Translate this page into:
Renal stone risk index assessment in potential Indian astronauts
-
Received: ,
Accepted: ,
Abstract
Human exposure to microgravity the unique low-gravity environment inside the spacecrafts results in a number of physiological changes to the human body. Among these changes are alterations in renal function, fluid redistribution, bone loss and muscle atrophy, all of which contribute to an altered urinary environment and the potential for renal stone formation during and immediately after flight. Previous data have demonstrated that human exposure to microgravity increases the risk of renal (kidney) stone development during and immediately after space flight. In-flight changes previously observed include decreased urine volume and increased urinary excretion of calcium, phosphate, and sodium. Urine from 50 healthy subjects reporting for annual medical examinations to the laboratory was collected. Following parameters were analysed to formulate average biochemical values of these solutes in Indian population:- volume, sodium, potassium, pH, citrate, uric acid, oxalate, calcium, creatinine and phosphate using manual and automated methods. Further 16 healthy volunteers were exposed to a 6 hour simulated space environment using the head down tilt method. The urine collected before the head down tilt, during the experiment and after the head tilt were analysed for the same biochemical parameters. The results revealed that there was a significant change in values of sodium, potassium, pH, citrate and uric acid. The paper has tabulated an average value of various urinary solutes in Indian population that can be used as a reference during the selection of an Indian astronaut for future space missions wherein the risk of development of renal stone in the aircrew will be minimal during the spaceflight. The paper also proposes a Renal Stone Risk Index (RSRI) nomogram assessment to predict the renal stones in future.
Keywords
Renal stone
Risk assessment index
Urinary biochemical analysis
Introduction
The astronauts in space are prone to develop renal stones due to increased calcium excretion (as a consequence of demineralisation). Certain human beings are as such more prone to develop renal stones due to higher urine calcium, oxalate or uric acid excretion. These individuals simultaneously may have a low citrate or sulphate which are normal chelators of calcium in urine.
During spaceflight, the development of a renal stone may not only impact the health of the crewmember, but also the success of the mission. The relative remoteness of the spaceflight environment renders complications particularly worrisome. Specifically the issues for spaceflight includes the following:-
The potential for forniceal rupture that temporarily releive the severe colic but causes a retroperitoneal urinoma subject to infection and diffuse ileus.
Infection behind the level of obstruction that, due to increased pressure, increases the risk of urosepsis.
A crewmember’s inability to maintain oral hydration due to the ileus. Any of these can lead to early mission termination[1].
This study has laid down the accepted levels for Indian population which will act as a benchmark for selection for astronaut
Material and Methods
50 healthy subjects were included in the study. Inclusion criteria were age between 20-35 yrs, Male. Exclusion criteria were known cases of renal/ endocrine disorders, subjects on any kind of medication. The subject abstained from alcohol and caffeine at least 12 hrs before the commencement of the test. The subject was asked to take a low fat vegetarian meal a night before. A 24 hr urine sample collection for these 50 healthy subjects was carried out. The urine was analysed for calcium, oxalate, uric acid, pH, citrate, creatinine, sodium and potassium levels. The electrolytes were measured by selective ion- electrode analyser- AVL 9180. Uric acid, phosphates, and creatinine were assayed by ERBA Chem 5 plus semi-autoanalyser using DDS Diagnostic Sytem® and Autopak® serum kits. Phosphates was measured by photometric UV (ammonium molybdenum) method with 1:20 urine dilution with distil water at 340 nm. Enzymatic uricase TBHBA method was used for estimating urinary uric method using 1:10 dilution. Urinary creatinine was estimated using Jaffe’s kinetic method with1:50 dilution of urine. The readings were taken at 492nm. Citrate was measured using citrate lyase method (phenyl hydrazine reaction). Commercial kits of R-Biopharm GmbH, Germany were used for this analysis. Advance DPX 300 MHz FT- Spectrophotometer was used for the measurement at 760 nm. Calcium was estimated using atomic absorption method. Oxalate was estimated by oxalate oxidase method using commercial kits of Sigma (St Louis No. 590). The above-mentioned spectrophotometer was used. The total volume was also measured. pH estimation was done using reagent strips.
16 volunteers amongst the 50 subjects were then subjected to a 6 hr 6° head down tilt simulating the space environment. The subject took a standard breakfast of 450 Kcal and two glasses of water, 1 hr before the procedure. The procedure was explained to each subject in the language they understood and a formal written informed consent was taken. A medical investigator closely monitored his pulse, blood pressure at regular intervals. After 3 hrs, he voided urine in a urinal while lying in the tilted position. After 6 hrs in lying position, the subject was again asked to pass urine in a test tube. For next 18 hr, the urine was collected in the same container. Same parameters were analysed on this 24 hr urine collected.
Results
The average mean values of the solutes was analysed in 24 hr urine collection from the 50 healthy subjects not suffering from any metabolic disease. These values are shown in Table 1.
| Sl No. | Urinary Analyte (Unit) | Method & Kit | Instrument | Mean Value (Range) | Expected Values | Sensitivity/ Limit of detection (LOD) |
|---|---|---|---|---|---|---|
| 1. | Total Volume (L/day) | Measuring cylinder | 1.78 (±0.2) | 0.9 -2.1 | ||
| 2. | pH | pH reagent strip | 6.16 (±0.08) | 05-07 | ||
| 3. | Calcium (mg/day) | Atomic absorption Spectrophotometry | Avance DPX300 MHz FT- Spectrophotomtr | 189.7(±6.61) | 100-300 on an average diet | |
| 4. | Phosphate (mg/day) | Photometric UV Test (Ammonium Molybdenum) | Erba Chem 5+ Semiautonalayser | 1031 (±29.89) | 700-1300 | 0.7 mg/dl(lower LOD) |
| 5. | Oxalate (mg/day) | Oxalate oxidase method (Kit: Sigma (St Louis No. 590) | Avance DPX300 MHz FT- Spectrophotometer | 42.3 (±0.92) | 07-48 | |
| 6. | Sodium (meq/day) | Selective Ion electrode Snap Pack AVL (Urine diluent- BP 0344) | AVL 9180 (Roche) | 185.6 (±5.58) | 40-220 | |
| 7. | Potassium (meq/day) | Selective Ion electrode Snap Pack AVL(Urine diluent - BP 0344) | AVL9180 (Roche) | 65.9 (±1.77) | 25-120 | |
| 8. | Citrate (mg/day) | Citrate Lyase method- Phenyl hydrazine reaction (R-Biopharm GmbH, Germany) measured at 760 nm | Avance DPX300 MHz FT- Spectrophotometer | 689.6 (±15.57) | 450-750 | 0.08 mg/dl(lower LOD) |
| 9. | Uric Acid (mg/day) | Uricase TBHBA method | Erba Chem 5+ Semiautonalayser | 593 (±15.2) | 800 assuming normal diet | 0.07 mg/dl(lower LOD) |
| 10. | Creatinine (mg/day) | Kinetic Jaffe’s Reaction | Erba Chem 5+ Semiautonalayser | 1080 (±87.2) | 14-26 mg/kg/day | 0.2 mg/dl(lower LOD) |
The urine samples of 16 volunteers received before and after the head tilt was analysed for various biochemical parameters. The results are tabulated in Table 2. The data is represented as mean with (+/- ranges). Statistical analysis was done by paired t-test.
| Sl No. | Analyte | Before head tilt | After head tilt | p value |
|---|---|---|---|---|
| 1. | pH | 5.99 (0.06) | 5.34 (0.06) | < 0.001 |
| 2. | Calcium (mg/day) | 198.3 (5.86) | 201.5 (6.88) | 0.089 |
| 3. | Phosphate (mg/day) | 1063.6 (26.56) | 988.9 (21.53) | 0.127 |
| 4. | Oxalate (mg/day) | 38.7 (0.92) | 37.8 (0.87) | 0.365 |
| 5. | Sodium (meq/day) | 173.1 (3.56) | 209.6 (3.63) | < 0.001 |
| 6. | Potassium (meq/day) | 67.1 (1.28) | 52.7 (1.1) | < 0.001 |
| 7. | Citrate (mg/day) | 711.6(14.46) | 629.2 (11.56) | < 0.001 |
| 8. | Uric Acid (mg/day) | 629 (13.2) | 749.7 (11.56) | < 0.001 |
| 9. | Creatinine (mg/day) | 1366 (43.2) | 1299.3 (28.81) | 0.106 |
Discussion
Studies have shown that immediately after spaceflight, the risk of calcium oxalate and uric acid stone formation is increased as a result of metabolic (hypercalciuria, hypocitraturia, pH) and environmental (lower urine volume) derangements, some of which could reflect residual effects of having been exposed to microgravity. Other factors contributing to increased risk include increased urinary calcium oxalate supersaturation, while urinary citrate, magnesium and volume are all decreased [2].
Hypercalciuria has been associated with calcium nephrolithiasis since 1939 and was noted during flight and immediately after landing in Skylab astronauts [3]. With normal anatomy, crystals form when the urine is supersaturated with minerals i.e. when the concentration of stone forming salts exceeds the solubility of the salt in solution and the solubility product exceeds the threshold for precipitation. High levels of cortisol in serum and urine due to physical/psychological stress also promotes demineralisation of the bones. The urinary calcium value of >250 mg/day signifies hypercalciuria. In weightlessness in space there is resorptive hypercalciuria due to excess demineralisation of bone mass. Due to reduced gravity the bones sense a decreased load and increased IL-2 is released which stimulate the osteoclast activity more than the osteoblastic activity. This leads to increased mobilization of calcium from bones onto the circulation. Simultaneously more creatine kinase B is secreted in microgravity which inhibits the normal functioning of the osteoblasts [4]. Our study showed an average value of 189.7 mg/day in Indian population. Since the simulated space environment exposure was too short to cause activation of osteoclasts no significant increase in urinary calcium was noticed after the head down tilt. Neither was significant rise in oxalate levels noted. An increase in oxalate by itself does not raise the chance of stone formation until and unless there is a simultaneous rise in calcium excretion in urine.
Microgravity alters the fluid electrolyte balance through alterations in the hormones. In flight studies has shown an increase in Anti Diuretic Hormone (ADH), decrease in Aldosterone and decrease in Atrial Natriuretic Factor (ANF) [5, 6]. On exposure to the weightlessness, there is cephaloid shift of blood leading to immediate sense of volume overload. The hormonal alteration leads to increase sodium loss in urine and decrease in potassium excretion. Similar change was noted in our head down tilt experiment. Urinary creatinine excretion was found to be unaltered post space environment simulation.
Ions such as citrate, magnesium and phosphate inhibit renal stone formation by binding to calcium and forming soluble complexes. Citrate and phosphate binds directly to calcium thereby decreasing the available calcium for stone formation. Urinary citrate also prevents calcium oxalate crystals from aggregating into larger crystals and into renal stones. In addition, citrate makes the urine less acidic which inhibits the development of uric acid stones [7]. Magnesium acts as an inhibitor of stone formation by complexing with oxalate available for calcium oxalate stones. Studies on use of potassium citrate pills have been done in astronauts to minimise chances of renal stone formation. Our study showed average values of 619 mg/day for urinary citrate and 1031 mg/day for urinary phosphate. On analysing 50 samples we can postulate that shortlisted aircrew with urinary citrate < 450mg/day (hypocitraturia) and phosphate <700 mg/day classify for rejection of an astronaut. In our study an 6 hr of head down tilt showed a significant reduction in urinary citrate (p<0.001).
A low pH promotes formation of calcium, phosphate and uric acid stones. The fall in pH in our experiment was significant. Hence we recommend use of alkalinizing agents along with citrate pills to prevent stone formation. Uric acid stones make up 6-8% of the total urinary stones in humans and are more common in patients suffering from gout. In our study there has been a significant rise in the uric acid levels after the simulated space environment [6].
Other factors that promote solute precipitation in an astronaut include reduced urine flow as the amount of fluid intake is minimal due to rationed water availability. Space motion sickness further reduces the intake of fluids due to fear of emesis. Spaceflight involves several activities associated with long periods in environments that make it difficult to void or access fluids. During 6 hr extravehicular activity there is loss of 1-2 ltr of water due to perspiration (high pressure insulated suit) and insensible loss thereby leading to a dehydration state promoting stone formation. [1]
During an astronaut selection, the conditions that predispose to renal stone and should be ruled out are recurrent urinary tract infection, indwelling foreign bodies, anatomical anomalies (medullary sponge kidney, solitary/polycystic kidney) and bladder outlet obstruction. Metabolic disorders like hyperparathyroidism, sarcoidosis and gout should be screened out. Genetic predisposition to stone formation often involves familiar hypercalciuria syndromes that can be due to the following:-
Absorptive hypercalciuria, where excessive calcium is absorbed from the gastrointestinal tract may result from excess dietary calcium.
Nephrogenic or renal hypercalciuria the kidneys filter out calcium from the blood but do not allow the resorption of the calcium back into the blood from the renal tubules. Medications and supplements may induce hypercalciuria by increasing intestinal absorption, adding directly to the calcium load (antacids), calcium supplements or enhancing renal calcium excretion (acetazolamide).
Diet rich in calcium, purine, dairy excess, oxalate and sodium also predisposes to stone formation. Ironically a diet too low in calcium may also promote calcium oxalate stone formation. Normally a large fraction of intestinal oxalate is bound to calcium and undergoes faecal loss. With inadequate dietary calcium the hyperoxaluria may result from absorption of unbound oxalate from intestine.
In the history of the US programme, 14 renal calculus events in 12 astronauts have been recorded out of a total of 332 flown astronauts. Four of these occurred before flight (not associated with space flight) and ten occurred within 2 yrs post flight. Two crewmembers have experienced multiple renal stone episodes. In the history of Russian space programme, three cosmonauts have been identified with post flight urinary calculi. Subsequent evaluation of these cosmonauts revealed that they did not have any anatomical or metabolic defect. One cosmonaut developed a presumed renal stone during a long duration mission that caused severe pain and significantly impacted the in-flight timeline. Several studies have documented a reduced fluid intake by astronauts in first 6 days of mission due to motion sickness, increased excretion of calcium, phosphates, sulphates, sodium and potassium in urine [1]. Skylab data indicated that nine crewmen decreased their fluid intake by approximately 700 ml in first six days [3]. No changes in creatinine have been documented.
As a countermeasure, diet advised to astronauts is low in oxalate content and reduced in animal proteins that are high in purine. Water intake should be high to achieve a urine output of 2 ltrs/ day. Potassium citrate tablets should be taken to minimise development of crystals and growth of stones. The side effects known with this pharmacologic intervention are abdominal discomfort, vomiting and diarrhoea. These risks may be minimised by ingestion of sustained release tablets [8]. The bone resorption due to microgravity can be inhibited by physical loading of bone (exercise countermeasures) and pharmacological drugs like biphosphonates that reduce the function of osteoclasts.
Renal Stone Risk Assessment
Although the urinary risk profile does not directly predict the formation of renal stones, it illustrates to the medical officer the current urine chemistry environment [9]. We recommend further large scale studies including more parameters like 24 hr urinary magnesium and sulphates measurement. We propose renal stone risk index assessment nomogram that can predict the chances of future renal stone formation. This index is depicted in Fig. 1. This relatively low cost highly effective methodology of renal stone risk profile can mitigate the abortion of an important space mission. Crew members experiencing an increased risk of stone prior to mission can be exposed to simulated microgravity environment with resultant bone loss, hypercalciuria and exact measurement of solutes in urine can be done.
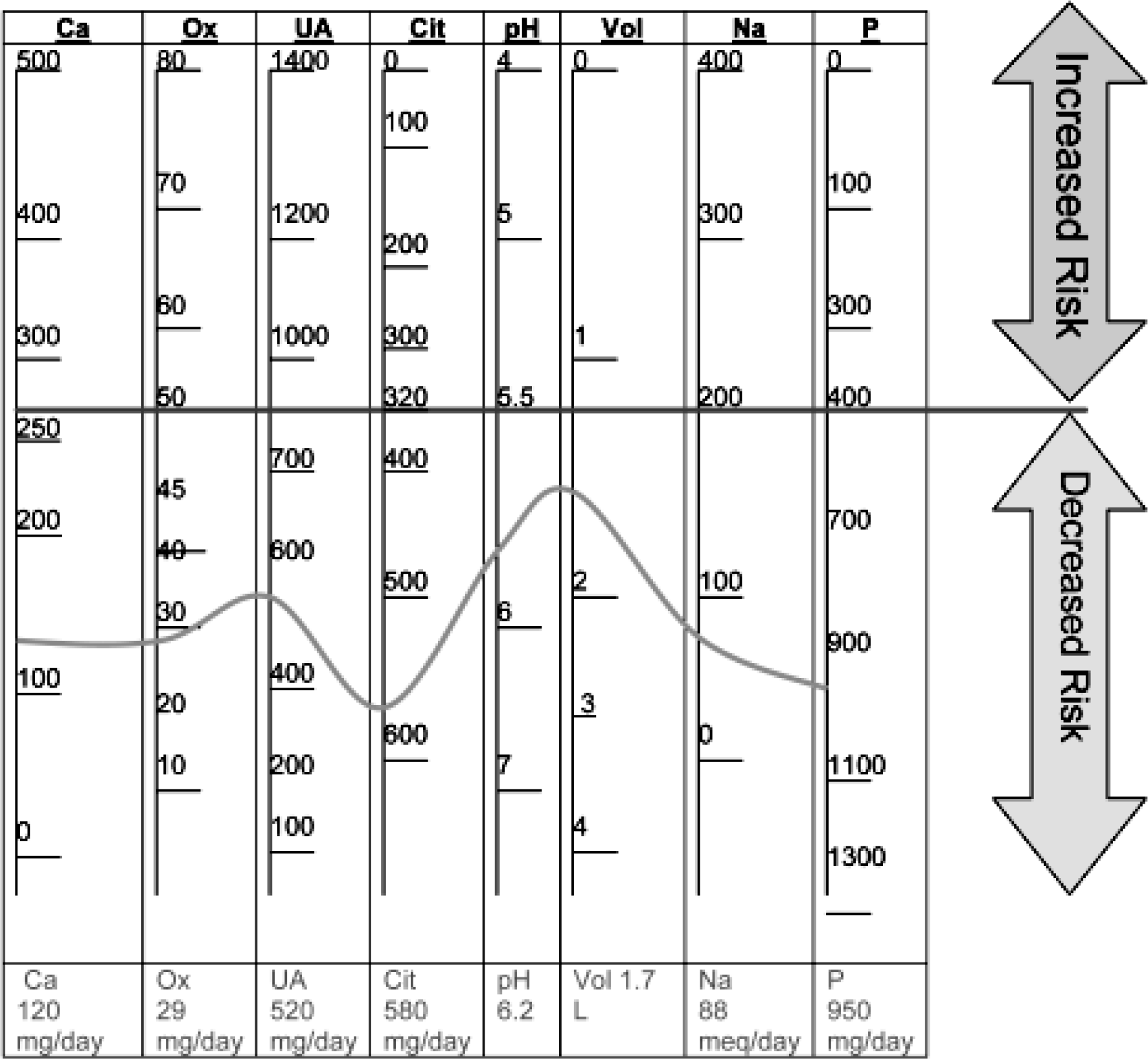
- Renal stone risk assessment index (values above the red line signifies as a risk factor); The blue line and figures depict an example of the plotted index of a healthy Indian male.
Conclusion
Renal stone formation continues to a remote but a dreaded complication in space flight. Formation of a stone during spaceflight can be detrimental to the goal of the mission. The medical officer during screening and selection of an Indian astronaut for space mission can predict future renal stone formation by investigating various solutes in the urine and plotting it in the proposed nomogram. They can also advise necessary countermeasures especially to candidates having altered urinary solutes.
Conflict of interest: None
References
- Renal and genitourinary concerns In: Baratt MR, Pool SL, eds. Principles of Clinical Medicine for Space Flight 2nd Ed. New York: Springer; 2008. p. :273-92.
- [Google Scholar]
- The risk of renal stone formation during and after long duration space flight. Nephron. 2001;89:264-70.
- [Google Scholar]
- Observations in energy balance in man during spaceflight. Am J Physiol. 1977;233:208-12.
- [Google Scholar]
- Animal development in microgravity In: Clement G, Slenzka K, eds. Fundamentals of space biology. Vol 18. Springer; 2006. p. :171-226.
- [Google Scholar]
- Changes in renal function and fluid & electrolyte regulation in spaceflight In: Book of abstracts. Washington DC: World Space Congress; 1992. Paper No. IAF/IAA-92-0256;81-2
- [Google Scholar]
- Renal stone formation among astronauts. Aviation Space and Environmental Medicine. 2007;78(1):A9-A13.
- [Google Scholar]
- Renal stone risk during space flight: Assessment and countermeasure validation. Expeditionthree, ISS Mission 7A.1, STS-105 Space Shuttle Flight In: NASA technical report 07/ 2001.
- [Google Scholar]
- Mathematical model to estimate risk of calcium-containing renal stones. Mineral and electrolyte metabolism. 1999;25:199-203.
- [Google Scholar]






