Translate this page into:
Polymorphous light eruption in ground crew
Abstract
Polymorphous light eruption (PMLE) is a common, acquired, idiopathic photodermatosis characterized by recurrent, abnormal and delayed reactions to sunlight It presents clinically as itchy erythematous papules, papulovesicles and plaques on sunlight-exposed surfaces, its prevalence in general population ranges from 5-20 %. Technical ground crew of the Indian Air Force work for long hours or the tarmac under hot sun throughout the year and are exposed to ultraviolet radiation, therefore are at increased risk of developing PMLE. During the year 2001 to 2C02, PMLE was diagnosed in 19 technics ground crew from various Air Force units in Bangalore. Only four airmen were from non technical trades. Lesions were predominantly papules, plaques and vesicles and resolved in an average of 4.58 days after therapy with topical corticosteoids. Recurrence rate was high, mainly because patients did not follow long term sum protection measures. Simple measures like wearing overalls with rolled down sleeves and turning up of the collar to cover the nape of neck and liberal use of opaque sun screens can shield the skin from sunlight and can help to prevent PMLE.
Keywords
Polymoi phous light eruption
photosensitivity
ground crew
Polymorphous light eruption (PMLE) is a common, acquired, idiopathic photodermatosis seen in dermatology clinics worldwide and is commonly known as “sun rash”. Its prevalence in general population varies from 10-20% in various populations and is more common in women than men. PMLE is often seen in ground crew due to prolonged occupational exposure to sunlight. As the name implies, the skin lesions consist of erythematous papules, plaques, papulovesicles and erythema multiforme like lesions which are pruritic in nature and involve sun exposed areas. The condition can be easily diagnosed and treated. The incidence, prevalence and response to therapy of this condition in technical ground crew posted at various Air Force units in Bangalore have been presented here.
Material and Methods
Ground crew who had presented with clinical features of PMLE to the dermatology outpatient department of Command Hospital Air Force Bangalore in the years 2001 and 2002 formed the subjects for the study. A detailed history was obtained about the time of sun exposure, duration and the relation to their skin rashes, with special relevance to the occupational exposure was recorded. Skin biopsy was done for histopathological confirmation as and when required. All were advised to use topical clobetasol propionate 0.05% at night time and were advised sun protection during day time. Sun screens were advised to be applied liberally at least thrice between 8AM to 4PM in some patients. In addition, prophylactic measures were explained in detail. The time taken for regression of lesions was noted. Patients were followed up and those who developed repeated recurrences were tested for Anti Nuclear Antibodies to exclude Systemic Lupus Erythematosus. Those on oral drugs for concommitant illnesses were excluded from the study.
Results
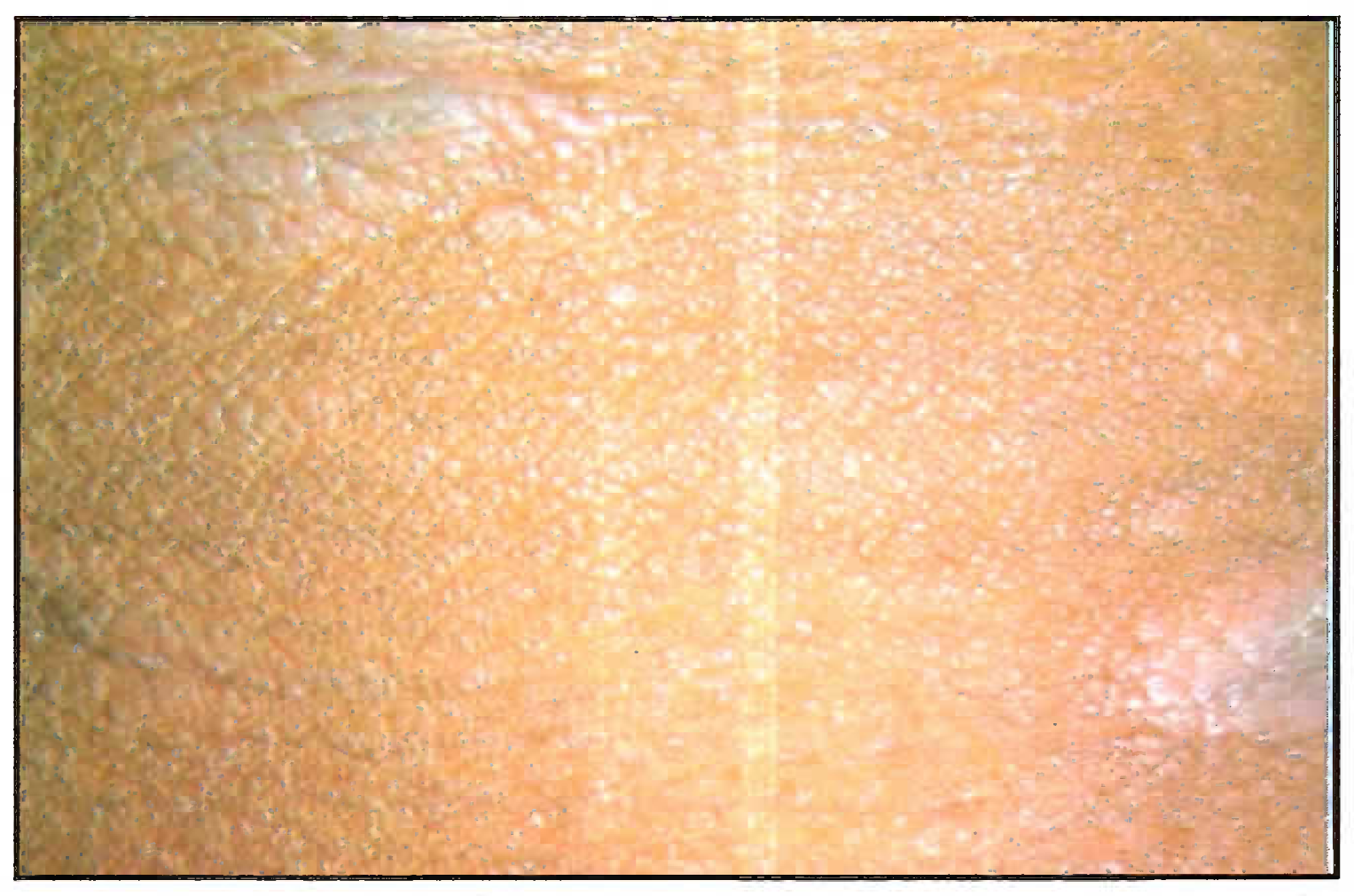
There were 19 technical ground crew from different Air Force units in Bangalore who were diagnosed with PMLE at Command Hospital Air Force Bangalore in the years 2001-2002. These personnel were from technical trades such as Engine, Instrument, Radio and Radar Fitter etc. There were four airmen from non-technical trades. The mean age of these indiviudals was 28 years (range 21-50 years). Symptoms developed within an average of 40 minutes of sun exposure (range 10 min to 6 hrs). Average duration of occupational sun exposure in these personnel was 3 to 4 hrs per day between 8 AM and 4 PM. Duration of symptoms prior to diagnosis ranged from 1 to 7 years. Seventeen (89%) out of 19 patients had their onset of symptoms in the months of February and March. Four (21%) patients had stated that their lesions persisted throughout the year. Lesions were predominantly papules, followed by plaques and vesicles (Figs 1 & 2). They were distributed mostly on the forearms, neck and face. Biopsy was done in seven (36%) cases. In all cases histopathology revealed a lymphocytic perivascular infiltrate.
Pruritus resolved in 4.58 days (range of 2 to 8 days) after therapy with topical clobetasol propionate. Thirteen patients had residual hypo or hyper pigmentation at the end of three months of follow-up. Sixteen (84%) cases responded well to therapy with complete resolution of all lesions, but three (15%) cases needed topical corticosteroids for longer than 30 days in a year. Lesions recurred in 14 (73.6%) patients in the next 1 to 12 months, mainly because patients did not follow correct sun protection measues. On follow up for one year, symptoms resolved without recurrence in five (26.4%) patients. None of the cases had tested positive for ANA at the end of one year follow-up.
Discussion
PMLE was found to have a prevalence of 10% in a survey of 271 apparently healthy people in Boston [1], in 21% of 397 people in Sweden [2] and 5% of 172 people in Perth, Austrialia [3]. The lesions may be recurrent and persist for many years [4], Individual lesions may be interspersed with normal skin but at times coalesce to form plaques [5]. In our study, the prevalence of PMLE was about 7% of all outpatient cases seen during the period. The age of onset is usually in the second and third decades and majority of our patients had their first episode in the third decade. Most patients give history of short burst of intense sun exposure precipitating their symptoms which was also the case in our study.
PMLE is the commonest idiopathic photosensitivity disorder in India. As the name implies, the lesions associated with PMLE vary widely in appearance. The rash which is itchy may consist of erythematous papules, papulo-vesicles, plaques and erythema multiforme like lesions in the sun exposed areas. The most commonly affected sites are nape of the neck, extensor aspects of forearms and face. It is more common in women than men. In general, one type of lesion predominates in a given individual. The diagnosis of PMLE is usually based on the clinical picture. Normal titres of ANA, as well as normal urine, stool and blood porphyrin levels support the diagnosis. Lesions generally appear in spring and summer and after sun exposure. They may persist for several days but eventually resolve without scarring. Symptoms are often mild and transient usually appearing in spring and summer, especially in high altitude locales. A “hardening effect” of skin takes place after prolonged exposure in the form of increased pigmentation, epidermal changes and immunological changes. This protects the skin from further lesions as summer progresses.

- Ill defined macule
- Scaly in aqiie ever the reck
Most authors consider PMLE as a delayed type of hypersensitivity to some unknown sunlight-induced antigen. Sunlight is definitely the precipitating factor, but the exact spectrum of wavelength that causes development of these lesions is not well known. Most patients are sensitive to UV-A (320 nm - 400 nm), but lesions can also be induced by UV-B (290 nm - 320 nm) alone. The natural history of the disease is highly variable, ranging from complete remission to development of debilitating symptoms and possibly other autoimmune disorders like lupus erythematosus. The susceptibility of monozygotic twins to develop PMLE is suggestive of a strong genetic aetiology.
The etiology of PMLE is not fully known, and it is likely to be multi-factorial. The immunologic pathogenesis of PMLE is supported by the study of timed biopsy samples of PMLE lesions. The CD4 subtype of T cells seen very early after exposure is replaced by CD8 lymphocytes 72 hours after irradiation. In general, findings conform to type IV delayed type hypersensitivity mechanism [6]. Immunofluorescence studies reveal extensive intravascular and focal perivascular deposits of fibrin, C3 and IgM, but the lupus band test is negative in all cases, suggesting that venular injury with activation of the clotting system may be involved in the development of lesions in PMLE [7] . In some PMLE lesions induced by UV-A, keratinocytes were found to express intercellular adhesion molecule 1 (ICAM-1). ICAM-1 is absent from normal keratinocytes, but it is known to be strongly induced by interferon gamma. The induction of ICAM-1 on keratinocytes results either from direct effects of UV on the promoter region of the ICAM-1 gene or from indirect effects of interferon gamma produced by activated lymphocytes aggregating in an underlying PMLE [8]. Though most authorities consider UV-A light as the causative factor in PMLE eruption, UV-B, or even visible light, may be responsible in some individuals. In one study, photo-provocation tests showed a pathologic reaction to both UV-A and UV-B in 88% of the men and 52% of the women [9].
Histopathology of PMLE lesions reveal a tight, perivascular lymphocytic infiltrate in the upper and mid dermis. Occasionally, neutrophils and eosinophils may be present in the infiltrate. All the seven cases in which biopsy was carried out showed perivascular lymphocytic infiltrate.
Technical ground crew of Indian Air Force can be exposed for prolonged periods to sun by virtue of their job. It is common to see such crew working on the tarmac under hot sun in flying units, often in overalls with their sleeves rolled up. This is to enable easy access to vital components of the aircraft and to prevent snagging of the overall in machinery. The duration of exposure depends on their work schedules and is often during the time of the day when ultraviolet radiation is at its highest. As a result their skin receives both UV-A and UV-B more than those tradesmen who work indoors most of the time. The prolonged periods of sun exposure in these ground crew appears to be the obvious precipitating cause for PMLE. The nape of the neck, extensor aspect of acral areas and forehead are the sites commonly involved. The onset of lesions in February and March is due to the inadequate hardening of the skin in winter compounded by clear skies during this time permitting high UV radiation to reach the ground. The incidence decreases in summer because of adaptive skin hardening.
Topical corticosteriods and advice on sun protection are the mainstay of therapy. In ground crew, precautionary measures include use of thick weave cotton clothing, rolled down sleeves, rolled up collar, wearing of a wide brimmed hat or a cap. Liberal use of an opaque sun screen such as zinc oxide cream on the uncovered areas such as face can reduce the incidence of PMLE. Early diagnosis and preventive health education can minimise the need of referral in most cases, thereby preventing loss of valuable man-hours. Squadron Medical officers should be able to easily recognise and treat most of the cases of PMLE. Intractable cases can be referred to the hospital for systemic therapy.
References
- Polymorphic light eruption: a common reaction uncommonly recognized. Acta Derm Venereol. 1982;62:237-40.
- [Google Scholar]
- Current aspects of polymorphous light eruptions in Sweden. Photodermatology 1986:298-302.
- [Google Scholar]
- Polymorphic light eruption: prevalence in Australia and England. BrJ Dermatol. 1994;130:62-4.
- [Google Scholar]
- Disease associations in polymorphous light eruption : A longterm follow-up study of 94 patients. Arch Dermatol. 1998;134:1081-5.
- [Google Scholar]
- Papulovesicular light eruption: a defined subset of polymorphous light eruption. Arch Dermatol. 1985;121:1286-8.
- [Google Scholar]
- Adhesion molecule expression in polymorphic light eruption. J Invest Dermatol. 1992;99:504-8.
- [Google Scholar]
- Papulai polymorphous light eruption: Fibrin, complement, and immunoglobulin deposition. Arch Dermatol. 1984;120:866-8.
- [Google Scholar]
- Expression of intercellular adhesion molecule-1 (ICAM-1) and OKM5 in UV-A and UV-B induced lesions in patients with lupus erythematosus and polymorphous light eruption. Arch Dermatol. 1993;285(6):328-33.
- [Google Scholar]
- Polymorphic light eruption: A clinical and photobiologic follow-up study of 110 patients. J Am Acad Dermatol. 2000;42:199-207.
- [Google Scholar]






