Translate this page into:
Proteinuria in Indian aviators
-
Received: ,
Accepted: ,
Abstract
Proteinuria is a condition occasionally detected both in military and civil aircrew. Medical personnel of Indian Armed Forces and civil involved in the care of either group require a standardized policy for the evaluation and aeromedical disposition of personnel with proteinuria. A two year retrospective study of all proteinuria reported in a large service evaluation centre was carried out. The pilots/candidates having proteinuria were further evaluated with the grade of proteinuria, renal function tests and imaging. A literature search was also conducted to obtain current information and prognostic data on proteinuria in the general medical literature. Generally accepted waiver principles were then examined to determine if proteinuria should be waivered in aviation personnel. Other agency policies regarding proteinuria in aviation personnel were examined. 102 out of 4416 aviators undergoing medical examination had proteinuria (incidence 2.3%). The general population (non aviators reporting to laboratory) proteinuria in this study was 4%. The commonest causes of proteinuria were urinary tract infection (73%), followed by renal calculi (7%) and orthostatic proteinuria (8%). 9 aviators had proteinuria as a result of other causes. The disposals and waiver policy for aviators have been discussed. This study further recommends the algorithmic approach to evaluate and the aeromedical disposition of aviation personnel with proteinuria. The study also brings out the common reasons for false positivity and false negativity of urinary proteins using dipsticks.
Keywords
Proteinuria
investigation
aeromedical disposition
Proteinuria is an occasional finding in the general population and is therefore sometimes encountered in the examination of personnel in the aviation field. The patho-physiological processes that cause proteinuria can lead to renal insufficiency or failure along with their attendant signs and symptoms (fatigue, susceptibility to infection, edema, electrolyte disturbances, etc.). These signs and symptoms are incompatible with aviation duties as are some of the underlying processes themselves. Short-term aeromedical concerns include the possibility of incapacitation, with the long-term consequences (in addition to impaired health) potentially leading to the undesired shortening of a full aviation career.
Proteinuria is occasionally detected among aviators as well. For assessment of a candidate during initial medical examination for ruling out renal ailment history should exclude any alteration in micturition (dysuria/frequency), recurrent attacks of cystitis; pyelonephritis or haematuria. Detailed enquiry must be made about any history of renal colic, acute nephritis, any operation on the renal tract including loss of a kidney, passing of stones or urethral discharges. If there is any history of enuresis, past or present, full details must be sought. Proteinuria in initial medical examination is a cause for rejection, unless it proves to be orthostatic. A correctable proteinuria concurrent with urinary tract infection (UTI) subsiding with antibiotics entail full renal investigation before declaring a candidate for aviations duties fit. Persistent evidence of urinary infection entails rejection. A candidate with proteinuria due to renal calculi is also unfit for intake [1].
The disposal highlighted for proteinuria in serving/civil experienced aircrew as per IAP 4303 that a cases of proteinuria should be investigated before return to duty. The disposal of such cases will depend on the cause. Functional or orthostatic type of proteinuria is of no pathological significance and such cases will be retained in full medical category [1]. The laid down guidelines do not elaborate on the steps to investigate and classify the type of Proteinuria. The waivers to be given in different types of proteinurias are also not mentioned.
Standards for entrance into the United States (US) Navy stipulate that proteinuria greater than 200 mg/day occurring more than 48 h after the last episode of strenuous exercise is a cause for rejection. These standards further state that well documented orthostatic proteinuria can be referred for waiver (“exception to policy”) consideration. A different criteria (which only mentions albumin) is imposed when joining the aviation community, where the standards for the US Navy state that the urine needs to have no albumin for the member to be physically qualified. There is no existing US Navy policy on waivers for abnormal levels of protein (of any type) detected on routine aviation physical examination. Previous waivers have been granted on an ad hoc basis only [2].
The purpose of this study was to find out incidence of proteinuria in Indian aviators with their follow up; and to develop a standardized policy for the investigation and aeromedical disposition of aviation personnel with proteinuria.
Material and Methods
A two year retrospective analysis of all the urinary protein estimation done at the institute’s laboratory was analysed. The proteinuria was tested and graded using Combistix® SG of Siemens Medical Diagnostics. The readings of the strip were taken immediately, because proteins carry a charge at physiologic pH, their presence elicit a pH change. The reagent strip is impregnated with tetrabromphenol blue buffered to an acid pH of 3. In the absence of protein the strip is yellow; 30-60 seconds following urine application, variable shades of green develop depending on the type and concentration of protein present. Results are read in a ‘plus’ system as negative, trace, and 1+ to 4+. The 24 hr urinary protein estimation was done using Esbachs regent.
Results
A total of 13,132 urine analysis was carried out at the institute’s laboratory in a period of 2 years (Aug 06 to Jul 08). Table 1 shows the incidence of proteinuria. The non aviators reporting to in this laboratory were also analysed to find out the incidence of proteinuria in general population.
| Incidence (%) | ||
|---|---|---|
| Total no. aviators having proteinuria in 2 years/Total number of | 102/4416 | 2.3% |
| urine analysis in aviators | ||
| Total no. non-aviators having proteinuria in 2 years/Total number of urine | 336/8716 | 4% |
| analysis in non- aviators | ||
| Female/Male aviators having proteinuria | 1:17 | |
| Orthostatic proteinuria in aviators/ Total number of proteinurias in aviators | 9/102 | 9% |
All cases of proteinurias without evidence of UTI underwent a repeat protein examination after 24 hrs. The aviators who were still positive for proteinuria subsequently underwent 24 hr urinary protein estimation. These aviators were then worked up as per the algorithm at Figure 1. The disposal of these cases has been tabulated at tables 3 and 4.
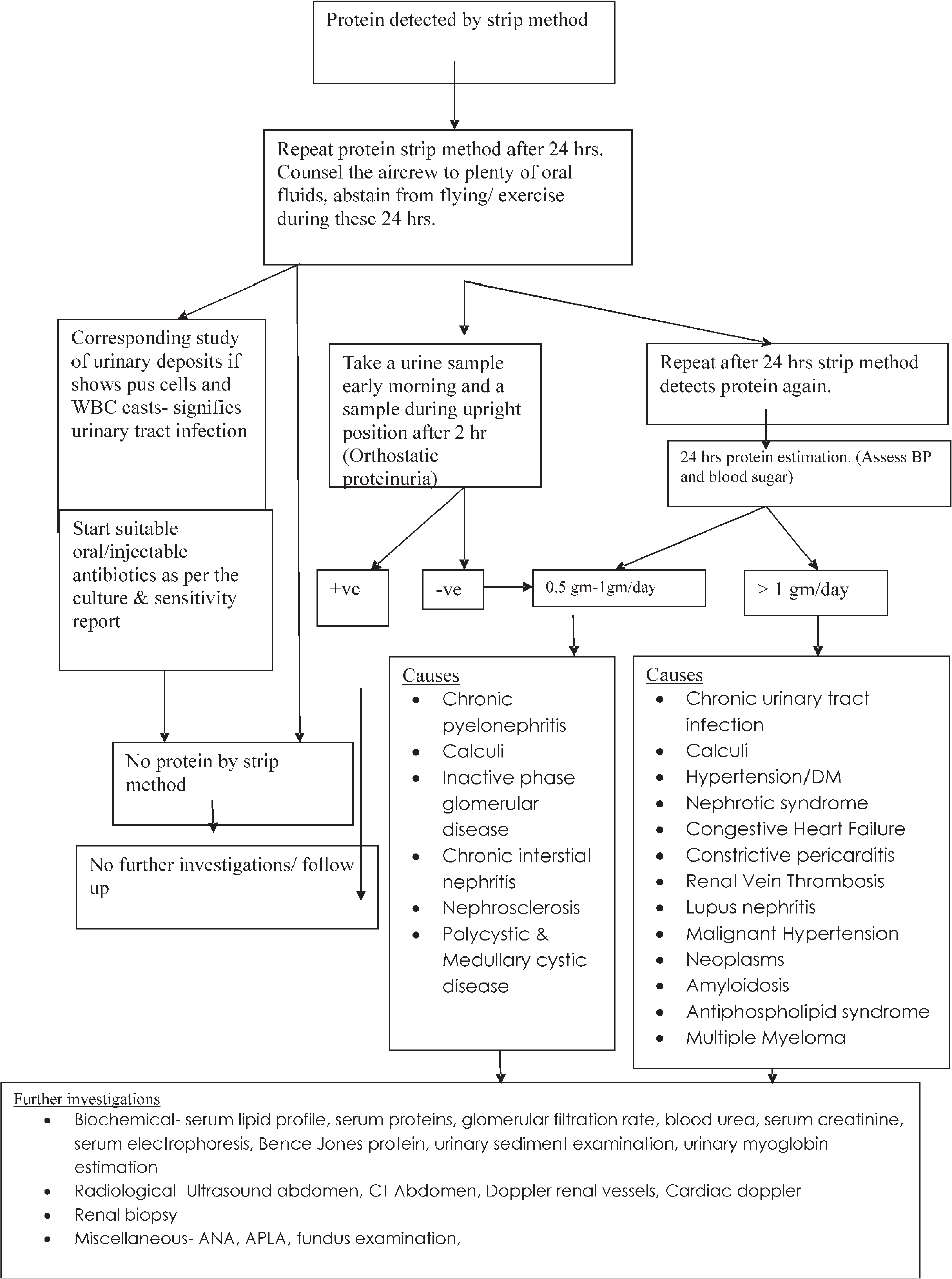
- Algorithm for investigation of an aircrew with proteinuria
| Grade | Equivalent Protein mg/dl | No. | No. after 24 hrs repeat | Presence Of Pus cells | Urine sugar (+) | Presence of calculi | Deranged renal function |
|---|---|---|---|---|---|---|---|
| Trace | < 30 | 3 | 1 | 1 | - | - | - |
| + | 30 | 56 | 49 | 37 | 3 | 2 | - |
| ++ | 100 | 29 | 28 | 26 | 4 | 2 | - |
| +++ | 300 | 13 | 13 | 8 | - | 3 | 1 |
| ++++ | >2000 | 4 | 4 | 2 | - | - | - |
| Diagnosis | Type of aircrew | Number | Protein | Disposal | ||
|---|---|---|---|---|---|---|
| 1. | Polycystic disease | Civil Candidate (Initial issue) | 1 | 0.5gm/dl | Rejected for intake | |
| 2. | Solitary renal cyst | Civil Candidate (Initial issue) | 1 | 0.5gm/dl | Fit to fly | |
| 3. | Renal/ureteric/ | Military Experienced | 2 | 0.5 gm/dl | Unfit to fly | |
| bladder calculi | Civil Candidate (Initial issue) | 4 | 0.5 gm/dl | Rejected for intake | ||
| 4. | Diabetic | Civil experienced | 4 | 0.5 gm/dl | Fit to fly as co-pilot | |
| Nephropathy | with monthly follow up of blood sugar and urinary protein | |||||
| 5. | Orthostatic | Military & Civil | 9 | 0.5 gm/dl | Fit to fly | |
| proteinuria | ||||||
| Diagnosis | Type of aircrew | Number | Protein | Disposal | |
|---|---|---|---|---|---|
| 1. | Renal/ureteric/ bladder calculi | Civil Candidate (Initial issue) | 1 | 1 gm/dl | Rejected for intake |
| 2. | Nephrotic syndrome | Civil candidate (Initial issue) | 2 | 2gm/dl | Rejected for intake |
| 3. | Diabetic Nephropathy | Civil experienced | 1 | 1 gm/dl | Fit to fly as co-pilot with monthly follow up of blood sugar and urinary protein |
| 4. | Lost to follow up | Civil candidates (Initial issue) | 5 | 1-1.5 m dl | Unfit in absentia |
Discussion
Normally, up to 150 mg of protein is excreted in the urine daily, with the average urine protein concentration varying from 2-10 mg/dl, depending on urine volume. About one third is albumin, and the remaining plasma protein includes small globulins, including á, â, and g-globulins. Plasma proteins with molecular weight less than 50000-60000 pass through the glomerular basement membrane and are normally reabsorbed by proximal tubular cells. Albumin, molecular weight 69000, is apparently filtered but only in very small amounts. Retinol binding, â2-microglobulin, immunoglobulin light chains, and lysozyme are excreted in small amounts. Tamm-Horsfall glycoprotein (uromucoid), secreted by distal tubular cells and cells of the ascending loop of Henle, constitutes about one third or more of the total normal protein loss. Immunoglubulin A (IgA) in secretions of the urinary tract, enzymes and proteins from tubular epithelial cells, other desquamated cells, and leukocytes also contribute to urine protein [3]. Proteinuria is a sign and not a diagnosis. The incidence in this study is 2.3% for aviators vis-a-vis 4% in general population. This could be possible due to a bias as the general population urine samples also included the non aviators reporting to the institute with complaints of urinary tract infection. The aviator population studied were those who reported for a routine medical examination (asymptomatic). An Indian study done in rural population (n= 5043) in south India revealed an incidence of 11% (594) in general population. However the urine analysis repeated after one week of treatment for urinary tract infections reduced the figure to 4.2% (212) [4].
Detection of an abnormal amount of protein in urine is an important indicator of renal disease because protein has a very low maximal tubular rate (Tm) of reabsorption; increased filtration of protein quickly saturates the reabsorptive mechanism. Screening methods are routinely used to differentiate normal protein excretion from abnormal, and therefore should not detect less than about 8-10 mg/dl in a normal adult with a normal rate of urine flow. The reagent strip method is sensitive to albumin; the acid precipitation methods though cumbersome detect all proteins and will therefore indicate the presence of globulins, as well as albumin. It should be noted that a very dilute random urine specimen may have a falsely low protein value. To rule out effects of dilution a spot urinary protein to creatinine ratio can be done (the normal value for this ratio is < 0.2). Exceptionally alkaline and/or highly buffered urine samples may give positive results in the absence of significant proteinuria (e.g., an aircrew on alkaline medication or with bacterial contamination). False positive results can also occur with quaternary ammonium compounds, amidoamines in fabric softeners, chlorhexidine, and with excessive wetting of the strip. Dipstick testing of urine for protein concentration has a sensitivity of about 88% and a specificity of about 96%. Reagent strips do have the advantage of avoiding false-positive reactions with organic iodides, such as those used for X-ray contrast and tolbutamides or other drugs [3].
Since a positive result for protein is significant, it must be confirmed by a second strip method after 24 hrs and also by another method (acid precipitation method). Functional proteinuria which is common is usually less than 0.5 gm/day, and can be seen in various situations in which dehydration contributes to the level of protein measured in urine. With strenuous exercise and fever, a mixture of high-and low- molecular weight proteins appear in the urine, and many casts, both hyaline and granular, can be seen [5]. Therefore it is important that the aviator who is being assessed should be advised not to do any flying, severe exercise and should not be dehydrated before the repeat test after 24 hrs. In our study 10 out of 102 cases having trace/1+ protein initially, disappeared after 24 hrs by following this regime.
The blood urea and creatinine should be asked for to rule out any long standing chronic renal disease. Examination of urinary sediments and culture rules out the commonest cause of transient proteinuria i.e. urinary tract infection. In our study 74 out of 102 proteinurias were due to urinary tract infection. Hence it is imperative that a urine microscopic examination must be conducted immediately after the proteinuria is detected. The aircrew can be started on the antibiotics as per the culture and sensitivity pattern. After the course of antibiotics urine for the protein must be tested again.
An ultrasonography seen of abdomen must be advise of for proteinuria to rules out renal calculi, certain renal parenchymal diseases and structural disorders of the urinary tract. In our study 7 out of 102 cases showed presence of calculi at different levels of the urinary tract. Two candidates, one with polycystic and other with solitary renal cyst were found out. Long standing diabetes mellitus affects the renal function almost a decade often the onsit of the disease. At the initial stages of the disease microalbuminuria sets in and subsequently frank proteinuria sets in. In our study 5 out of 102 aviators with proteinuria had uncontrolled diabetes.
Postural proteinuria (orthostatic) occurs in 3-5% of apparently healthy young adults. In this condition, proteinuria is found during the day but not at night when a recumbent position is assumed. Persistent proteinuria may develop in some of these healthy subjects at a later date, and renal biopsies have shown abnormalities of the glomerulus in a few cases. Proteinuria is apparently related to an exaggerated lordotic position and may result from renal congestion or ischemia [3]. The total daily excretion of protein rarely exceeds 1 g, and in most instances, no other evidence of renal disease develops. In our study there were 9 cases of orthostatic proteinurias amongst 4416 aviators who underwent medical examination at the institute (incidence 0.2%). The incidence is less than the general population incidence as recorded in the literature. This can be explained by the transient nature of this proteinuria and a small sample size.
Intermittent, transient proteinuria can occasionally be seen in humans with a normal history, physical examination, and otherwise normal renal function. Except for the occasional proteinuria, urinalysis is also normal. These candidates are typically followed every 6 months to check for hypertension or other abnormalities. There is another rare entity called overflow proteinuria. This is due to the overflow of excess levels of a protein in the circulation, and can be seen with hemoglobin, myoglobin, or immunoglobulin loss into the urine.
The patho-physiological mechanisms for proteinuria include glomerular damage (most common for proteinuria of > 2gm/day) and tubular damage or tubular overflow (where the tubules are unable to reabsorb an excessive filtered load of protein). These mechanisms can be active in many diverse, and sometimes rare, diagnoses. Searching for the specific diagnosis that is causing proteinuria can be time consuming, expensive, and require invasive tests (e.g., renal biopsy) along with the possibility of associated morbidity. A simpler and more convenient categorisation scheme (rather than specific diagnosis) separates proteinuria into two major classes: benign proteinuria (protein excretion of <1 gm/day and asymptomatic) and serious proteinuria (excretion> 1gm/day) based on the daily protein excretion rate and the presence or absence of symptoms is both easy and inexpensive and can be performed by most clinical aviation medical specialists at peripheral medical setups. The causes and an algorithm for proposed investigations has been elaborated at Fig 1. When the presence or absence of systemic disease is included this categorization scheme is also a good predictor of prognosis [6].
Proteinuria is usually asymptomatic, although aircrew may complain of some “frothiness” of their urine. Heavy and persistent proteinuria results in hypo-albuminaemia. This may produce, ankle swelling, abdominal pain and breathlessness. Patients with asymptomatic proteinuria usually have no signs; but in more severe cases, such as nephrotic syndrome, there may be oedema, ascites, hydrocoeles and pleural effusions as a result of decreased oncotic pressure.
In general, conditions which cause a high rate of proteinuria are more likely to a prognosis of renal failure with time. Additionally, the prognosis with systemic disease (especially diabetes or hypertension) or abnormal renal function is worse than if these conditions are absent. Prognosis is generally good for conditions causing benign proteinuria in the absence of systemic disease, and progression to advanced disease is rare over the next 20 years (a typical military career length) [7]. Of those conditions causing benign proteinuria, those that cause persistent (non-orthostatic) proteinuria carry a relatively poorer prognosis. Conversely, when systemic disease is present there is a higher risk for loss of kidney function and cardiovascular complications (myocardial infarction and cerebro-vascular accident) even with benign proteinuria. This can potentially shorten a full military aviation career, as these resultant conditions are incompatible with aviation duties.
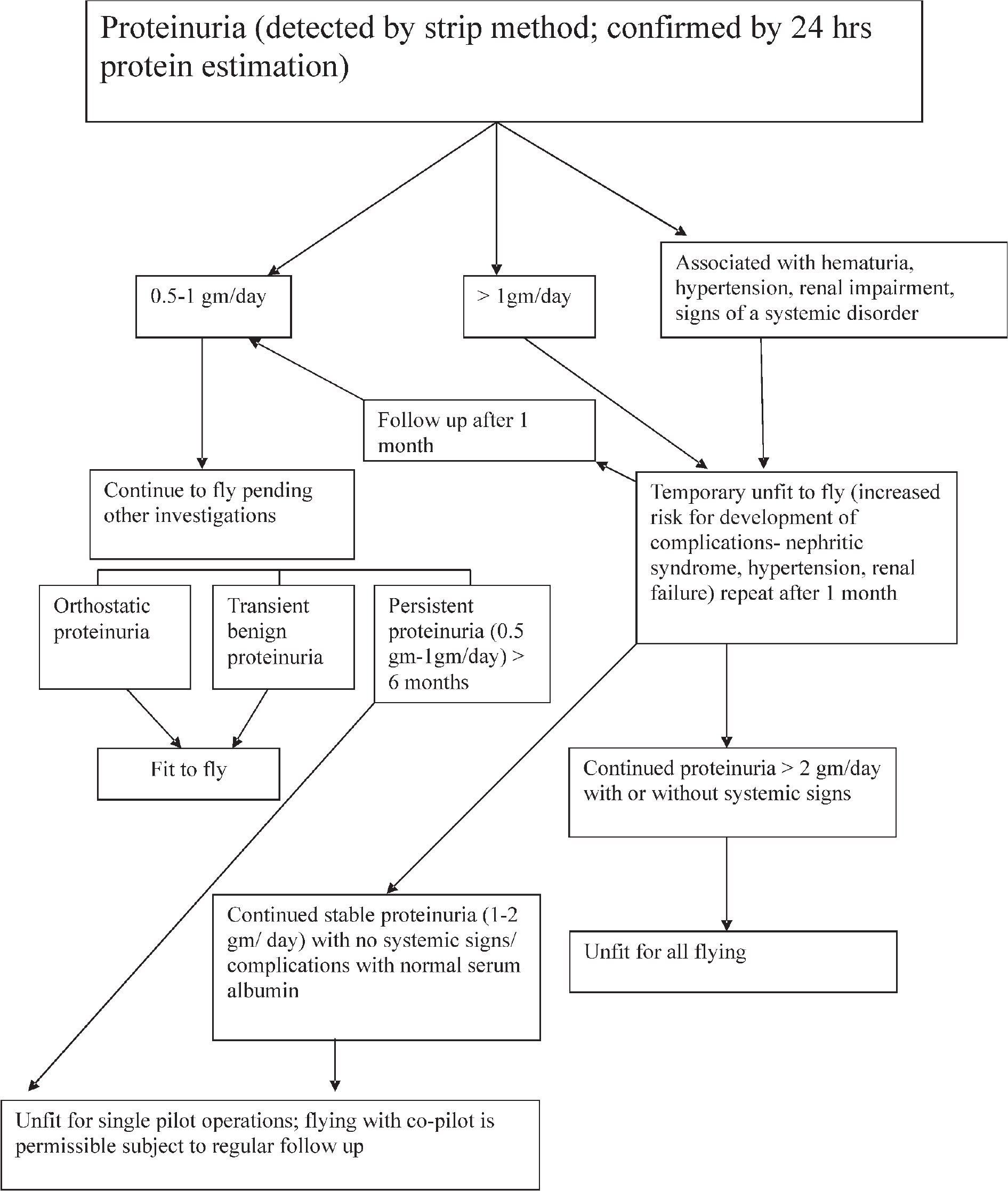
- Algorithm for aeromedical disposal of aircrew with proteinuria
Waiver Principles
The disqualifying defect must not pose a risk of sudden or latent incapacitation. Sudden/latent incapacitation (especially without symptoms) is unlikely for conditions that cause benign proteinuria. In this study all cases having <1gm/dl 24 hr protein were found fit to fly except those with renal/ureteric/ bladder calculi that can cause sudden spasmodic inflight pain. Incapacitation could occur in some conditions that cause serious proteinuria, but normally this happens only after obvious signs and symptoms are present. In our study one case of polycystic kidney was made unfit to fly as it is associated with types at other cysts in body, cerebral aneurysms and chronic renal diseases. In an experienced pilot with polycystic renal disease the waiver to fly can only be given when bleeding into tract, repeated urinary tract infection, calculi, hypertension and chronic renal failure have been ruled out.
The defect must have resolved or be stable at the time of waiver. Benign (non-persistent or orthostatic) proteinuria is normally stable. Benign persistent (non- orthostatic) or serious proteinuria is more likely to be progressive in nature. In our study four cases of nephrotic syndrome, as diagnosed by urinary proteins, serum cholesterol and protein levels, were lost to follow up. These were civil candidates who proceeded to civil hospitals for further investigations and treatment. The pilots who have chronic renal disease can only be made fit to fly as co-pilot in case their physical state is stable i.e.- absence of uncontrolled hypertension, chronic renal failure, stable renal functions with a creatinine clearance of >20ml/min, with no features of acidosis and anaemia [3].
The defect must not be exacerbated by military service or continued flying. There are no studies directly showing that continued flying exacerbates the underlying conditions that cause proteinuria. Some features of the aviation environment (e.g. hypoxia, acceleration forces) have, in some studies, been shown to cause transient proteinuria. The urinary protein excretion in climbers at high altitude was studied in 1970 [8]. This study investigated the relationship between protein excretion in high altitude climbers and 14 hrs after the exercise. Increasing protein excretion was found with increased altitude and was best correlated after a 1day lag (similar to acute mountain sickness symptoms). The association between altitude and protein excretion was attributed to hypoxic effects on the kidneys. A study in 1986 investigated the relationship between +Gz exposure and proteinuria. This study investigated the relationship between centrifuge exposure and urinary protein excretion [9]. Twenty subjects (fighter pilots) were selected, none with pre-existing proteinuria. +Gz acceleration varied from 3.5 to 5.5 G for about 15 min duration during each experiment. Seventeen of twenty subjects had detectable proteinuria following the centrifuge test. The resulting proteinuria was attributed to decreased renal blood flow during +Gz exposure. However an Indian study in 1995 done to analyse proteinuria post +Gz run showed 4 out of 17 subjects to have trace proteinuria [10]. To summarize these studies, conditions associated with the aviation environment may cause transient proteinuria with a physiological basis (transient renal hypoxia or ischemia). There is no evidence to suggest that repeated transient episodes of proteinuria from these causes cause any choric effects in those with normal renal function and without systemic disease.
Treatment is usually indicated for benign persistent proteinuria. Treatment may be limited to common medications (angiotensin enzyme inhibitors or angiotensin receptor blockers in cases of benign persistent (non-orthostatic) proteinuria or serious proteinuria. Monitoring progression of proteinuria is relatively simple and can be accomplished at peripheral Station Medicare Centres. Experienced pilots with acute glomerulonephritis are made unfit temporaily at the time of diagnosis. Aircrew who have spontaneous permanent remission can be made fit to fly as a co-pilot only with a monthly follow up inclusive of renal function tests [11].
Neither benign nor serious proteinuria is likely to impact mission accomplishment in the short term. Serious proteinuria may lead to eventual disqualification and removal from duties before a full military aviation career is completed. This justifies the rejection of proteinuric candidates for intake with systemic diseases and obvious signs and symptoms.
Disposition Policies Elsewhere
A review of other agency policies regarding proteinuria was conducted. The US Army policy maintains that proteinuria can be a sign of significant renal disease that may lead to chronic fatigue, near syncope, or unconsciousness. Mild proteinuria without underlying pathology is routinely recommended for waiver. If trace or 1+ protein is found repeatedly on urinanalysis; 24 h urine for total proteins under taken. For cases with more than 200 mg of protein/day, a nephrology or urology consultation is required. Waiver is usually based on the stability of disease and lack of significant symptoms. The policy guidelines suggests that the environment (heat, dehydration, prolonged duty) may exacerbate conditions that cause proteinuria [12].
The US Air Force policy (air force instruction) states that greater than 200mg/day of protein is disqualifying. Waivers are considered for fixed and reducible orthostatic proteinuria with a urinary creatinine ratio of <0.2. A nephrologist must conduct the evaluation for proteinuria [13].
Recommended Aeromedical Disposal
An algorithm for disposal of aircrew with protenein proposed at Fig 2. Available information from this retrospective study and the literature review, suggest that generally accepted evaluation protocal for waiver for cases with ad hoc proteinuria includes (a) Protein excretion rate less than 1 gm/ day (b) Normal renal function (c) Nephrologist consultation for assistance in diagnosis and estimation of prognosis after initial workup (d) Supporting laboratory and imaging studies including renal biopsy if indicated.
It is recommended that personnel with a protein excretion rate of greater than 2 gm/day should not normally be considered for a waiver due to the high likelihood of progression to renal failure. Periodic requirements for personnel to continue aviation duties with waiver would be 24 hr urine studies for total protein and creatinine clearance every 6 months until stable; annual review thereafter; and re-evaluation of waiver if protein excretion exceeds 1 gm/day, renal function declines, or related systemic disease becomes apparent.
Conclusion
A retrospective study for the incidence of proteinuria in Indian aviators was conducted. The incidence was similar to that of the general population. Generally accepted waiver principles were then examined to determine if waives can be proteinuria should be waived in aviation personnel. Other agency policies regarding proteinuria in aviation personnel were examined. Each case of isolated proteinuria should undergo a urine analysis after exercise free 24 hrs. Subsequent protein positive aviators have to undergo 24 hr urinary protein estimation and renal function test before a consultation to a nephrologist. The benign nonpersistent/ orthostatic proteinuria can be made fit to fly with regular follow up. Cases with serious proteinuria and with systemic involvement are made unfit to fly.
Conflict of interest: None
References
- The gauge for navy flight physical examination In: The ultimate flight surgeon reference Vol 58. (3rd ed). The U.S Naval, U.S. Army US. Air Force flight; 2001. p. :157-8.
- [Google Scholar]
- Basic Examination Of Urine In : Henry’s Clinical Diagnosis and management by laboratory methods (21st ed). Saunders; 2007. p. :393-425.
- [Google Scholar]
- Prevalence of proteinuria in rural adult population in Tamil Nadu. Ind J Med Res. 2006;124:185-8.
- [Google Scholar]
- Proteinuria: potential causes and approach to evaluation. Am J Med Sci. 2000;320(3):188-94.
- [Google Scholar]
- Proteinuria. Its clinical importance and role progressive renal disease. Am J Kidney Dis. 2000;35(4S):97-105.
- [Google Scholar]
- Proteinuria in fighter pilots after high +GZ exposure. Aviat Space Med. 1986;57:122-5.
- [Google Scholar]
- Urinary stress variables during exposure to high sustained +Gz. Indian J Aero Med. 1995;38(2):65-72.
- [Google Scholar]
- Clinical Aviation Medicine (3rd edition). Castle Connoly Graduate Medical Publishers; 2000. p. :43-44.
- [Google Scholar]
- U.S. Army aeromedical policy letters Condition: (ICD9 7910) U.S. Army Technical bulletin AR 40-501 40-8;15 Jan 1998. In: The ultimate flight surgeon reference (4th ed). Societies of the U.S. Naval U.S. Air Force Surgeons; 2001.
- [Google Scholar]
- U.S. Air Force Instruction 48-123 Medical examination standards, section A7.21.3. Washington DC: US January 200.152;
- [Google Scholar]






