Translate this page into:
Pulmonary fat embolism in IAF aircraft accident fatalities: A 33 year retrospective study
Abstract
A 33 year retrospective study of aircrew fatalities was done. Out of 587 autopsies studied, histological sections from lungs were available in 392 cases. It was observed that only 5.1% cases showed microscopic evidence of pulmonary fat embolism. The aetiological factors were correlated with presence of fat embolism. The significance of pulmonary embolism has been highlighted in relation to aircraft accident investigation.
Keywords
Fat embolism
Timing of injury
Fat embolism in today’s clinical scenario is commonly seen during long standing orthopaedic procedures viz. spinal body surgeries, intramedullary nailing, total hip replacement and intraosseous infusions in pediatric rehydration protocol.
The reconstruction of fatal aircraft accident from medical findings depends to a large extent on timing of injury. It is difficult to do so in aircraft accidents, as trauma is widespread. Gross appearances are of some aid e.g. a bloodless fracture suggests a postmortem injury.
Studies have shown that presence of pulmonary fat and bone marrow emboli correlates well with evidence of antemortem fracture [1]. In 1965 Armstrong and colleagues in their report on Comet disasters showed the possibility of using tissue embolism in lungs as a means of demonstrating antemortem violence [2]. There has been conflict in literature as to the distribution of fat embolism in different lobes of lungs. Scully found that there is no particular localization of emboli and that findings are uniform throughout the lung [3].
Mason showed a contradictory finding showing that more extensive the injury, lesser the grades of embolism [1]. This was explained with simultaneous breach of cardiovascular system.
This study has been conducted to find out the incidence of fat embolism in lung tissue as encountered during autopsies conducted. These findings were then compared to various studies and other factors.
Materials and methods
A retrospective study was carried out at the Department of Aviation Pathology, Institute of Aerospace Medicine, IAF, Bangalore on 587 autopsies conducted on aircrew fatalities between 1970 and 2003. All types of aircrashes and fatal ejections were included in this study, irrespective of circumstances of accidents. MS 1956 (Medical Report on Fatal Aircraft Accident) consisting of autopsy reports, investigations, court of inquiry findings was studied. The histological sections stained with Sudan III (fat stain) was available in only 392 cases. Two independent pathologists reviewed these slides. The H&E sections were also reviewed for evidence of fat embolism (Photo 1 and 2).
Results
The age of aircrew ranged from 20 to 38 years (mean 27.9 years). The total number of autopsies conducted were 587. The lung tissue was retrieved in 392 (66.7%) cases. Fat emboli was seen in 20 (5.1%) cases. 313 had disintegration injuries. The corrected percentage for fat embolism is 25.3%.
The pulmonary fat embolism was graded according to Mason classification and is shown in Table 1 and Fig 1.
The cases having fat embolism were further classified on the basis of the phase of flying in which the accident took place. The incidence is shown in Table 2.
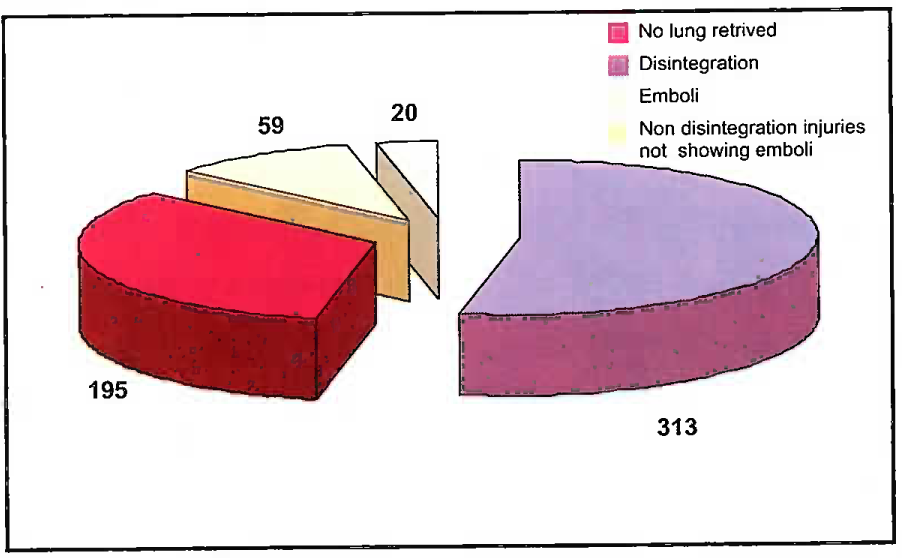
- Showing the incidence of pulmonary fat emboli in fatal aircraft accidents
| Grade of Emboli | Description (Fatal injuries) | Number (n = 79) | % |
|---|---|---|---|
| 0 | No emboli seen | 59 | 74.6 |
| I | Emboli found after some search | 12 | 15.1 |
| II | Emboli easily found | 6 | 7.5 |
| III | Emboli present in large number | 2 | 2.5 |
| IV | Emboli present in fatal concentration | 0 | 0 |
| Phase of Flying | Fat Emboli (n 20) | Normalised % |
|---|---|---|
| Take off (n=26) | 8 | 30.7 |
| In flight (n=27) | 3 | 11.1 |
| Mid Air | 1 | |
| Collision | ||
| Hying | 1 | |
| Failure to recover from spin | 1 | |
| Ejection (n=10) | 1 | 10 |
| Landing (n-16) | 8 | 50 |
Chi Square test of statistical significance was applied. It was found that the frequency of fat embolism was significantly higher during the landing phase (p<0.05).
All cases showing fat embolism were reviewed to see whether the victim had signs of antemortem burns based on the levels of carboxyhaemoglobin and histopathological changes. The incidence is shown in Table 3.
Types of injuries causing death were classified into disintegration, multiple injuries, head injuries, limb fractures and spinal fractures.
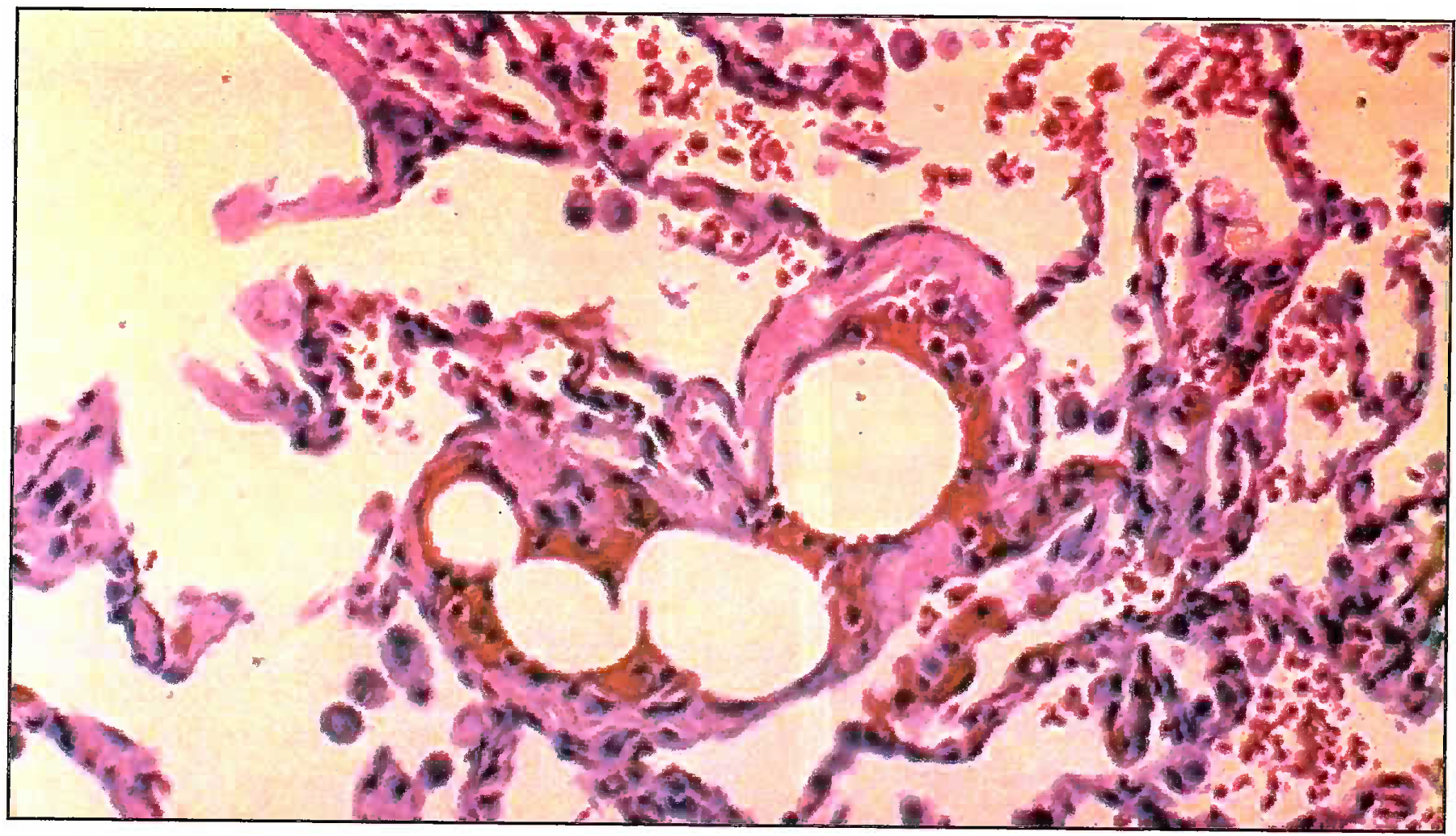
- Microphotograph showing fat emboli in pulmonary vessel (400X) Grade II
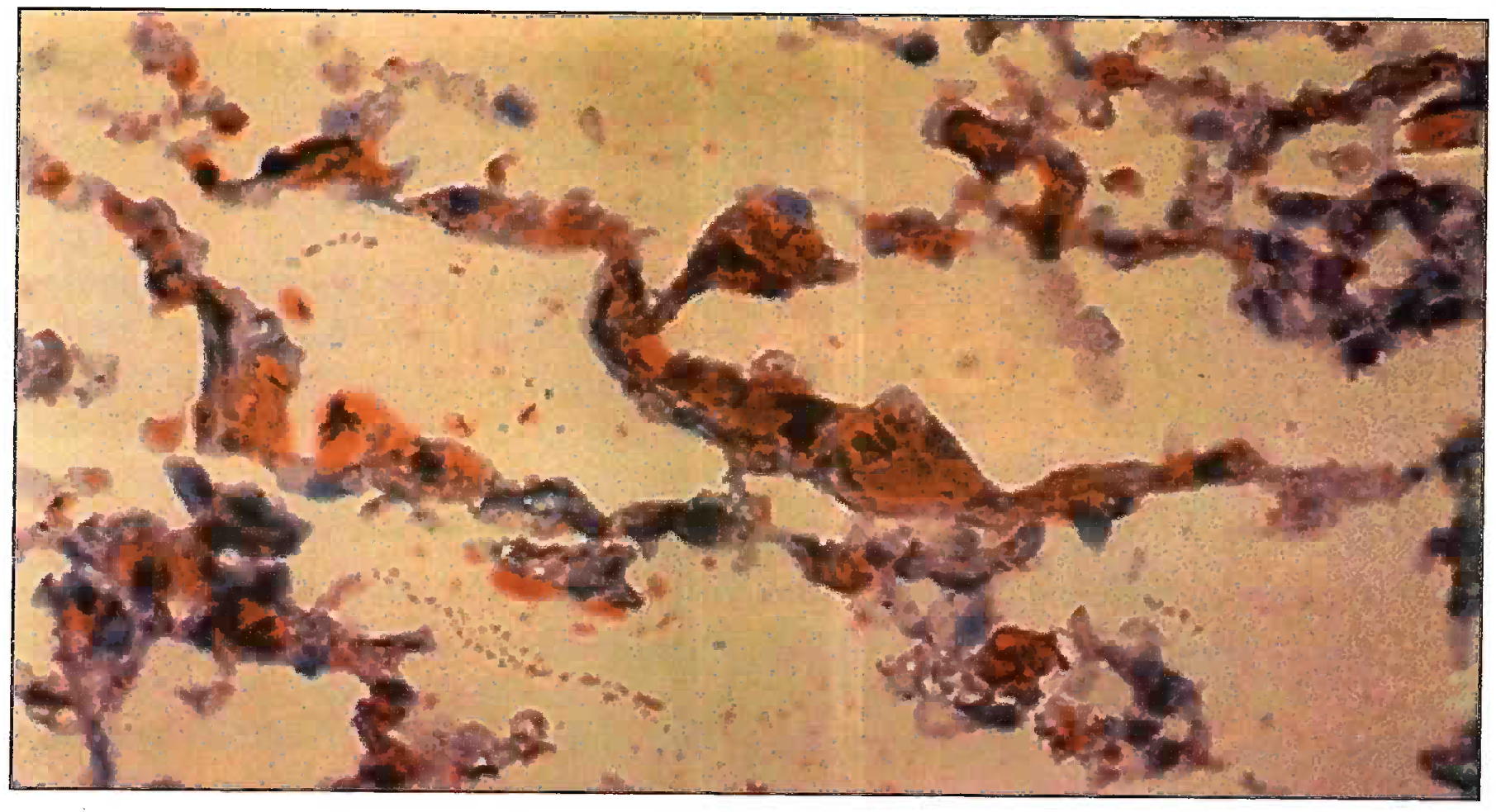
- Sudan Black III Stain Microphotograph showing fat emboli in pulmonary vessel (400X) Grade III
| Antemortem Burns | Number | % |
|---|---|---|
| Present | 7 | 35 |
| Absent | 13 | 65 |
Incidence of pulmonary fat embolism from each group is shown in Table 4.
| Type of Injury (n=79) | No. of cases showing embolism | % |
|---|---|---|
| Limb fractures (n=21) | 6 | 28.57 |
| Multiple injury (n-33) | 11 | 33.3 |
| Head injury (n=16) | 2 | 12.5 |
| Spineinjury (n=6) | 1 | 16.6 |
| Disintegration (n=3) | 0 | 0 |
Chi square test was applied to determine the significance. On correlating the rate of formation of fat embolism and type of injury sustained, it was seen that there was no statistically significant difference between the frequency of fat embolism and type of injury. No disintegration case showed a fat embolus.
| Bone Marrow embolism | Number (n=20) | % |
|---|---|---|
| Present | 5 | 25 |
| Absent | 15 | 75 |
Discussion
Presence of pulmonary fat embolism has been known for decades as means for determining presence of antemortem injuries in motor and aircraft accidents. Table 6 shows incidence of pulmonary fat embolism as reported by various authors. The result of various studies were statistically compared to present study and it was found that the findings were not significantly different from the study of Adaval et al. (Chi square test p> 0.05) [4]. The low incidence of pulmonary fat embolism in our study as compared to other studies could be due to inclusion of death by disintegration in our studies. After removing the disintegration injuries the corrected occurrence of pulmonary fat embolism is 25.3%. The incidence is still low compared to studies done abroad. This can be due to low number of lung sections sent to the Institute.
The grade of embolism depends on the intact circulation and cardiac function for a longer time. On analyzing the phase of flying with the positivity of pulmonary fat embolism it was found that maximum number were found in landings where the chances of survival are higher.
The occurrence of simultaneous bone marrow embolism was sought in the pulmonary fat embolism cases. The incidence is shown in Table 5. Two pathologists analyzed the histopathological findings of lungs in 79 non-disintegration fatal aircraft accidents. The first pathologist was able to identify fat embolism in 18 (22.7%), whereas the second pathologist identified fat embolism in 20 (25.3%) cases. The numbers were not different statistically.
Lynch et al (1959) described an association between pulmonary fat embolism and antemortem bums [6]. This view was negated by a subsequent report by Milosavich (1960) who stated that all antemortem injuries are not linked with aircraft fire showing the above correlation to be statistically insignificant [7]. In our study 35% cases of positive showed signs of antemortem bums.
| Year | Authors | Incidence % | Source |
|---|---|---|---|
| 1931 | Vance | 42 | 164 Injury cases |
| 1958 | Hickey & Stembridge | 51 | 236 Aircraft accident deaths |
| 1980 | Adaval & Kunzru [4] | 25 | 182 Aircraft accident deaths |
| 1983 | Bierre AK [5] | 35 | 78 New Zealand Airliner crash |
| 2003 | Present study | 5.1 | 392 Aircraft accidents deaths |
| 2003 | Present study | 25.3 | Corrected for nondisintegration injuries |
Grant and Reeve in their study also concluded that 28% of fat embolism cases showed bone marrow embolism [8]. Bone marrow embolism is less common than fat embolism (Photo 3). This can be explained by two factors :
(a) Fat embolism occurs with a greater rapidity than bone marrow embolism.
(b) It is also known that the bone marrow emboli resolve faster.
In our study, 25% cases of pulmonary embolism showed bone marrow embolism. There was no case showing isolated bone marrow embolism. While the presence of bone marrow emboli almost certainly indicates antemortem violence, failure to demonstrate emboli does not prove the contrary. More the number of lung sections taken more are the chances of picking up emboli.
On correlating the frequency of fat embolism and type of injury sustained, it was seen that there was no statistically significant difference between the frequency of fat embolism and type of injury. No disintegration case showed a fat embolus further confirming the significance of intact circulation for the formation of embolus.
A study carried out by Spann (1959) to correlate the degree of fat embolism with laceration of heart and aorta revealed that the grade and extent of embolism was relatively more with atrial injuries than ventricular rupture [9]. Warthin emphasized that when many bones are broken the fat may pass into vascular system in few seconds [10]. Scully proved that fat embolism can arise from trauma to subcutaneous fat in ejection cases with no fractures [3].
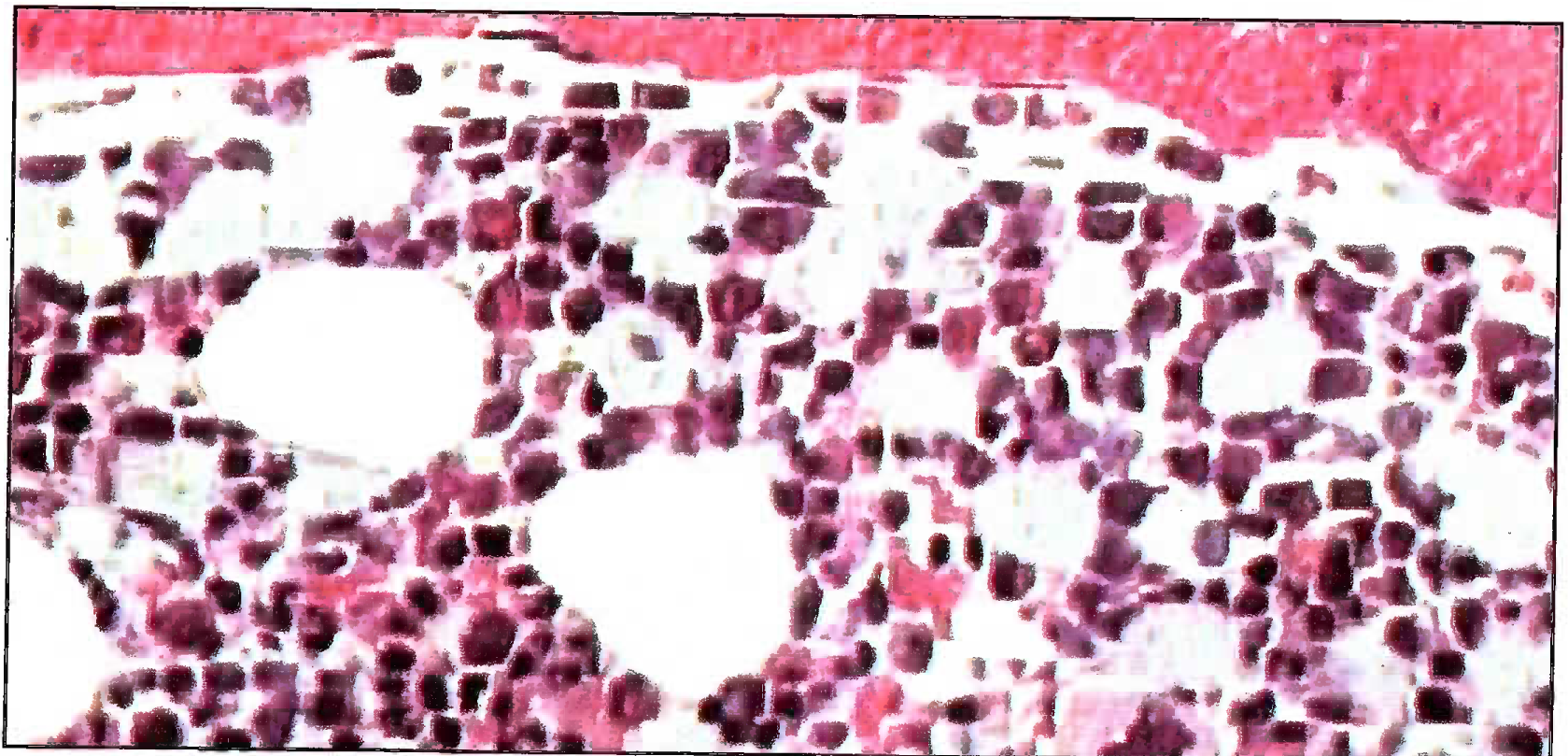
- H & E Microphotograph showing bone marrow emboli in pulmonary vessel (200X)
There was an older hypothesis stating that the major trauma to body used to alter the blood chemistry and lead to coalescence of chylomicrons forming emboli. Later this hypothesis was disproved by coexistent presence of bone marrow emboli. In 1989 Richter came with a theory of fat embolism arising as a consequence of increased C-reactive proteins [11]. This finding was proved to be statistically insignificant by various authors.
Rait drew attention to similarities between fatal fat embolism and fatal decompression sickness (DCS) [12]. He hypothesized that the fat embolism causes the blockage of vessels and results in the symptoms of decompression sickness. This view was unacceptable, as degree of fat embolism is so slight that it would be implausible to invoke such drastic symptoms. Secondly, the presence of air bubbles in the pial vessels during autopsy of a pilot dying due to DCS further confirms the theory of nitrogen bubbles as a cause of DCS and not fat embolism. Haymarker and Johnston assumed that fat emboli were the outcome of rupture of fat cells secondary to intracellular bubble formation [13].
The concurrent presence of fat embolism and fatty liver was seen by Haymarker and Johnstone [13]. This was earlier explained by the hypothesis that the liver is the organ filtering off the excess fat in circulation. Due to trauma the fat embolus formed from the bone marrow was getting filtered in liver. This theory was negated by the absence of high lipids in plasma of deceased pilots’ [14]. The second hypothesis, which is accepted is that fatty liver on rupture led to the dislodging of fat to circulation causing embolism [12].
Conclusions and Recommendations
An early retrieval and processing of large amounts of lung tissue are neccessary for better results. A minimum of 5 tissues, one from each lobe of lung should be sent to IAM for histopathological examination. The squadron medical officer / aviation medical specialist should always accompany the army/civil pathologist during the conduction of autopsy to explain the aeromedicai significance of various findings. The pathologists reviewing the lung slides should meticulously search for emboli in all the H&E sections and Sudan III stained slides. Pulmonary fat embolism is a time-tested mode of ascertaining an antemortem injury in aircraft accidents and will continue to be so.
References
- Timing of injuries In: Aviation Accident Pathology - A study of fatalities (1st ed). London: Butterworths; 1962. p. :239-68. In:
- [Google Scholar]
- Correlation of pulmonary fat embolism and fatalities due to bums. Lancet. 1959;2:123-5.
- [Google Scholar]
- Fat emulsion agglutination test-an alternate to CRP. Clinical Chem Acta. 1997;281:141-48.
- [Google Scholar]






