Translate this page into:
In-flight medical emergencies and their outcome in a commercial airliner

*Corresponding author: Umesh Kumar Kadubasavaiah Bhagavath, Department of Civil Aviation, Rusayl Health Centre, Muscat, Oman.umeshyash7@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Umesh KB, Shukaili WS. In-flight medical emergencies and their outcome in a commercial airliner. Indian J Aerosp Med 2022;66:79-83
Abstract
Introduction:
Super-connected modern era facilitated an unprecedented no. of air passages all around the world, simply because the number of people has doubled over the past 50 years culminating to around 4 billion air trips annually. An ever-increasing number of elderly passengers traveling with antecedent medical morbidities resulted in an upsurge in the In-flight Medical Emergencies (IME).
Objective:
Considering the trend, it was decided to ascertain the type of IMEs based on various organ systems and their outcome aside causes of flight diversion due to IME and types of in-flight medical assistance rendered by onboard physicians and paramedics.
Material and Method:
Crew safety report from March 1, 2015, to March 31, 2019, in a commercial airline of a Middle-Eastern country was analyzed for IMEs along with allied issues.
Results:
There were 614 IMEs during the period of study resulting in 01 IME for every 336 flights. About 81% of IMEs occurred during the main cruising phase of the flight. Nine onboard deaths were recorded during the study tenure. Causes of death were two each for Myocardial Infarction (MI) and malignancy, one due to cardiac failure with arrest and uncertain in four cases. The most common IME was syncope (35.5%) followed by trauma (26.8%) and respiratory difficulty (17.3%). Gastrointestinal symptoms accounted for 10% of cases. Diversion of aircraft was carried out on 16 IME incidents. The main causes of diversion were MI, epilepsy, stroke, and Bell’s palsy. Onboard assistance from physicians and nurses was sought in 62 % and 27% of incidents, respectively. Oxygen and onboard medications were used in 74% and 32% of cases correspondingly.
Conclusion:
There is no comprehensive globally accepted reporting and management of IMEs. Every airline has its own protocols for the same. Onboard healthcare professionals play a key role in the outcome of IMEs.
Keywords
In-flight medical emergencies
Commercial aviation
Medical diversion
INTRODUCTION
In the year 2019, nearly 4.3 billion passenger enplanements were reported by commercial airliners all over the world.[1] An increase in the passenger volume and a sustained growth of airline travelers recounted an increase in customers seeking in-flight medical assistance. Aged patrons traveling with disease and disabilities are also on the rise. There has been a 30% increase in people withdiseases or disabilities indulging in the voyage by commercial airliners.[2] With the increase in aged passengers traveling with morbidities, there has been a steady increase in In-flight Medical Emergencies (IMEs). There is no standard universally accepted reporting procedure for notification of IMEs specified by ICAO or other regulatory authority. Every airline has its own reporting procedure of the IMEs. Contemplating the upward trend of IMEs, it was decided to analyze details of IMEs, inter-alia allied factors, if any, reported by a national airline of Middle-east country in the recent past.
MATERIAL AND METHODS
A retrospective review of all records of crew safety report pertaining to IMEs by the captain of aircraft for all the flights from March 1, 2015, to March 31, 2019, of a national carrier of a Middle-eastern country was carried out. Reports contained event date and time, type of aircraft involved and detailed summary of the incidents including personal profile of affected passenger/crew member with nature of symptoms, Medical-Information-Forms (MedIF) of all eligible patients having medical history/treatments/miscellaneous medical information, type of assistance pursued from healthcare professionals with detail of assistance rendered beside management of the case. These findings were analyzed in customized Excel sheet. The report also included data in relation to onboard death, flight diversions with reason, and final outcome of diseased passenger.
RESULTS
A total of 614 IMEs were declared during 4 years. Airline flew a total of 2, 06, 321 flights during the same period. This amounts to one IME for every 336 flights. Total number of IME was 30.7/million passengers and 01 for every 1.46 billion passenger kilometers.
On analyzing the phase of occurrence of IMEs, it is seen that maximum number of IME occurred during the Cruise. It accounted for nearly 81% of all IMEs. This is represented in Figure 1.
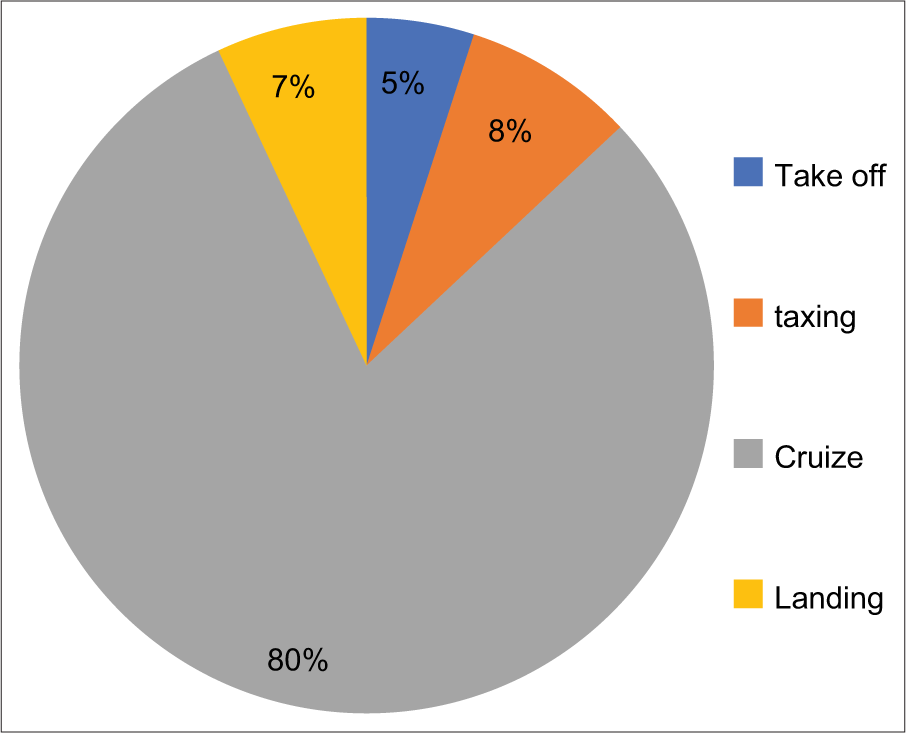
- Flight Phases for Occurrence of in-flight Medical Emergencies
Distribution of all IMEs is presented in Table 1 and Figure 2
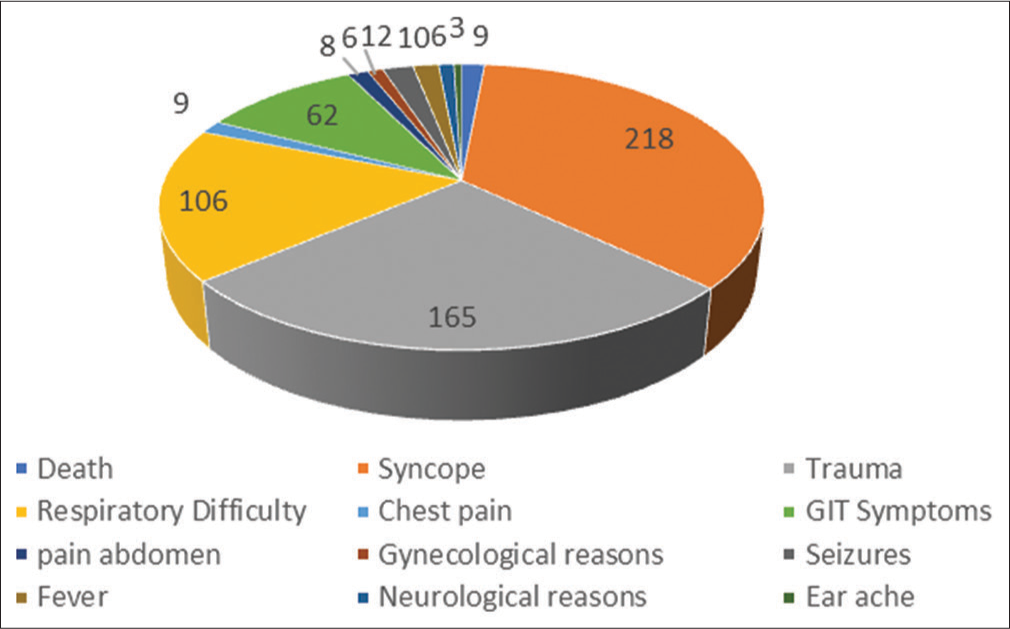
- Reasons for In-flight Emergencies.
| Reasons for IMEs | No. | Percent |
|---|---|---|
| Death | 09 | 1.47 |
| Syncope | 218 | 35.50 |
| Trauma | 165 | 26.87 |
| Respiratory difficulty | 106 | 17.26 |
| Chest pain | 09 | 1.47 |
| Gastrointestinal symptoms | 62 | 10.10 |
| Pain abdomen | 08 | 1.30 |
| Gynecological reasons | 06 | 0.97 |
| Seizures | 12 | 1.95 |
| Fever | 10 | 1.63 |
| Neurological reasons | 06 | 0.97 |
| Ear ache (Baro-trauma) | 03 | 0.49 |
IME: In-flight medical emergencies
In-flight death
There were nine deaths reported during the period of analysis. MedIF cases accounted for five subjects. There was no obvious illness before flight in four clients. Among the subjects declared as serious patients, one had advanced carcinoma of colon and another; a child had cardiac valvular anomalies and was on his way for definitive treatment. Clinical diagnosis of Myocardial Infarction (MI) was made on the basis of symptoms in two cases. Cardiopulmonary resuscitation was rendered in almost all cases. Onboard physician declared dead in six instances and three such were done by paramedics and nurses. Aircraft diverted to the nearest airbase in two cases and deceased passenger was off-loaded.
Causes of IME
Syncope was the most common; accounted for nearly 35.5% of all IMEs. Injuries were the next common cause of IMEs. It comprised of nearly 26.8% of IMEs. Causes of injuries are shown in the Figure 3. Third common cause of IMEs was respiratory difficulty that reckoned for 17.3% of IMEs.
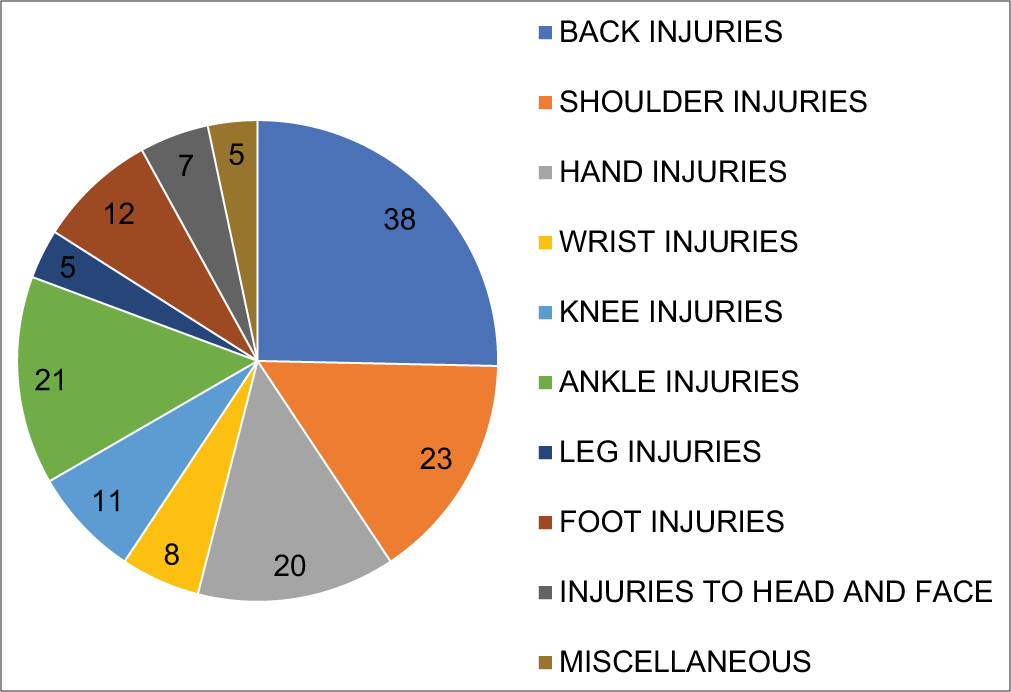
- Various types of injuries.
Syncope
Exact cause of syncope could not be established in many cases; however, two clients had high blood sugar. Oxygen inhalation with foot end elevation played a major role in syncope management by improving the venous return and enhancing oxygenation that helped brain to recover faster. Almost all responded to above-mentioned treatment except one MI patient presented as syncope and succumbed onboard.
Injuries
Injuries were mainly sustained by the cabin attendants compared to the passengers. The most common injury was lumbago/back injury followed by shoulder injury. Many had burn/scald following the spillage of hot liquid. Distribution of various injuries is depicted in Figure 3.
Other manifestations
Respiratory difficulty was the third common cause of IMEs and all of them were managed by oxygen administration at the rate of 4–6 L/min. Oxygen was delivered by face mask from the emergency oxygen cylinder. Bronchial asthma was diagnosed in seven cases and bronchodilator aerosols were used. There was no flight diversion because of respiratory symptoms.
Gastrointestinal symptoms consisted mainly of vomiting, diarrhea, and acidity. These were managed with oral medication. Parenteral fluid was administered by onboard physician in two clients.
Gynecological manifestations involved 0.9% of all the IMEs. It included mainly excessive vaginal bleeding; and abdominal pain in an expectant lady. These were managed onboard conservatively.
Pediatric casualties
There was a total of 21 pediatric emergencies. There were nine reported cases of epilepsy amongst children along with two epistaxis, four gastroenteritis, three burns, and three cardiac diseases out of which one child died onboard. Seizure and neurological symptoms accounted for maximum number of diversions. Main reason for diversion in seizures is non-availability of anti-epileptics onboard. Uncontrolled epilepsy prompted the physician to advice for flight diversion.
Diversion
Changing of landing destination is called diversion. Depending on the occurrence of emergency, diversion can cost anywhere between 30, 000 and 7, 25, 000 USD.[3]This also causes inconvenience to the fellow passengers by disruption of travel schedule. There were 16 diversions recorded during the period of study. Physician advice was sought in 12 cases and captain of the aircraft decided to divert on the basis of findings of the cabin crew and nurses in the remaining cases. Main reasons for diversion included MI – 03, uncontrolled seizures – 03, stroke – 02, and Bell’s palsy – 01. One of the MI patients with severe hypotension did not respond to routine conservative treatment and was therefore diverted. Uncontrolled epilepsy in a child prompted the pilot to take diversion. Regarding the first aid in epilepsy, no antiepileptic medications are kept in the First Aid Kit (FAK); it is the policy of health ministry of the country not to provide any sedative medication in FAK or Emergency Kit. This reportedly posed significant difficulty in management of epilepsy cases onboard in national carrier airlines. Airliner policy directs that all MedIF cases need to take antiepileptic medication before boarding and commencing of the voyage.
Onboard assistance from medical personnel
Onboard physician help as a good Samaritan was noted in 62% of cases. Nurses help was sought in 27% of cases and paramedics/dental doctor helped in 11% cases. Oxygen was used in 74% of IMEs. In-flight medication and intravenous administrations were used in 32% of cases. Vital parameters measured in 68% of cases and Glucometer was used in 8% of cases. Onboard diagnosis of cases without appropriate clinical history is really a challenging task for the onboard physicians. Reportedly constraints of space, unfamiliar environment with possible air-turbulence hampered the quality of management of in-flight emergencies. Some physicians had problem in interpreting blood sugar from mg to mmoL. Almost all the physicians had valid medical license card and they were not under the influence of alcohol at the time of rendering service.
DISCUSSION
IMEs are on the rise and will continue to surge as the number of aged passengers with preexisting diseases traveling long distances is also increasing.
A total of 614 IMEs were declared for 4 years in the present work. This amounts to 01 IME for every 336 flights. When compared with the results documented by the studies of the recent past where in the IMEs delineated to be one per every 604 flights; the present study unveiled a higher occurrence of IMEs as recorded by the National Carrier.[4] There is also a possibility of subjectivity in recording the IMEs. One of the reasons for higher incidence could be the air traveling of MedIF passengers. National Carrier renders voyages to MedIF cases in much higher number as compared to other airlines. A total of nine onboard deaths were reported during the same period making it one onboard death for every 22, 924 flights. Total number of IME was 30.7/million passengers and 01 IME for every 1.46 billion passenger kilometers. The incidence of IME in the present intent is similar to the findings as reported and documented by Los Angeles International Airport indicating 01 IME/29.8/million passengers.[5]
On analyzing the causes for aggravation of preexisting illness, the latter found to have been increased by many folds in a long-haul commercial flight. Reduction of oxygen saturation from 97% to 93% in-flight may not affect normal individuals but passengers who are already compensated by chronic morbidity will exhibit symptoms of decreased oxygenation. Prolonged upright sitting, poor venous drainage from lower torso and hypoxia trigger poor vital organ perfusion, systemic inflammation, and platelet activation. This leads to venous embolism in old passengers. Engine bled air from outside environment is dehumidified before releasing to the cabin. Decreased humidity in the air will also lead to dehydration. These triggering factors make the preexisting diseases manifest by exaggeration of symptoms.
Syncope accounted for nearly 35.5% of all IMEs and stood out as the most predominant ailment. Syncope can be central or peripheral. Central syncope is triggered by pain and anxiety whereas peripheral syncope is triggered by sitting in upright position combined with dehydration.[6] Common mode of approach to all cases of syncope has been foot end elevation, oral glucose administration, and oxygen inhalation. Commercial aircrafts carry oxygen that is intended for short-term use in case of loss of cabin pressurization. Oxygen is delivered at 2–4 L/min which is enough at cruising altitudes. Cases requiring more oxygen such as MedIF cases additional oxygen cylinders are carried by the carrier for the specific condition as requested by physician.
Injuries are the next common medical conditions contributed to 26.8% of IMEs. Injuries included traumatic lumbago, shoulder injuries, and burns/scalds. Most of in-flight injuries occurred among the flight attendants (91%) compared to the passengers. Our observations are similar to the observation by Logie et al.[7] There was no flight diversion or any delay due to injuries. FAK was enough to manage the injuries onboard. Two cases of fracture were reported among flight attendants.
Respiratory difficulty (17.3%) was observed the next frequent affliction onboard and was managed conservatively. Cardiac defibrillators are mandatory requirement in case of FAA certified aircrafts of more than 7500 Lbs.[8] It is a pre-requisite feature in all airlines flying in USA;[9] however, same is not applicable in EASA guidelines. Current national carrier follows the EASA guidelines; hence, Automated-External-Cardiac-Defibrillators (AECDs) are carried only in certain wide bodied aircrafts
Pediatric emergencies and their management onboard
While epilepsy recounted for maximum no. Cases of among children; in contrast, infectious diseases accounted for the most in US Airline.[10] However, the observed data appear to be insufficient to make any comparison. Uncontrolled epilepsy called for diversion in one case. Pediatric management of epilepsy was difficult as barbiturate suppositories were not a part of emergency kit. Establishing the lifeline onboard was also a herculean task in case of gastroenteritis.
In-flight death
A total of nine onboard deaths were reported during the same period making it one onboard death for every 22, 924 flights and 0.4 deaths/million passengers. Death rate is slightly higher than the global average of 0.31/million passengers.[11] In-flight deaths are more in those carriers that carry more Medif cases and have a greater number of long-haul flights. Careful preflight screening of Medif cases with availability of advanced medical kit and specialized training of flight attendants may help reduce the onboard deaths.
Prevention of IMEs
This must start from the booking stage itself. A detailed medical history will enable the airline physician to predict the possible emergencies onboard. Aviation Physician must apply his theoretical knowledge, clinical acumen, and proficiency in clearing the borderline MedIF cases likely to become critical onboard. Comprehensive training of cabin attendants in handling acute medical emergencies will pay rich dividends and prevent loss and inconvenience due to diversion. AECDs and its application training of the cabin attendants will greatly enhance the chance of survival of onboard cardiac emergencies. FAKs must be regularly updated considering the previous emergencies so that the management of cases will be better by Medical professionals.
This is a limited study based on review of data from records of IMEs documented by the national carrier airliners of a Middle-Eastern country. Therefore, the result may not stand applicable universally. However, the data generated opens up avenues for discussion especially on ways to prevent in-flight mortality and thereby its consequent fall-outs. Similar studies are recommended to unfold data on IMEs for other airliners.
CONCLUSION
Presently, there is no comprehensive globally accepted reporting and management guidelines for In-flight Medical Emergencies (IMEs). Every airline has developed and instituted their own protocols for dealing with the in-flight medical emergencies. While onboard healthcare professionals play a key role in the eventual outcome of IMEs, there is a need for more information on as to how internationally, the airlines deal with medical emergencies on board.
Declaration of patient consent
Patient’s consent not required as patient identities are not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Global Air Traffic-Passengers Scheduled Passengers 2004-2021. Available from: https://www.statista.com,statistics [Last accessed on 2020 Sep 20]
- [Google Scholar]
- Medical Tourism. :1-2. Available from: https://www.medicaltourismassociation.com/en/medical-tourism [Last accessed on 2020 Sep 20]
- [Google Scholar]
- Outcomes of medical emergencies on commercial airline flights. N Engl J Med. 2013;368:2075-83.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of in-flight medical emergencies on commercial airlines. Ann Emerg Med. 1989;18:26-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pacing for vasovagal syncope. Arrythm Electrophysiol Rev. 2018;7:95-102.
- [CrossRef] [PubMed] [Google Scholar]
- Musculoskeletal injury prevention project: Report on the flight attendant group. AirBC. 1997;3:1-82.
- [Google Scholar]
- In-flight medical events and aircraft diversions: One airline's experience. Aviat Space Environ Med. 2003;74:62-8.
- [Google Scholar]
- Emergency Medical Equipment 66 Federal Register 19028. 2001. Washington: Federal Aviation Administration; Available from: https://www.federalregister.gov/documents/2001/04/12/01-8932/emergency-medical-equipment [Last accessed on 2020 Sep 20]
- [Google Scholar]
- Pediatric emergencies on a US-based commercial airline. Pediatr Emerg Care. 2005;21:725-9.
- [CrossRef] [PubMed] [Google Scholar]
- In-flight deaths during the commercial travel. How big is the problem? JAMA. 1988;259:1983-8.
- [CrossRef] [PubMed] [Google Scholar]






