Translate this page into:
Prevalence of liver abnormalities in healthy aircrew: A histopathological examination of autopsy samples and possible etiologies

*Corresponding author: Neha Gupta, Associate Professor (Pathology), Indian Air Force, Lucknow, Uttar Pradesh, India. nehagupta17sep@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta N, Santhosh SR. Prevalence of liver abnormalities in healthy aircrew: A histopathological examination of autopsy samples and possible etiologies. Indian J Aerosp Med 2024;68:61-6. doi: 10.25259/IJASM_1_2024
Abstract
Objectives
A substantial number of ostensibly healthy aircrew has incidentally shown liver abnormalities during routine medical assessments, posing challenges in their fitness evaluation. This study aimed to suggest the possible etiopathology behind such aberrations by integrating histopathological findings of liver samples and clinical data retrieved from the autopsy records of the same cohort of healthy aircrew.
Material and Methods
This retrospective cross-sectional study encompassed 22 years, studying the autopsy records of deceased aircrew following fatal aircraft accidents. The inclusion criteria comprised healthy aircrew between the ages of 20 and 55 years, who held a medical category of A1G1 or an equivalent rating. Alcohol intake, whether occasional or none was noted. Exclusion criteria covered aircrew with lower medical categorization or those with obesity (Body mass index [BMI] >30 kg/m2), pre-existing systemic diseases such as jaundice, cardiovascular disease, liver disease, diabetes mellitus, and chronic alcoholism. The archived microscopic slides of liver specimen were meticulously evaluated for histopathological abnormalities.
Results
Out of the 167 cases included in the study, macrovesicular steatosis was found in 23.8% individuals. The Chi-square test did not reveal a significant correlation between steatosis and alcohol intake (χ2 = 0.724, P = 0.39). The severity of macrovesicular steatosis was graded using the Non-Alcoholic Fatty Liver disease (NAFLD) activity scoring (NAS) system, with scores of 0, 1, 2, 3, and 4 found in 75.9%, 12.7%, 7.8%, 3.0%, and 0.6%, respectively. Both univariate and multivariate analysis was conducted using logistic regression to assess the correlation between age, BMI, and steatosis which yielded significant results. The odds ratios of age-adjusted for BMI and BMI adjusted for age for occurrence of steatosis were 1.11 and 1.57, respectively. Ordinal regression confirmed the association of age and BMI with increasing severity of steatosis, in agreement with the logistic regression results.
Conclusion
Macrovesicular steatosis accounted for 95.8% of histopathological abnormalities in the liver and was associated with increasing BMI an age, rather than alcohol intake. The severity of macrovesicular steatosis was limited to a maximum NAS score of 4, distinguishing it from non-alcoholic steatohepatitis (NASH), which requires a NAS score of ≥5. Thus, the macrovesicular steatosis was linked to uncomplicated NAFLD, in contrast to NASH, which is an irreversible condition and carries a graver prognosis. The most likely etiopathology underlying incidental and often transient liver abnormalities including elevated liver enzymes with or without hyperbilirubinemia and fatty liver detected during ultrasonography is NAFLD. The predominant finding of uncomplicated NAFLD, along with the absence of full-blown NASH and alcoholic liver disease, brings positive news since dietary and lifestyle modifications can potentially treat a majority of these cases.
Keywords
Aircrew fitness
Indian
Non-alcoholic fatty liver disease
Non-alcoholic steatohepatitis
Steatosis
Transaminitis
INTRODUCTION
Regular medical examinations have been crucial for ensuring the health and well-being of the aircrew. Interestingly, a noteworthy number of seemingly healthy aircrew undergoing routine medical assessments have been incidentally found to exhibit liver abnormalities, such as elevated liver enzymes with or without hyperbilirubinemia and fatty liver during ultrasonography.[1] This poses a challenge for physicians assessing their fitness for duty.[2,3]
In persistent cases where infectious causes and chronic alcoholism are ruled out, non-alcoholic steatohepatitis (NASH) is often presumed. However, diagnosing NASH relies on histopathological assessment, and liver biopsies are infrequently requested due to the mild and transient nature of the condition.
This raises the important question of whether the prevalence of mildly abnormal liver function tests and fatty liver in these individuals is sufficiently aligned with the histopathologically proven presence of steatohepatitis, thus enabling accurate attribution of the NASH diagnosis in the absence of a biopsy.
Autopsies present a valuable opportunity to gain insights into the prevalence of ongoing diseases within a population, particularly in cases where subtle derangements may not warrant a biopsy.[4,5] The previous studies conducted in India have revealed a 35.2% prevalence of steatohepatitis in forensic autopsies, primarily associated with death due to road traffic accidents, either with or without alcoholism (41.9%), and poisoning (24.8%).[6] Clearly, extrapolating such data to the healthy aircrew population would be inappropriate. Therefore, exploring the prevalence of hepatic histopathological abnormalities in autopsy samples obtained from the same cohort of healthy aircrew can provide valuable clues to the actual prevalence of these liver disorders.
In this study, we examine the histopathological findings in liver samples received during autopsies of healthy aircrew involved in fatal aircraft accidents and derive possible etiologies particularly focusing on the prevalence of NASH and associated lesions.
MATERIAL AND METHODS
This retrospective cross-sectional study was conducted at the Department of Aviation Pathology and Toxicology, where autopsy samples of deceased aircrew following fatal aircraft accidents are customarily investigated as part of the standard protocol in India. Liver specimens obtained during these autopsies were included for analysis, covering a study period of 22 years, from the year 2000 to 2021.
Clinical data pertaining to the aircrew was retrieved from the department’s records (Form – 1956). The inclusion criteria comprised liver samples from healthy aircrew individuals between the ages of 20 and 55, who held a medical category of A1G1 or an equivalent rating. Alcohol consumption history was meticulously sought from the Form 1956 which contains archival records completed by the Medical Officers at the time of the accident. Chronic alcoholism was an exclusion criterion. In this study, chronic alcoholism was effectively ruled out due to the rigorous protocols and continuous scrutiny implemented on the aircrew population, ensuring strict compliance and accountability in alcohol intake. Chronic alcoholics are not permitted to fly and, therefore, are not involved in aircraft accidents. However, occasional drinkers (consuming <20 g of alcohol per day)[7] or abstainers, as mentioned in the Form 1956, were included in the study.
The other exclusion criteria encompassed aircrew with lower medical categorization or those with obesity (Body mass index [BMI] >30 kg/m2), pre-existing systemic diseases such as jaundice, cardiovascular disease, liver disease, diabetes mellitus, hypertension, or those on regular medication.
The clinical data collection was followed by a meticulous evaluation of microscopic slides from the liver samples stained by hematoxylin and eosin (H&E) stain. Features such as hepatocytic lobular architecture, intracellular hepatocyte accumulations, intracellular inclusions, presence of granulomas, or necrosis were examined in detail. The portal triads were studied for mononuclear cell or plasma cell infiltration, interphase hepatitis, bile duct proliferation, and presence of overt fibrosis.
Macrovesicular steatosis was graded based on the non-alcoholic fatty liver disease (NAFLD) activity scoring (NAS) system [Table 1][8] and NASH was labeled for cases with NAS score ≥5. Autolysed samples and those displaying extensive coagulation necrosis due to burns associated with air crashes were excluded from the study to focus specifically on long standing antemortem abnormalities.
| Histological feature | Score | Category definition |
|---|---|---|
| Steatosis (%) | 0 | <5 |
| 1 | 5–33 | |
| 2 | 34–66 | |
| 3 | >66 | |
| Inflammation | 0 | None |
| 1 | 1–2 foci per×20 field | |
| 2 | 2–4 foci per×20 field | |
| 3 | >4 foci per×20 field | |
| Ballooning degeneration | 0 | None |
| 1 | Few | |
| 2 | Many |
A NAS score of 1–3 is labeled as NAFLD, 4 as indeterminate and ≥5 with hepatocyte ballooning is generally considered diagnostic of NASH. NASH: Non-alcoholic steatohepatitis, NAFLD: Non-alcoholic fatty liver disease, NAS: NAFLD activity scoring system
The data analysis was performed using the Statistical Packages for the Social Sciences (SPSS) software, (version 22.0 SPSS, Inc., Chicago, IL, USA). For quantitative data, the data were presented as mean ± standard deviation, and normality of data was assessed using the Kolmogorov–Smirnov test. Pearson’s correlation coefficient was used for normally distributed data, while Spearman’s correlation coefficient was employed for non-normally distributed data. Categorical variables were presented as numbers and percentages. Univariate analysis, using the χ2- test, was carried out to compare the significance of occasional alcohol intake in relation to liver pathology. Binary logistic regression was used to observe univariate associations of categorical and continuous predictors with the predominant pathological lesion. Only the independent variables with a significant association were included in the multivariate logistic regression analysis. P < 0.05 was considered significant in this study.
RESULTS
The study encompassed 176 cases where liver specimen was received for examination out of which 167 fulfilled the inclusion criteria. The demographic profile of the study population is given in Table 2.
| Parameter | Mean±SD | Total |
|---|---|---|
| Age (years) | 31.94±6.38 | 161 |
| Sex (%) | ||
| Males | 164 (98.2%) | 167 |
| Females | 3 (1.8%) | |
| BMI (Kg/m2) | 24.1±1.83 | 93 |
| Alcohol intake (%) | ||
| Occasional | 60 (70.6%) | 85 |
| Non-drinker | 25 (29.4%) | |
BMI: Body mass index, SD: Standard deviation
Liver pathologies observed are given in Figure 1. Macrovesicular steatosis was found in 23.8% individuals. The hepatocytic lobular architecture was preserved in all the cases with no instances of granulomas or necrosis. None of the cases showed interphase hepatitis, bile duct proliferation, and overt fibrosis.
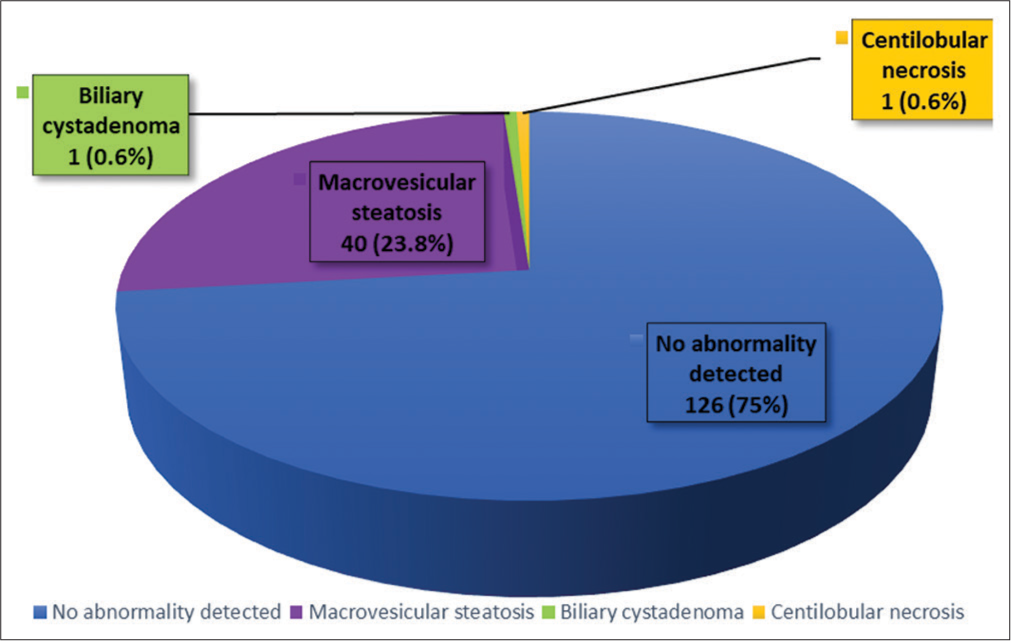
- Histopathological findings observed in liver samples.
Notably, macrovesicular steatosis constituted for 95.8% of the detected histopathological abnormalities while no instances of ballooning degeneration, Mallory–Denk bodies or obvious satellitosis of hepatocytes by neutrophils were observed. Mild mononuclear cell infiltration of portal triads along with macrovesicular steatosis was noted in 06 (3.6%) cases with no plasma cell infiltration or formation of lymphoid aggregates. In addition, no cases with a NAS score ≥5 amounting to NASH were identified. Figure 2 features photomicrographs illustrating different NAS scores found in this study. Moreover, the frequency of macrovesicular steatosis in all the 166 cases, stratified by increasing grades is shown in Figure 3, with a score of 0 indicating no steatosis.
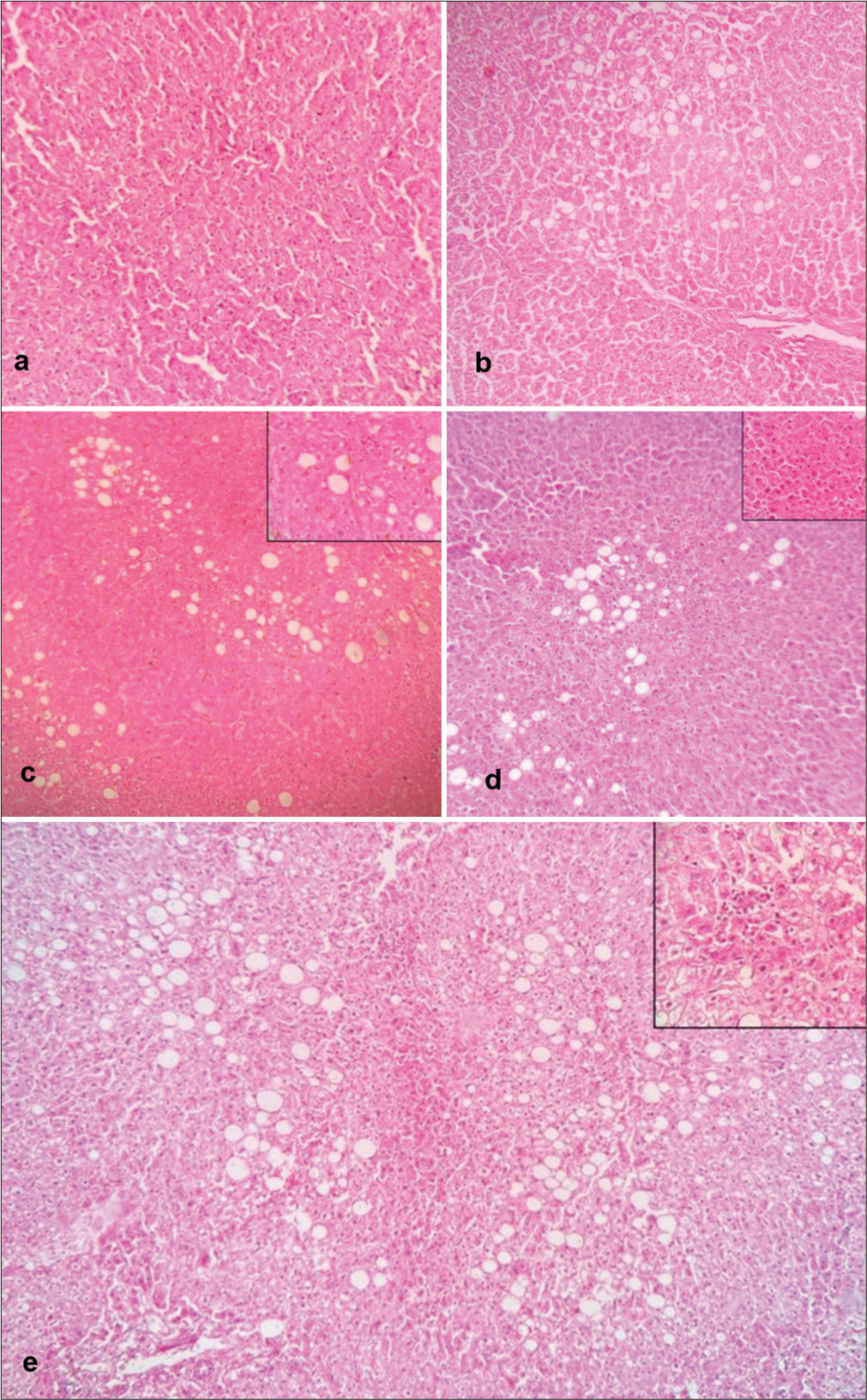
- Photomicrographs illustrating different non-alcoholic fatty liver disease activity scores (NAS) (Hematoxylin and Eosin stain, ×10). The inset images show inflammation (×40). (a) NAS-0 (<5% steatosis); (b) NAS – 1 (steatosis: 1, noinflammation); (c) NAS – 2 (steatosis 1, Inflammation: 1); (d) NAS – 3 (steatosis: 1, inflammation: 2) and (e) NAS – 4 (steatosis: 2, inflammation: 2).
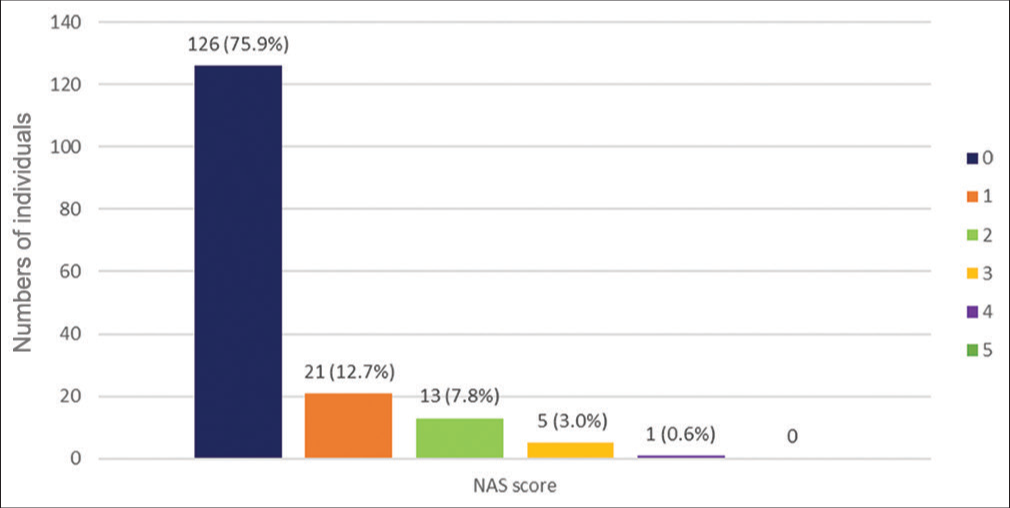
- Grading of macrosteatosis based on non alcoholic fatty liver disease activity scoring system (NAS).
The occurrence of macrosteatosis with age, alcohol intake, and BMI are depicted in the Figure 4a-c, respectively.
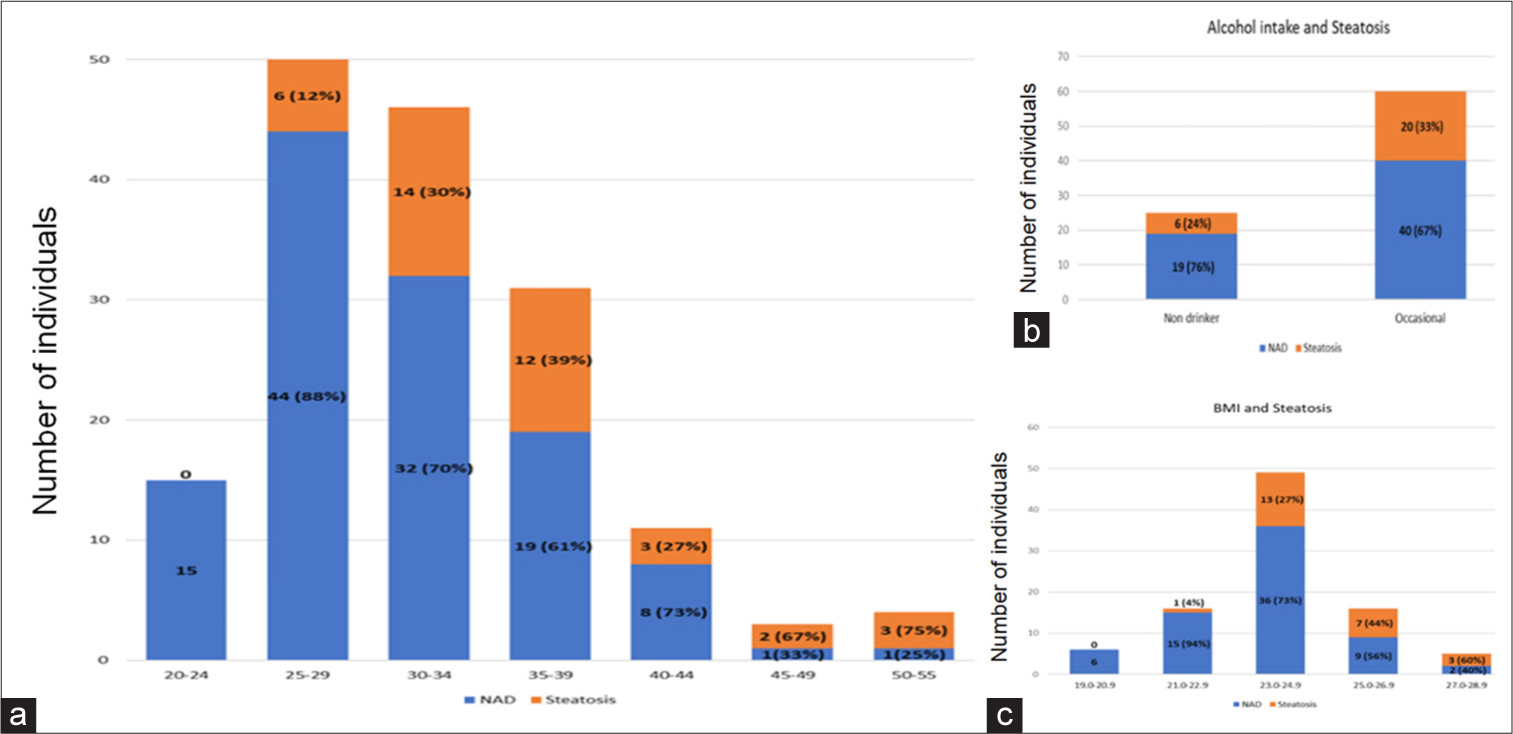
- Incidence of steatosis with respect to different variables. (a) Age, (b) alcohol intake and (c) body mass index.
A positive correlation was observed between age and BMI (r = 0.41, P < 0.05). The study further explored the relationship between steatosis and age, BMI, and alcohol intake. The Chi-square test did not show a significant correlation between steatosis and alcohol intake (χ2 = 0.724, P = 0.39). In addition, both univariate and multivariate analysis was conducted using logistic regression to assess the correlation between age, BMI, and steatosis. The results were significant in all the instances [Table 3]. The odds ratios of age adjusted for BMI and BMI adjusted for age for occurrence of steatosis were 1.11 and 1.57, respectively.
| Predictor | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P | Odds ratio | 95% CI | P | |
| Age | 1.132 | 1.064–1.205 | <0.05 | 1.117 | 1.013–1.232 | 0.026 |
| BMI | 1.786 | 1.277–2.499 | 0.001 | 1.570 | 1.102–2.236 | 0.012 |
Hoshmer–Lemeshaw test for goodness of fit P=0.229, CI: Confidence interval, BMI: Body mass index
To verify the consistency of the association of age and BMI with the increasing grades of steatosis, an ordinal regression was performed. The results from this analysis concurred with those obtained from logistic regression, as illustrated in Table 4.
| Predictor | Estimate | SE | P | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| Age | 0.109 | 0.044 | 0.12 | 1.115 | 1.018–1.221 |
| BMI | 0.353 | 0.163 | 0.03 | 1.424 | 1.033–1.962 |
Test for Parallel lines:P=0.997, Hoshmer–Lemeshaw test for goodness of fit P=0.936, SE: Standard error. CI: Confidence interval, BMI: Body mass index, NAS: NAFLD activity scoring
DISCUSSION
The primary aim of this study was to examine the histopathological findings in liver samples obtained during autopsies of healthy aircrew and elucidate the potential etiology. To achieve this, a multidisciplinary approach was employed, correlating liver histopathological findings with clinical data from autopsy records of deceased aircrew and then employing logistic regression to study correlation. What sets this study apart is its inclusion of a substantial amount of liver histopathological data from documented healthy adult Indians, a crucial aspect often absent in other forensic studies. Moreover, it overcomes the selection bias encountered in hospital-based liver biopsy studies, where these subtle derangements seldom warrant a biopsy.
The high incidence of alcohol consumption in unnatural deaths (up to 49.2%), including those resulting from road traffic accidents or poisoning, presents notable challenges in liver histopathological studies that rely on forensic autopsy samples.[6] This arises from the striking resemblance in histopathological findings between chronic alcoholism and NASH potentially complicating accurate diagnosis and interpretation of liver abnormalities in these studies.
The significant exclusion of chronic alcoholism enhances the study’s reliability in accurately discerning the etiopathology of liver abnormalities without the confounding influence of chronic alcoholism. However, it is essential to acknowledge that the target population included individuals who consumed alcohol occasionally. Therefore, alcohol intake was duly documented, and a correlation between alcohol consumption and histopathological findings was examined to comprehensively explore potential association.
The most common liver pathology encountered in these healthy adults was macrovesicular steatosis (23.8%). In a similar study done on the British aircrew, fatty liver disease was found in 15.6%.[9] Table 5 lists the common causes of macrovesicular steatosis.[10]
| 1. | Obesity |
| 2. | Diabetes mellitus |
| 3. | Protein-calorie malnutrition |
| 4. | Total parenteral nutrition |
| 5. | Drugs and toxins (e.g., Alcohol and corticosteroids) |
| 6. | Metabolic Disorders (e.g., Wilson’s disease) |
| 7. | Infections (e.g., Hepatitis C) |
The study meticulously ruled out probable causes through the use of exclusion criteria such as BMI for obesity, medical category for diabetes mellitus, and certain histopathological hallmarks such as presence of lymphoid aggregates for hepatitis C. No evidence of effect of occasional alcohol intake on liver histopathology such as Mallory–Denk bodies and neutrophilic satellitism was found. In addition, no significant correlation was found between alcohol intake and the occurrence of steatosis. Conversely, a notable and meaningful association emerged with age and BMI, reflected in adjusted odds ratios of 1.117 and 1.57, respectively. Evidently, BMI demonstrated a more pronounced impact than age on the occurrence of steatosis, exhibiting a trend of increased severity with higher BMI as indicated in Table 5. This observation suggests NAFLD as the more plausible etiology.
It is important to note that Southeast Asia faces a severe situation as far as disease burden of NAFLD is concerned.[11] While NAFLD is commonly associated with metabolic syndrome, obesity, and diabetes mellitus, it is crucial to highlight that the study population was characteristically healthy, with an average BMI of 24.1 ± 1.83 Kg/m2. Some specific genes, namely, PNPLA3, TM6SF2, and SERPINA1, have been linked to the incidence of NAFLD in non-obese individuals;[11,12] however, inadequate literature is available regarding the prevalence of these genes and their association with NAFLD in the Indian context.
Substantial research has established connections between NAFLD and various environmental factors, including a diet rich in saturated fats, trans fats, red meat, and sugar-sweetened beverages, as well as a lifestyle involving reduced physical activity.[13-16] These factors can induce oxidative stress in the liver environment.[17] Consequently, it is reasonable to consider that, in addition to the influence of increasing BMI, the progression in age associated with reduced physical activity and the accumulation of oxidative damage, potentially contribute to the heightened occurrence of NAFLD as age advances.
In addition, certain chemicals related to aviation, such as per- and polyfluoroalkyl substances used in firefighting foams and other aviation applications, have been associated with liver damage and a heightened risk of NAFLD.[18] However, the extent of their impact on aviators remains to be thoroughly investigated.
An endeavor was undertaken to assess the severity of NAFLD using the NAS score to determine the proportion of lesions corresponding to NASH. However, none of the lesions met the criteria for NASH, since none fulfilled a NAS score of ≥5, and no ballooning degeneration was observed. The mild mononuclear portal inflammation observed in a few cases was commensurate with NAFLD.[10] Fortunately, unlike NASH, NAFLD is reversible and improves through dietary and lifestyle modification.[14,19]
An association has been observed between the occurrence of elevated liver enzymes and more than 20% liver steatosis, even in the absence of features indicative of NASH.[20] In our study, we observed such lesions in NAS scores 3 and 4, accounting for 3.6% of the cases [as depicted in Figure 3]. In a separate study within the same cohort, elevated transaminase levels were detected in 0.59% of the population, and within this group, only 14.4% were identified to have fatty liver on ultrasonography.[1] This suggests that while a significant degree of steatosis may be present histologically, a smaller proportion of individuals are likely to exhibit abnormal liver enzyme levels and further lesser as fatty liver on ultrasonography.
This study faced a few limitations. First, its retrospective nature limited the amount of data obtainable from autopsy records. In addition, while the identified lesions were of milder nature and lacked fibrosis or ballooning degeneration (key features of NASH) on H&E stain, an assessment of fibrosis using special stains like Masson’s Trichrome stain was not performed. Finally, the findings were based on the observations of a single pathologist. Given the subjective nature of histopathological evaluations, interobserver bias could not be mitigated.
CONCLUSION
This study offers valuable insights into liver abnormalities among healthy aircrew. The predominant finding of un-complicated NAFLD, along with the absence of full-blown NASH and alcoholic liver disease, brings positive news. The fact that dietary and lifestyle modifications can potentially treat a majority of these cases is encouraging. By unraveling the intricacies behind these liver derangements, more robust evidence-based guidelines can be developed, leading to better overall wellness for this distinctive occupational group.
Ethical approval
Institutional Review Board approval is not required as it is a retrospective cross-sectional study.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Biochemical abnormalities in Indian aircrew. Int J Contemp Med Res. 2018;5:1-4.
- [CrossRef] [Google Scholar]
- Mild transaminitis in asymptomatic aircrew-a clinical dilemma. Ind J Aerospace Med. 2008;52:71-6.
- [Google Scholar]
- Unconjugated hyperbilirubinemia in commercial pilot: A clinical dilemma. Ind J Aerospace Med. 2009;53:53-7.
- [Google Scholar]
- Forensic pathology and epidemiology, public health and population-based research. Acad Forensic Pathol. 2011;1:282-7.
- [CrossRef] [Google Scholar]
- Autopsy proven pulmonary embolism in hospital patients: Are we detecting enough deep vein thrombosis? J R Soc Med. 1989;82:203-5.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592-609.
- [CrossRef] [PubMed] [Google Scholar]
- Design and validation of a histological scoring system for non-alcoholic fatty liver disease. Hepatology. 2005;41:1313-21.
- [CrossRef] [PubMed] [Google Scholar]
- Steatosis, steatohepatitis and related conditions In: Scheuer's liver biopsy interpretation (10th ed). New York: Elsevier Ltd; 2021. p. :108-35.
- [CrossRef] [Google Scholar]
- Changes in the global, regional, and national burdens of NAFLD from 1990 to 2019: A systematic analysis of the global burden of disease study 2019. Front Nutr. 2022;9:1047129.
- [CrossRef] [PubMed] [Google Scholar]
- Toward genetic prediction of nonalcoholic fatty liver disease trajectories: PNPLA3 and beyond. Gastroenterology. 2020;158:1865-80.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary habits, and their relations to insulin resistance and postprandial lipemia in non-alcoholic steatohepatitis. Hepatology. 2003;37:909-16.
- [CrossRef] [PubMed] [Google Scholar]
- Nutrition and physical activity in NAFLD: An overview of the epidemiological evidence. World J Gastroenterol. 2011;17:3377-89.
- [CrossRef] [PubMed] [Google Scholar]
- Sugar-sweetened beverages, low/no-calorie beverages, fruit juice and non-alcoholic fatty liver disease defined by fatty liver index: The SWEET project. Nutr Diabetes. 2023;13:6.
- [CrossRef] [PubMed] [Google Scholar]
- Food groups and the likelihood of non-alcoholic fatty liver disease: A systematic review and meta-analysis. Br J Nutr. 2020;124:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative stress in NAFLD: Role of nutrients and food contaminants. Biomolecules. 2020;10:1702-66.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding environmental contaminants' direct effects on non-alcoholic fatty liver disease progression. Curr Environ Health Rep. 2019;6:95-104.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of nutritional changes on nonalcoholic fatty liver disease. Nutrients. 2019;11:677.
- [CrossRef] [PubMed] [Google Scholar]
- Transaminase abnormalities and adaptations of the liver lobule manifest at specific cut-offs of steatosis. Sci Rep. 2017;7:40977.
- [CrossRef] [PubMed] [Google Scholar]







