Translate this page into:
Study of Occupational Risks to Personnel in an Air Force Station
Abstract
The Air Force personnel by virtue of their diverse role in varying climatic conditions, terrain and often congenial psycho social environment are exposed to peculiar occupational stressors at workplace. Promoting occupational health measures is therefore of prime importance for optimizing the efficiency, and contentment of these personnel. Accordingly a study was planned to assess occupational risks to personnel in an Air Force Station. The study was conducted sequentially in the three phases at Air force Station with one of the most advanced air bases in the country. Tarmac trades and work stations had higher occupational morbidity profile than the nontarmac work stations contributing to more than 80% of the morbidity. Locomotor injury contributed to more than 50% of the morbidity. Next in order are occupational dermatoses and Noise Induced hearing Loss (NIHL). Locomotor injury, NIHL, and occupational dermatoses mainly contribute to occupational morbidity among the airfield maintenance staff. Work practices at some of the work-stations were incorrect from the safety point and could result in accidental injuries.
Keywords
Occupational stressor
Locomotor injury
Noise Induced Hearing Loss
Introduction
The Armed forces by virtue of its diverse role in varying climatic conditions, terrain and often congenial psycho social environment are exposed to peculiar occupational stressors at workplace. It is well recognized that a variety of physical and chemical hazards exist in the aviation environment [1,2,3]. Studies have been published regarding emerging morbidity both in Russian and American armed forces due to occupational exposure [4,5]. Information about occupational health disorders in the Armed forces has been sporadic in India [6,7,8]. Occupational stressors likely to affect the services are heat, noise, non ionizing radiation, accidental injuries due to machinery and industrial toxins [6,7,8]. Occupational health is of prime importance for optimizing the efficiency, well-being and contentment of the workers. Thus there is an urgent necessity to objectively identify the risk profile and put suitable safety measures in place.
Aims and Objectives
Study the morbidity patterns of different occupational groups/trades working with aircrafts and other related equipment, based on their medical records.
Evaluate the occupational risks in various work environments of personnel in Air Force station.
Study the operational procedures in these occupational settings with the view to analyze hazardous and critical control points.
Make suitable recommendations regarding workers safety and health.
Material and Methods:
Place of study: Air force Station with one of the most advanced air bases in the country.
Study population: All air warriors posted in Air Force station including the lodger units and Base Repair Depot located in /around the airfield.
Sampling frame and Size: For first phase of the study, a review of 100% of the medical records of all personnel below officer rank was done. For the second phase a sample size of 300 was selected using multi- stage cluster sampling according to work stations.
Exclusion criteria
Officers were excluded as their nature of duties are more variable.
Any personnel working at the work station for a period less than 06 months were excluded from the study.
Phases of study: The study was conducted sequentially in the three phases.
Phase I - Cross sectional record based study of occupational morbidity from Medical records (AFMSF-1) held with SMO, Air Force Station. These records were analysed to correlate with any patterns emerging with their trades/occupational setting.
Phase II- In phase II, the data was collected by a pre-tested, structured, self-administered questionnaire. The participants were asked to recall ‘any occupational morbidity’ while working in the present work station for a period exceeding 06 months.
Phase III- In this phase environmental survey of the clusters included in second phase was conducted. The survey was done for certain known physical hazards like heat, noise and UV radiation and highlight their association with morbidity patterns emerging in the first two phases.
Sampling Procedure (Phase II): The second phase of the study was two stage cluster sampling. The work stations were divided as the runway, aircraft dispersal and contiguous areas, area within 100 meters of these were defined as tarmac (T), Work stations located more than 100 meters but within 500 meters were defined as near- tarmac (NT). While those located more than 500 meters away were categorized as non-tarmac (nt). 20 work stations (called clusters) were identified and 10 work stations were selected using probability proportional to size as part of the study. 30 persons were selected from each cluster randomly based on their unique service number. Ten work stations (clusters) included in the study were as per Table No 2
Measurement of Noise Levels
Noise levels in decibels were measured at work stations by using a hand held battery operated Type 2 sound level meter (SLM). The maximum and average noise levels were measured at each work station for a period of two hours in a work shift.
Measurement of Heat Levels
The heat levels at work stations were measured by calculating the Wet Bulb Globe Temp in deg C. The Wet bulb and Dry bulb reading were taken using Sling Psychrometer and the radiant heat was measured using a Globe Thermometer. Time-weighted average (TWA) WBGT was used to assess average heat exposure over the work shift of eight hours
Measurement of Ultra violet radiation Levels
Ultra violet radiation levels were measured at work stations by using a hand held battery operated Ultra Violet Light meter, measuring the peak irradiance levels in mWatt/cm2. The UV Meter was calibrated for the spectral bandwidth of 290-390nm, which is essentially a UVA range of irradiance. The maximum level and average for a two hour period of a shift was monitored.
Work practices and use of personal protective measures
These were objectively observed and analysed during phase III of the study. The methodology adopted was ‘Walk around inspection of health hazards’ as standardized in Technical Manual of Occupational Safety and Health Administration (OSHA)[9].
Limitations of the study
The questionnaire based survey carries an element of subjectivity.
The cross sectional study indirectly shows an association of a work place /occupation with morbidity.
The risk of occupational hazards incrementally rises with duration of exposure.
Non Combatants were not included in the studies, who too are subjected to occupational hazards.
Results
First Phase
In this phase the medical records were surveyed for any occupational morbidity in the past three years, the numbers of records surveyed were 2648: occupational morbidity was recorded in 54 (2.04%). Locomotor injury was recorded as the predominant occupational morbidity contributing for more than 50%. Occupational dermatitis and Noise Induced Hearing Loss (NIHL) were the other major occupational morbidity (Fig 1)

- Record Based Occupational Morbidity
Trade wise breakdown: The trades which are working on aircrafts were classified as tarmac trades (T), Those working in Air traffic control, maintenance labs etc were defined as near-tarmac trades (NT). While others were taken as non tarmac trades (nt).
As we can make out from Table 1, the medical records show an overwhelming majority (81.5%), of recorded occupational morbity among tradesmen working on tarmac (T) and near tarmac region (NT).
| Trades of personnel having occupational morbidity | Frequency (%) |
|---|---|
| TARMAC TRADES | 27 (50.0%) |
| NEAR TARMAC TRADES | 17 (31.5%) |
| NON TARMAC TRADES | 10 (18.5%) |
| TOTAL | 54 (100%) |
Second Phase:
As shown in Fig 2, the highest morbidity was reported from 25 respondents in the work stations on the tarmac (T), followed by 12 on near tarmac (NT). Which collectively forms 37 (88.1%) of the morbidity. 42 (14.0%) out of the 300 respondents reported occupational morbidity in the survey as shown in Fig 3. One third of the morbidity was due to occupational dermatitis (33.3%). While locomotor and ocular injuries collectively contributed for another one third (35.7%). Further analysis of the data reveals that almost all the categories of occupational morbidity were reported higher in the tarmac (T) work stations compared to others (Fig 4).
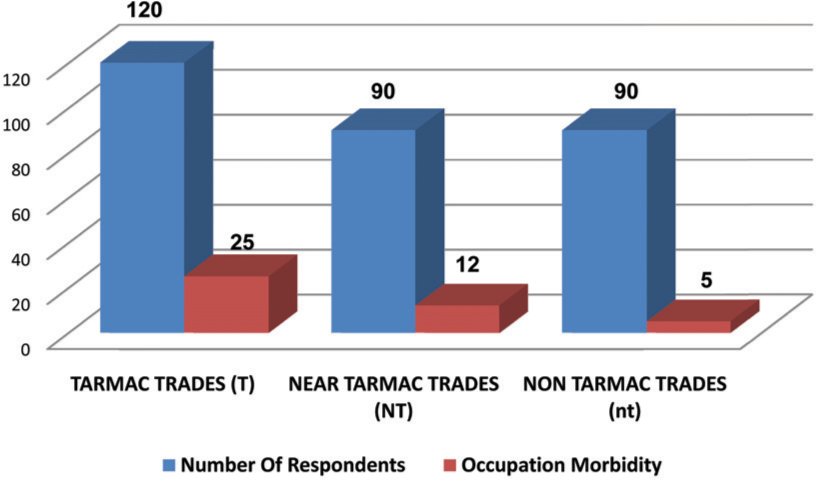
- Distribution of occupational morbidity in survey based on work stations
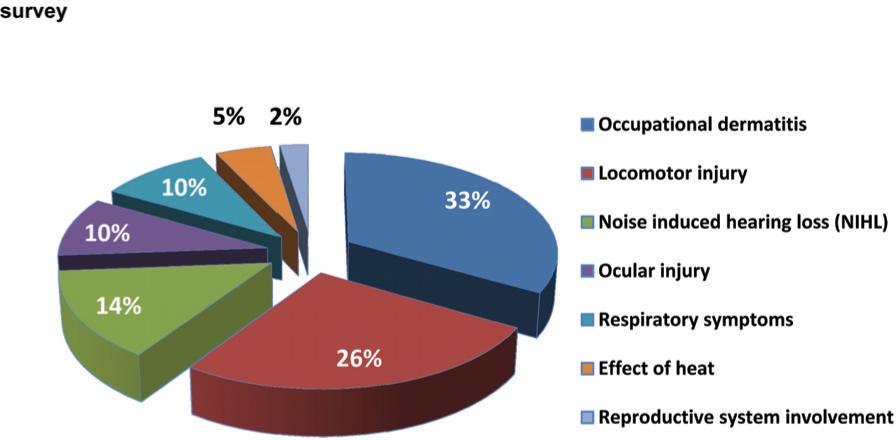
- Percentage distribution of occupational morbidity based on questionnaire survey
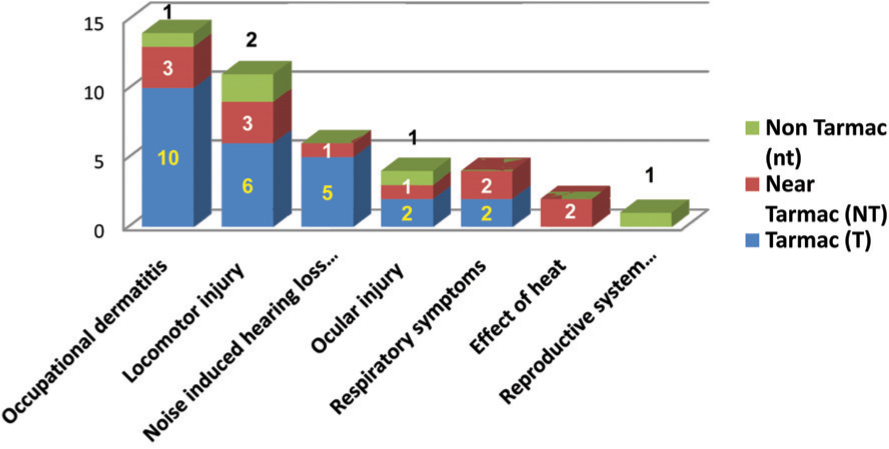
- Distribution of occupational morbidity at work station cluster
Third Phase:
Environmental Monitoring: Noise
The maximum noise levels were observed on the tarmac (T) and near tarmac (NT) work stations (97 – 107 dB). And the average noise level in a two hour period of a work shift was highest on tarmac (T) work stations, 88–92 dB (Table 2).
| S No | Work Stations | Maximum Noise (dB) | Average for 2- hours in shift (dB) |
|---|---|---|---|
| 1 | ATC/ Crash bay - (T) | 104 | 92 |
| 2 | DSS (SQN X) - (T) | 106 | 90 |
| 3 | DSS (SQN Y) - (T) | 105 | 92 |
| 4 | DSS (SQN Z) - (T) | 107 | 88 |
| 5 | Tech Flt (CR & SS) (NT) | 96 | 84 |
| 6 | Bomb Dump (NT) | 100 | 80 |
| 7 | Sea Eagle Complex (NT) | 98 | 75 |
| 8 | Radio Labs (nt) | 88 | 76 |
| 9 | Radar Labs (nt) | 89 | 78 |
| 10 | MT Section (nt) | 85 | 77 |
Environmental Monitoring: Heat
The maximum recording of both Wet Bulb Globe Temp (35.8 deg C) and average for an eight hour shift (30.2 deg C) was seen at bomb dump. It is notable that three work stations of near and non tarmac category had an average Wet Bulb Globe Temp for an eight hour shift exceeding 28 deg C, which is ideally suited for development of heat effects in workers in Occupational settings (Table 3).
| Sl | Work Stations WBGT (deg C) | Maximum in shift WBGT (deg C) | Average for 8- hours |
|---|---|---|---|
| 1. | ATC/ Crash bay - (T) | 32.2 | 26.6 |
| 2. | DSS (SQN X) - (T) | 31.6 | 26.2 |
| 3. | DSS (SQN Y) - (T) | 32.8 | 25.4 |
| 4. | DSS (SQN Z) - (T) | 31.8 | 27.8 |
| 5. | Tech Flt (CR & SS) (NT) | 34.6 | 29.8 |
| 6. | Bomb Dump (NT) | 35.8 | 30.2 |
| 7. | Sea Eagle Complex (NT) | 29.2 | 25.6 |
| 8. | Radio Labs (nt) | 26.4 | 23.4 |
| 9. | Radar Labs (nt) | 25.8 | 24.2 |
| 10. | MT Section (nt) | 32.0 | 28.2 |
Environmental Monitoring: Ultraviolet radiation
The maximum UV radiation was noted in radio and radar labs (6.4 – 7.8 mW/cm2). While the average UV radiation levels at most of the locations were below 0.1mW/cm2 (Table 4).
| Sl | Work Stations | Maximum radiation (mW/cm2) | Average for 2- hours period of shift radiation (mW/cm2) |
|---|---|---|---|
| 1 | ATC/ Crash bay - (T) | 1.2 | 0.04 |
| 2 | DSS (SQN X) - (T) | 1.6 | 0.02 |
| 3 | DSS (SQN Y) - (T) | 1.1 | 0.04 |
| 4 | DSS (SQN Z) - (T) | 1.8 | 0.08 |
| 5 | Tech Flt (CR & SS) (NT) | 4.6 | 0.08 |
| 6 | Bomb Dump (NT) | 3.8 | 0.02 |
| 7 | Sea Eagle Complex (NT) | 2.2 | 0.06 |
| 8 | Radio Labs (nt) | 6.4 | 0.10 |
| 9 | Radar Labs (nt) | 7.8 | 0.11 |
| 10 | MT Section (nt) | 2.0 | 0.02 |
Walkaround : Informal Interveiws
Use of personal protective measures like ear defenders and work overalls was not adequate at certain work stations. Though majority of the respondents (64.3%) from the tarmac (T) and near-tarmac (NT) work stations said that they regularly use ear defenders for protection, the work-practices survey revealed the incorrect practice of sharing overalls. The importance of wearing clean overalls was known to only 17.6% workers. Emergency drills for accidental injuries were not known by a substantial number of workers. While majority (62.4%) of the workers had received some training in first aid in case of an accidental injury, more than a third (37.6%) had less than adequate knowledge on basic actions in emergencies.
Discussion:
Occupational Morbidity:
The record based survey showed a recent history of occupational morbidity among all personnel to be more than 2% (Table 1). It is very likely that this was only the proverbial ‘tip of iceberg’ as highlighted in the Phase II of survey wherein the self-reported occupational morbidity was as high as 14% (Fig 2). Worldwide occupational morbidity among armed forces personnel has been receiving more attention [10]. Injuries remain the predominant cause of occupational morbidity in most studies [11].
In Phase I locomotor injuries were reported to be the predominant cause accounting for more than 50% (Fig 1). The Phase II of the study revealed that locomotor injuries was reported by respondents as the second most common cause of occupational morbidity accounting for 26.2% (Fig 3). A study in US army in Haiti found ‘work related injuries’ contributed to 36% of the ‘light- duty’ work restriction in an operational setting [12]. Most of the occupational dermatitis involves close contact with ATF lubricants and solvents used in maintenance of aircrafts. The excess risk in some of these work stations is well recognized internationally. Stringent standards have been laid down by the United States Air force for certain work stations considered more prone to occupational morbidity [13].
Noise Hazard
It is evident (Table 2) that the maximum noise levels were observed on the tarmac (T) and near tarmac (NT) work stations. It correlates well with the morbidity of NIHL detected in Phase II of the study, where 83.3% cases were reported from the tarmac (T) work stations. The annoyance effects of aircraft noise are widely recognized, however aircraft noise is also responsible for a significant amount of hearing loss as well as a contributor to a number of diseases [14,15,16,17]. Aircraft noise is a significant concern for approximately 100 sqKms surrounding most major airports [14]. Noise mapping of area around an aircraft has been studied in India, and the findings reveal the necessity to stringently monitor the work environment and the use of personal protective measures [18].
Heat Stress
Heat stress for the aircrew is a well recognized and researched entity [19]. The ill effects of heat are directly proportional to the duration of exposure. Both OSHA and NIOSH lays down stringent guidelines on the work rest ratio-per- hour on the WBGT levels in the occupational settings [20]. Heat stress has been a subject of a lot of studies in India and all over the world [21,22, 23, 24, 25]. Armed forces the world over are carrying out studies to quantify the risk to their personnel [26].
Non Ionising Radiation
Our study shows two cases (10%) of ocular injury and one case (2%) of reproductive system involvement, which were attributed to the possible exposure of radiation (Fig 3).
Communication equipments in Armed forces use radiowaves which may be Very High Frequency(VHF) or High Frequency(HF). Microwaves have higher frequencies than radio waves and are used in radars and satellite communications [29]. Radiowaves and microwaves are non-ionizing, thus have insufficient energy to ionize atoms in the body tissues but can cause thermal injury to tissues, most well recorded being the lens of the eye resulting in cataract [27, 28, 29].
Conclusion
Occupational morbidity contributes significantly to the overall morbidity rate of the trained maintenance staff at the airfield. tarmac (T) and near tarmac (NT) work stations have a higher occupational morbidity profile than the non tarmac (nt) work stations. Locomotor injury, NIHL, and occupational dermatoses mainly contribute to the occupational morbidity. All occupational morbidity may not get recorded in the medical records of the worker, denying him of the possibility of being compensated at the time of retirement for an occupational exposure attributable to service. Use of personal protective measures like ear defenders and work overalls was not adequate at certain work stations. Emergency drills for accidental injuries was not known by a substantial number of workers
Recommendations
Sqn/Unit Medical officers need to be vigilant while taking occupational history of patients, and the same needs to be carefully recorded in AFMSF-1, so as to help grant attributability/aggravation at the later date. Periodic medical examination of high risk trades need to be more focused on occupational morbidity. Permissible standards of exposure, as laid down in the Western armed forces needs to be enunciated at all work settings. Monitoring equipments could be scaled in modernization plans of SHOs, as part of Industrial hygiene cell. Intensive IEC efforts of the workers need to be undertaken by the health authorities of station to improve awareness of the health risks and the importance of safe work practices and use of personal protective measures. The emergency drill in case of injuries needs to be periodically rehearsed under medical supervision. Lastly administrative authorities need to focus on sign posting of hazards, measures of prevention, provision of adequate cool areas, cold drinking water facilities and adequate washing arrangements in the work areas.
References
- Effects on health and occupational exposure to microwave radiation (radar) Am J Epidemiology. 1980;112(1):39-53.
- [Google Scholar]
- Cerebral arterial gas embolism in air force ground maintenance crew–a case report of two cases. Avait Space Environ Med. 1999;70(7):698-700.
- [Google Scholar]
- Surveillance for work related hearing loss in UK: OSSA and OPRA 1997-2000. Occp Med (Lond). 2002;52(2):75-79.
- [Google Scholar]
- Cancer in korean war navy technicians; mortality survey after 40 years. Am J of Epidemol. 2002;155(9):810-818.
- [Google Scholar]
- Current problems in medical support for provision of radiation and chemical safety in Armed forces(Russian) Voen Med Zh. 2001;2:4-10.
- [Google Scholar]
- An enquiry into causes of repeated sickness absence in a ship repairing organisation. Indian J Pub Hlth. 1991;35(3):86.
- [Google Scholar]
- Study of traumatic cataract in occupation and environmental trauma and its management. Med J Armed Forces india. 1998;54(1):41-43.
- [Google Scholar]
- Evaluation of hearing handicap in textile mill employees with noise induced hearing loss. Indian J Otolaryng Head Neck Surgery. 1997;49(2):97-100.
- [Google Scholar]
- Hospitalisation for injuries among Finnish Conscripts in 1990-1999. Accid Anal Prev. 2006;38(1):99-104.
- [Google Scholar]
- Risk of accidents and occupational diseases among the Finnish Defence Forces. Mil Med. 2005;170(9):756-9.
- [Google Scholar]
- Diseases nonbattle injury surveillance for commander, Joint task force Haiti, 2004. Mil Med. 2005;170(12):1032-3.
- [Google Scholar]
- Air Force Guidance Memorandum to AFI. :91-203. Air Force Consolidated Occupational Safety Instruction
- [Google Scholar]
- Hearing loss in Military aviation and other trades, investigation of prevalence and risk factors. Aviat Space Environ Med. 2205;76(12):1128-35.
- [Google Scholar]
- Analysis of on ground and in flight sound levels produced by Chetak and Pratap helicopters. Ind J Arospace. 2002;46(1):51-61.
- [Google Scholar]
- Manual of Health for the Armed Forces. Ch XXVI. India: Published by Directorate General, Armed Forces Medical services; :973-74.
- [Google Scholar]
- A survey of the provision of educational supervision in occupational medicine in Armed Forces. OccupMed(Lond). 2005;55(3):227-33.
- [Google Scholar]
- Changinf heat related mortality in the United States Environ Health Perspect. . 2003;111(14):1712-8.
- [Google Scholar]
- Assesement of heat tolerance for post exertional heat stroke individuals. Med Sci Monit. 2004;10(6):CE252-7.
- [Google Scholar]
- Heat hyperpyrexia: time to act In: Indian J Med Res 119. 2004. p. :vii-X. Editorial
- [Google Scholar]
- Health status of personnel occupationally exposed to radiowaves. ArhHigRadaToksikol. 1993;44(3):223-8.
- [Google Scholar]
- Epidemiologic evidence relevant to radar (Microwave) effects. Environ Health Perspect. 1997;105(Suppli 6):1579-87.
- [Google Scholar]






