement in sagittal spl it osteotomies: a longitudinal and long-term follow-up study. European Journal of Orthodontics. 2008;30:16-23.
- [Google Scholar]
- Long-term stability of mandibular setback surgery: a follow-up of 80 bilateral sagittal split osteotomy patients. International Journal of Adult Orthodontics and Orthognathic Surgery. 2000;15:83-95.
- [Google Scholar]
- Stability after surgical-orthodontic correction of skeletal Class III malocclusion. I. Mandibular setback. International Journal of Adult Orthodontics and Orthognathic Surgery. 1991;6:7-18.
- [Google Scholar]
- Cephalometric evaluation of surgical-orthodontic treatment of skeletal Class III malocclusion. International Journal of Adult Orthodontics and Orthognathic Surgery. 1995;10:173-180.
- [Google Scholar]






