Translate this page into:
Hyperbaric Oxygen Therapy - IAM Experience A Review of Past Forty Years Cases
Abstract
This a retrospective study specifically aimed to cover the complete gambit of illness/ indications for which Hyperbaric Oxygen Therapy (HBOT) was given at this Institute. The data collected was also analyzed on various criteria to get trends of clientele at IAM. HBOT is a form of treatment in which a patient breathes 100% oxygen greater than 1 Atmosphere Absolute Pressure (ATA). Over the past 40 years (Jan 1973 – Jun 2013), hyperbaric oxygen therapy has been used in a wide variety of medical conditions. The analysis of data brings out some interesting trends. The data held at Dept of High Altitude Physiology and Hyperbaric Medicine (HAP&HM), was compiled and observed that 1540 cases were treated with HBOT, with an average of 37 cases being treated every year. Based on the data obtained at the beginning of the treatment, the cases were classified into various groups based on diagnosis like Non-healing ulcers, SNHL, Vascular, Post radiation, CVA, Dental etc. The data was also classified based on the client population. There was a varied type of clientele comprising mainly of civilians. Serving personnel, retired personnel and their dependents were also treated. Out of 1540 cases treated at this Institute, 889 (63.45%) improved, 444 (31.69%) could not be followed up. For 40 (2.85%) patients HBOT was interrupted due to reasons like discontinuation as advised by treating physicians, development of symptoms in chamber etc and only 5 (0.35%) did not show any signs of consisted improvement. The majority of the cases treated of 362 (25.83%) cases of Non Healing Wounds 258 (18.41%) cases of vascular disorder, 155 (11.06%) cases of SNHLand 118 (8.42%).
IAM experience over a span of four decade indicates that addition of HBO therapy to conventional treatment modalities significantly improves the outcome of various indicated diseases, especially non healing wounds, SNHL and Post radiation injuries.
Keywords
Hyperbaric Oxygen Therapy (HBOT)
Non healing wounds
SNHL
Post radiation injury
Introduction
Hyperbaric Medicine is use of increased barometric pressure for delivering increased oxygen dissolved in plasma to body tissues. HBOT is a form of treatment in which a patient breathes 100% oxygen at higher than normal atmospheric pressure that is greater than 1 atmosphere absolute (ATA). Therapy is given in special therapeutic chambers, which were earlier used primarily to treat illnesses of deep sea divers. Over the last five decades, animal studies, clinical trials and well-validated clinical experience has proved usefulness of HBO in several indications and there is recently a transformed concern in this field all over the world.
Acute traumatic wounds, crush injuries, gas gangrene are indications where addition of hyperbaric oxygen may be life and limb saving. Patients who have been suffering from non healing ulcers and all late consequence of radiation therapy show dramatic benefits with HBOT. Acute hearing loss and many neurological illnesses are now almost certainly known to benefit from HBOT. With ongoing growth all over the world, Hyperbaric Medicine has found a distinct role in the contemporary era of evidence-based medicine.
In major conditions, as with heart attacks or strokes, the amount of oxygen being carried by the blood may be normal but the tissues of the heart or brain are dying of hypoxia - lack of oxygen. A controlled trial in California has shown that when the latest clot busting drugs are given together with hyperbaric oxygenation, the benefit is dramatic [1].
This is a retrospective study specifically aimed to cover the complete gambit of illness/indications for which HBO therapy was given at this centre (Dept of HAP & HM).
Method
The patients included in this study have received routine HBOT in hyperbaric chamber at IAM over last 40 years. Total number of cases studied was 1540. The data was obtained from the medical record books maintained at the Department of High Altitude Physiology and Hyperbaric Medicine (HAP&HM). Based on the data obtained at the beginning of the treatment, the cases were classified in to various groups like Non-healing ulcers, SNHL, Vascular, Post radiation, CVA, Dental etc. The data was also classified based on the clientele population, their outcome, yearly trends etc. There was a varied type of clientele comprising of civilians, serving, retired personnel and their dependents. The data was analyzed for different parameters.
Results
The data of the treated cases were analyzed on various grounds like category, diagnosis, referral, outcome, yearly trends. The classification of cases as per diagnosis is given Table-1 and Figure1. The male to female ratio is given inTable-2.
| SSl No | Diagnosis | Cases | % age |
|---|---|---|---|
| 1 | Non Healing Wounds | 362 | 23.51 |
| 2 | No Diagnosis | 258 | 16.75 |
| 3 | Vascular | 258 | 16.75 |
| 4 | SNHL | 155 | 10.06 |
| 5 | Post Radiation | 118 | 7.66 |
| 6 | CVA | 66 | 4.29 |
| 7 | Osteomyelitis | 57 | 3.70 |
| 8 | Cold Injuries | 47 | 3.05 |
| 9 | Infective | 44 | 2.86 |
| 10 | Miscellaneous | 43 | 2.79 |
| 11 | Multiple Sclerosis | 24 | 1.56 |
| 12 | Fractures | 34 | 2.21 |
| 13 | Fascitis | 4 | 0.26 |
| 14 | Dental | 43 | 2.79 |
| 15 | Research Runs | 14 | 0.91 |
| 16 | IHD | 13 | 0.84 |
| Total | 1540 | 100.00 |

- Classification of cases as per Diagnosis
| Gender | Number | Percentage |
|---|---|---|
| Females | 290 | 18.8 |
| Males | 1250 | 81.2 |
| 1540 | 100 |
Majority of the patients treated for HBOT were civilians (52.34%). It is interesting to note the number of personnel treated and the category which they belong with age. Table to denote the percentage of personnel treated as per category is shown in Table-3. The outcome as per category is shown in Table-4 and Figure 3.
| Sl No | Category | Cases | % age |
|---|---|---|---|
| 1 | Serving | 531 | 34.48 |
| 2 | Dependent | 120 | 7.79 |
| 3 | Retired | 83 | 5.39 |
| 4 | Civilian | 806 | 52.34 |
| Total | 1540 | 100.00 |
| Sl no | Outcome | No | Percentage |
|---|---|---|---|
| 1 | Improved | 889 | 57.73 |
| 2 | Not improved | 5 | 0.32 |
| 3 | No follow up | 583 | 37.86 |
| 4 | Died | 3 | 0.19 |
| 5 | Interrupted | 40 | 2.60 |
| 6 | Research Run | 20 | 1.30 |
| Total | 1540 | 100.00 |
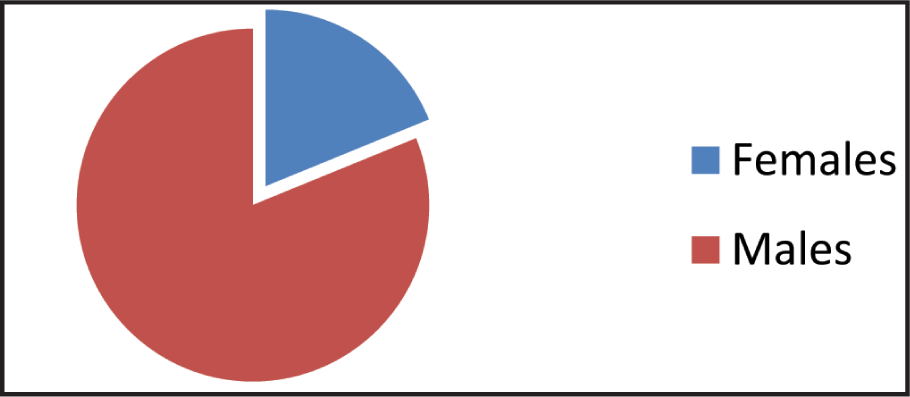
- Male to female ratio
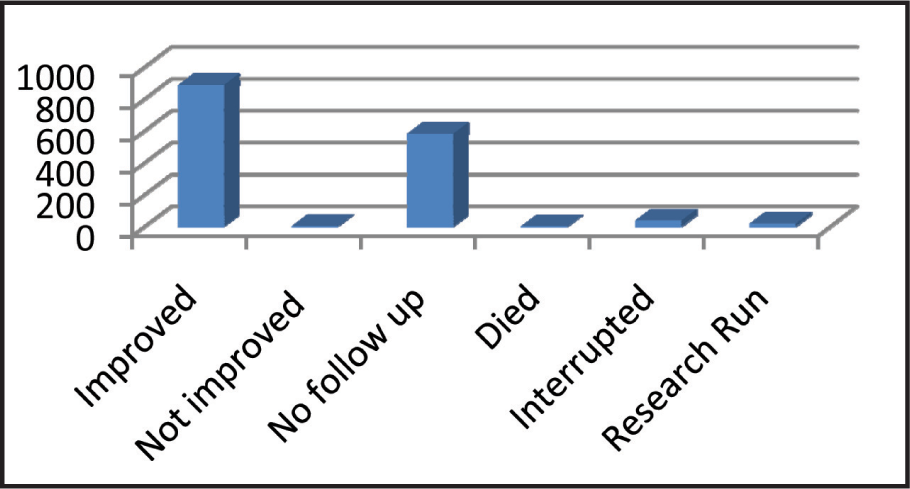
- - Distribution as per outcome
Classification as per years versus referal centres is given in Table 5. The trend of cases based on civil or service personnel depending on the centre from which they are referred when plotted year wise showed the trend depicted in Figure 5.
| Year | Service | Non- Service | Total |
|---|---|---|---|
| 1973 | 47 | 0 | 47 |
| 1974 | 6 | 0 | 6 |
| 1975 | 21 | 0 | 21 |
| 1976 | 20 | 3 | 23 |
| 1977 | 21 | 2 | 23 |
| 1978 | 5 | 1 | 6 |
| 1979 | 46 | 4 | 50 |
| 1980 | 16 | 3 | 19 |
| 1981 | 10 | 8 | 18 |
| 1982 | 18 | 2 | 20 |
| 1983 | 16 | 8 | 24 |
| 1984 | 5 | 8 | 13 |
| 1985 | 20 | 25 | 45 |
| 1986 | 33 | 19 | 52 |
| 1987 | 82 | 27 | 109 |
| 1988 | 22 | 13 | 35 |
| 1989 | 13 | 10 | 23 |
| 1990 | 26 | 12 | 38 |
| 1991 | 39 | 35 | 74 |
| 1992 | 34 | 2 | 36 |
| 1993 | 28 | 2 | 30 |
| 1994 | 64 | 9 | 73 |
| 1995 | 20 | 22 | 42 |
| 1996 | 26 | 26 | 26 |
| 1997 | 9 | 27 | 36 |
| 1998 | 4 | 19 | 23 |
| 1999 | 7 | 9 | 16 |
| 2000 | 16 | 35 | 51 |
| 2001 | 5 | 21 | 26 |
| 2002 | 6 | 24 | 30 |
| 2003 | 5 | 26 | 31 |
| 2004 | 16 | 16 | 32 |
| 2005 | 21 | 18 | 39 |
| 2006 | 2 | 39 | 41 |
| 2007 | 9 | 49 | 58 |
| 2008 | 13 | 43 | 56 |
| 2009 | 5 | 40 | 45 |
| 2010 | 10 | 52 | 62 |
| 2011 | 17 | 56 | 73 |
| 2012 | 10 | 40 | 50 |
| 2013 | 4 | 14 | 18 |
| 1540 |

- Trends of cases based on referral center
Discussion
Although the clinical history of hyperbaric medicine dates back to the 17th century, reports of the beneficial effects of increased oxygen pressure on wound healing and infection did not appear in the medical literature until the 1960s. The most recent report by the Hyperbaric Oxygen Therapy Committee of the Undersea and Hyperbaric Medical Society lists several indications for hyperbaric oxygen (HBO) therapy that are directly applicable to lower-extremity pathology. These include Clostridial Myonecrosis, Acute Traumatic Ischemia, enhancement of healing in problem wounds, necrotizing soft tissue infections, Refractory Osteomyelitis, compromised skin grafts and flaps, and thermal burns. Interestingly, there are relatively few controlled clinical trials in human subjects involving HBO for the treatment of these conditions. In fact, the majority of published reports on this topic consist of review articles, case reports, uncontrolled studies, and animal or in vitro studies.
Physiological Basis
When we normally breathe air at sea level pressure, most tissue needs for Oxygen are met from the Oxygen combined to Hb, which is 95 % saturated. 100 ml blood carries 19 ml O2 combined with Hb and 0.32 ml dissolved in plasma. At this pressure, if 100% O2 is inspired, O2 combined with Hb increases to a maximum of 20 ml and that dissolved in plasma to 2.09 ml. The higher pressure during hyperbaric oxygen treatment pushes more oxygen into dissolved from in plasma. The amount of O2 dissolved in plasma increases to 4.4 ml/dl at a pressure of 2 ATA and to 6.8 ml/dl at 3 ATA. This additional O2 in plasma is almost sufficient to meet tissue needs without contribution from O2 bound to hemoglobin and is responsible for most of the beneficial effects of this therapy [1,2,3,5].
The application of HBO to the therapy of various human diseases developed over a 300 year period. Like most of medicine, the basis of this application was and continues to be pragmatic in nature, and involves uncritical and untested judgments [4].
HBOT has been found beneficial not only by increasing the amount of dissolved oxygen but also by other mechanisms like:
Vasoconstriction leading to edema reduction
Neo vascularization
Bacteriostatic and bactericidal effect
Epithelialization
IAM Experience
The overall experience at IAM points out to the fact that use of HBOT is definitely beneficial for the UHMS indicated diseases. On analyzing the outcome, it was observed that improvement rate was 57%. However if the non followed up cases are added to this, rate is close to two third of the total cases. Though this cannot be proven statistically, being a retrograde study without control population, the results are definitely encouraging.
In the first two decades of the HBOT chamber mainly serving personnel or dependents were treated. However, in the overall data it is observed that the majority of the cases treated are civilians, accounting for 57.53%. This may be attributed due to loss of data.
Decade wise distribution
The analysis of trends based on the cases referred by service versus non-service hospital, it was found that in first two decades majority of the cases were referred from Service hospitals. In the last two decades the trend is reversed. It may be analyzed that this can be attributed to either increased awareness of HBOT in Non service hospitals due to proven benefits of HBOT or may be due to relative fall in the number of cases from service hospitals.
HBOT in Non Healing Wounds
Many studies have been done on effects of HBOT on lower extremity wounds and diabetic foot. Two randomized studies included a control group that did not receive HBO therapy. The controlled diabetic foot studies included an average of 28 subjects in the HBO therapy group (range 10-62) and an average of 16.2 subjects in the nonHBO control group (range 5-33). Additional randomized placebo-controlled clinical trials in large diabetic populations would further lend credence to the presumption that HBO therapy improves clinical outcomes. Given the relatively high cost of this treatment modality, perhaps a more acute awareness of the medical literature would reduce the economic burden that HBO therapy imposes on care providers that are financially at risk [5]. HBOT, in conjunction with an aggressive multidisciplinary therapeutic protocol, is effective in decreasing major amputations in diabetic patients with severe prevalently ischemic foot ulcers [6].
The total cases treated at IAM for which records are available are 1540 over past four decades. The commonest disability treated was Chronic Non Healing Wounds. (23.51%). 38.3% of Non Healing wounds were Diabetic foot. Outcome of chronic wounds is shown in Table 6. This outcome is very closely comparable with other studies.
| Service Hospital | Non-Service Hospital | Total | ||
|---|---|---|---|---|
| Decade 1 | 226 | 31 | 257 | |
| Decade 2 | 302 | 153 | 455 | |
| Decade 3 | 162 | 218 | 354 | |
| Decade 4 | 107 | 367 | 474 | |
| Outcome | Cases | % age |
|---|---|---|
| Died | 1 | 0.28 |
| Improved | 212 | 58.56 |
| Interrupted | 12 | 3.31 |
| No Follow Up | 135 | 37.29 |
| Not Improved | 2 | 0.55 |
| Total | 362 | 100.00 |
Ninety-four patients with Wagner grade 2, 3, or 4 ulcers, which had been present for >3 months, were studied [8]. In the intention-to-treat analysis, complete healing of the index ulcer was achieved in 37 patients at 1-year of follow-up: 25/ 48 (52%) in the HBOT group. At IAM chronic injuries were treated with at least 15 HBO2 sessions [10].
HBOT in Post Radiation Osteoradionecrosis (Mandibular Osteoradionecrosis)
Because of the mandible’s low vascularity and great density, the incidence of osteoradionecrosis is highest at this site. The mandible is often involved because head and neck cancers are common, and radiation therapy in these cancers is very effective. The presence of teeth in the jaws, as well as the functional and cosmetic importance of the mandible, means that osteoradionecrosis of the mandible most dramatically impacts on the patient’s quality of life.
Osteoradionecrosis (ORN) of the mandible is a potential complication of head and neck irradiation. It is defined as a nonhealing, nonseptic lesion of bone (Clayman, 1997). The underlying cause of ORN is believed to be progressive vascular occlusion and tissue hypoxia after radiation treatment (Porter & Brian, 1999). Three types of ORN have been described. Type 1 occurs when a patient receives radiation therapy within 21 days of tooth extraction or mandibulotomy. Type 2 is induced by trauma. It generally occurs 3-6 years after radiation therapy, usually following a tooth extraction. Type 3 occurs spontaneously 6 months to 2 years after radiation therapy and is associated with higher radiation doses, neutron beam therapy and brachytherapy (Cronje, 1998). Hyperbaric oxygen therapy is generally accepted as a treatment for patients who have ORN. The use of hyperbaric oxygen therapy is also proposed as a prophylactic treatment before dental work to prevent ORN in patients who have had irradiation of the head and neck.
The 1990 Consensus Paper of the National Cancer Institute on the Oral Complications of Cancer Therapies states: “The treatment of ORN with antibiotics and surgical debridement frequently fails, with progressive involvement of the remaining mandible. The keystone of the treatment of ORN is the provision of adequate tissue oxygenation in the damaged bone. This is best done by using Hyperbaric Oxygen Therapy (HBOT). In the event that dental extractions are required following radiation, meticulous surgical technique and antibiotic prophylaxis are necessary.
At IAM, 118 cases were treated with HBOT for post radiation injuries. Out of which 41 cases were of ORN. Majority of cases i.e. 37 cases were improved and 4 were not followed up.
HBOT in SNHL and Tinnitus
Idiopathic sudden sensorineural hearing loss (ISSHL) with or without tinnitus is common and presents a health problem with significant effect on quality of life. Hyperbaric oxygen therapy ( may improve oxygen supply to the inner ear and thereby result in an improvement in hearing and/or a reduction in the intensity of tinnitus 9.
At IAM, a total 155 (10.06%) cases of SNHL were treated, out of which 105 improved. In 07 cases, treatment was interrupted due to various reasons, 41 cases were not followed up and only one did not improve.
Conclusion
IAM experience over a span of four decades indicates that the addition of HBO therapy to conventional treatment modalities significantly improves the outcome of various indicated diseases, especially non healing wounds, SNHL and Post radiation injuries. It is found that there is association between outcome of the disease and number of sessions. It is recommended to maintain a data base programme at the department of HAP & HM for future analysis of such cases in a standardized and systematic manner.
References
- Introduction to the physical and physiological basis of hyperbaric therapy. In: Davis JC, Hunt TK, eds. Hyperbaric Oxygen Therapy. Kensington, MD: Undersea & Hyperbaric Medical Society; 1986. p. :11-24.
- [Google Scholar]
- Kuldeep Singh Hyperbaric Oxygen Therapy. Vol 14. Kensington, MD: Undersea & Hyperbaric Medical Society Medicine; 2004. The Association of Physicians of India
- [Google Scholar]
- Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer. A randomized study, Diabetes Care. 19
- [Google Scholar]
- Hyperbaric Oxygen Therapy and Mandibular Osteoradionecrosis: A Retrospective Study and Analysis of Treatment Outcomes. J Can Dent Assoc. 2001;67:384.
- [Google Scholar]
- Hyperbaric oxygen therapy facilitates healing of chronic foot Ulcers in Patients a diabetes. Diabetes Care. 2010;33(5):998-1003.
- [Google Scholar]
- Hyperbaric oxygen for idiopathic sudden sensorineural hearing loss and tinnitus. The Cochrane review Library.
- [Google Scholar]
- Hyperbaric oxygen therapy: types of injury and number of sessions – a review of 1507 cases In: UHM. Vol 35. 2008. p. :53-60.
- [Google Scholar]






